Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Blunt Trauma
BLUNT TRAUMA
Although
blunt chest trauma is more common, it is often diffi-cult to identify the
extent of the damage because the symptoms may be generalized and vague. In
addition, patients may not seek immediate medical attention, which may
complicate the problem.
Pathophysiology
Injuries
to the chest are often life-threatening and result in one or more of the
following pathologic mechanisms:
·
Hypoxemia from disruption of the
airway; injury to the lung parenchyma, rib cage, and respiratory musculature;
massive hemorrhage; collapsed lung; and pneumothorax
·
Hypovolemia from massive fluid loss
from the great vessels, cardiac rupture, or hemothorax
·
Cardiac failure from cardiac
tamponade, cardiac contusion, or increased intrathoracic pressure
These
mechanisms frequently result in impaired ventilation and perfusion leading to
ARF, hypovolemic shock, and death.
Assessment and Diagnostic Findings
Time
is critical in treating chest trauma. Therefore, it is essential to assess the
patient immediately to determine the following:
·
When the injury occurred
·
Mechanism of injury
·
Level of responsiveness
·
Specific injuries
·
Estimated blood loss
·
Recent drug or alcohol use
·
Prehospital treatment
The
initial assessment of thoracic injuries includes assessment of the patient for
airway obstruction, tension pneumothorax, open pneumothorax, massive
hemothorax, flail chest, and cardiac tamponade. These injuries are
life-threatening and need imme-diate treatment. Secondary assessment would
include simple pneumothorax, hemothorax, pulmonary contusion, traumatic aortic
rupture, tracheobronchial disruption, esophageal perfora-tion, traumatic
diaphragmatic injury, and penetrating wounds to the mediastinum (Owens,
Chaudry, Eggerstedt & Smith, 2000). Although listed as secondary, these
injuries may be life-threatening as well depending upon the circumstances.
The
physical examination includes inspection of the airway, thorax, neck veins, and
breathing difficulty. Specifics include as-sessing the rate and depth of
breathing for abnormalities, such as stridor, cyanosis, nasal flaring, use of
accessory muscles, drooling, and overt trauma to the face, mouth, or neck. The
chest should be assessed for symmetric movement, symmetry of breath sounds,
open chest wounds, entrance or exit wounds, impaled objects, tracheal shift,
distended neck veins, subcutaneous emphysema, and paradoxical chest wall
motion. In addition, the chest wall should be assessed for bruising, petechiae,
lacerations, and burns. The vital signs and skin color are assessed for signs
of shock. The thorax is palpated for tenderness and crepitus; the position of
the trachea is also assessed.
The
initial diagnostic workup includes a chest x-ray, CT scan, complete blood
count, clotting studies, type and cross-match, electrolytes, oxygen saturation,
arterial blood gas analysis, and ECG. The patient is completely undressed to
avoid missing ad-ditional injuries that can complicate care. Many patients with
in-juries involving the chest have associated head and abdominal injuries that
require attention. Ongoing assessment is essential to monitor the patient’s
response to treatment and to detect early signs of clinical deterioration.
Medical Management
The
goals of treatment are to evaluate the patient’s condition and to initiate
aggressive resuscitation. An airway is immediately es-tablished with oxygen
support and, in some cases, intubation and ventilatory support. Re-establishing
fluid volume and negative in-trapleural pressure and draining intrapleural
fluid and blood are essential.
The
potential for massive blood loss and exsanguination with blunt or penetrating
chest injuries is high because of injury to the great blood vessels. Many
patients die at the scene or are in shock by the time help arrives. Agitation
and irrational and combative behavior are signs of decreased oxygen delivery to
the cerebral cortex. Strategies to restore and maintain cardiopulmonary
func-tion include ensuring an adequate airway and ventilation, stabi-lizing and
re-establishing chest wall integrity, occluding any opening into the chest
(open pneumothorax), and draining or re-moving any air or fluid from the thorax
to relieve pneumothorax, hemothorax, or cardiac tamponade. Hypovolemia and low
car-diac output must be corrected. Many of these treatment efforts, along with
the control of hemorrhage, are usually carried out si-multaneously at the scene
of the injury or in the emergency de-partment. Depending on the success of
efforts to control the hemorrhage in the emergency department, the patient may
be taken immediately to the operating room. Principles of manage-ment are
essentially those pertaining to care of the postoperative thoracic patient.
Sternal and Rib Fractures
Sternal
fractures are most common in motor vehicle crashes with a direct blow to the
sternum via the steering wheel and are most common in women, patients over age
50, and those using shoul-der restraints (Owens, Chaudry, Eggerstedt &
Smith, 2000).
Rib
fractures are the most common type of chest trauma, oc-curring in more than 60%
of patients admitted with blunt chest injury. Most rib fractures are benign and
are treated conserva-tively. Fractures of the first three ribs are rare but can
result in a high mortality rate because they are associated with laceration of
the subclavian artery or vein. The fifth through ninth ribs are the most common
sites of fractures. Fractures of the lower ribs are as-sociated with injury to
the spleen and liver, which may be lacer-ated by fragmented sections of the
rib.
CLINICAL MANIFESTATIONS
The
patient with sternal fractures has anterior chest pain, over-lying tenderness,
ecchymosis, crepitus, swelling, and the poten-tial of a chest wall deformity.
For the patient with rib fractures, clinical manifestations are similar: severe
pain, point tenderness,and muscle spasm over the area of the fracture, which is
aggra-vated by coughing, deep breathing, and movement. The area around the
fracture may be bruised. To reduce the pain, the patient splints the chest by
breathing in a shallow manner and avoids sighs, deep breaths, coughing, and
movement. This reluctance to move or breathe deeply results in diminished
ventilation, collapse of unaerated alveoli (atelectasis), pneumonitis, and
hypoxemia. Respiratory insufficiency and failure can be the outcomes of such a
cycle.
ASSESSMENT AND DIAGNOSTIC FINDINGS
The
patient with a sternal fracture must be closely evaluated for underlying
cardiac injuries. A crackling, grating sound in the tho-rax (subcutaneous
crepitus) may be detected with auscultation. The diagnostic workup may include
a chest x-ray, rib films of a specific area, ECG, continuous pulse oximetry,
and arterial blood gas analysis.
MEDICAL MANAGEMENT
Medical
management of the patient with a sternal fracture is di-rected toward
controlling pain, avoiding excessive activity, and treating any associated
injuries. Surgical fixation is rarely neces-sary unless fragments are grossly
displaced and pose a potential for further injury.
The
goals of treatment for rib fractures are to control pain and to detect and
treat the injury. Sedation is used to relieve pain and to allow deep breathing
and coughing. Care must be taken to avoid oversedation and suppression of the
respiratory drive. Alter-native strategies to relieve pain include an
intercostal nerve block and ice over the fracture site; a chest binder may
decrease pain on movement. Usually the pain abates in 5 to 7 days, and
discom-fort can be controlled with epidural analgesia, patient-controlled
analgesia, or nonopioid analgesia. Most rib fractures heal in 3 to 6 weeks. The
patient is monitored closely for signs and symptoms of associated injuries.
Flail Chest
Flail
chest is frequently a complication of blunt chest trauma from a steering wheel
injury. It usually occurs when three or more adjacent ribs (multiple contiguous
ribs) are fractured at two or more sites, resulting in free-floating rib
segments. It may also result as a combination fracture of ribs and costal
cartilages or ster-num (Owens, Chaudry, Eggerstedt & Smith, 2000). As a
result, the chest wall loses stability and there is subsequent respiratory
impairment and usually severe respiratory distress.
PATHOPHYSIOLOGY
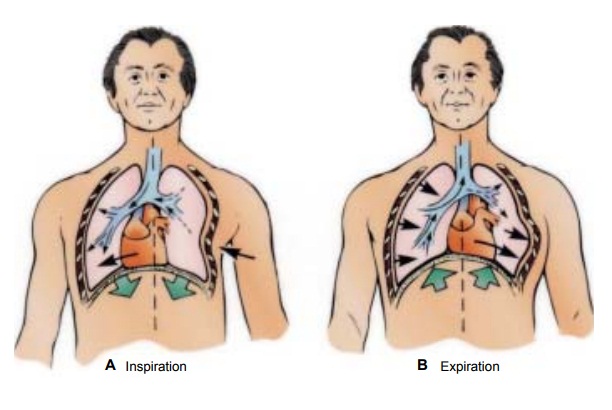
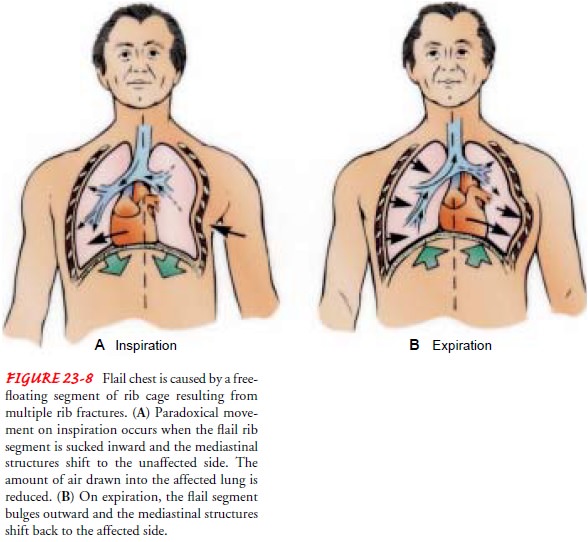
During
inspiration, as the chest expands, the detached part of the rib segment (flail
segment) moves in a paradoxical manner (pen-delluft movement) in that it is
pulled inward during inspiration, reducing the amount of air that can be drawn
into the lungs. On expiration, because the intrathoracic pressure exceeds
atmospheric pressure, the flail segment bulges outward, impairing the patient’s
ability to exhale. The mediastinum then shifts back to the affected side (Fig.
23-8). This paradoxical action results in increased dead space, a reduction in
alveolar ventilation, and decreased compli-ance. Retained airway secretions and
atelectasis frequently ac-company flail chest. The patient has hypoxemia, and
if gas exchange is greatly compromised, respiratory acidosis develops as a
result of CO2 retention. Hypotension, inadequate
tissue perfu-sion, and metabolic acidosis often follow as the paradoxical
mo-tion of the mediastinum decreases cardiac output.
MEDICAL MANAGEMENT
As
with rib fracture, treatment of flail chest is usually supportive. Management
includes providing ventilatory support, clearing se-cretions from the lungs,
and controlling pain. The specific man-agement depends on the degree of
respiratory dysfunction. If only a small segment of the chest is involved, the
objectives are to clear the airway through positioning, coughing, deep
breathing, and suctioning to aid in the expansion of the lung, and to relieve
pain by intercostal nerve blocks, high thoracic epidural blocks, or cau-tious
use of intravenous opioids.
For
mild to moderate flail chest injuries, the underlying pul-monary contusion is
treated by monitoring fluid intake and ap-propriate fluid replacement, while at
the same time relieving chest pain. Pulmonary physiotherapy focusing on lung
volume expan-sion and secretion management techniques are performed. The
patient is closely monitored for further respiratory compromise.
When a severe flail chest injury is encountered, endotracheal intubation and mechanical ventilation are required to provide in-ternal pneumatic stabilization of the flail chest and to correct ab-normalities in gas exchange.
This helps to treat the underlying pulmonary
contusion, serves to stabilize the thoracic cage to allow the fractures to
heal, and improves alveolar ventilation and in-trathoracic volume by decreasing
the work of breathing. This treatment modality requires endotracheal intubation
and venti-lator support. Differing modes of ventilation are used depending on
the patient’s underlying disease and specific needs.
In
rare circumstances, surgery may be required to more quickly stabilize the flail
segment. This may be used in the patient who is difficult to ventilate or the
high-risk patient with under-lying lung disease who may be difficult to wean
from mechanical ventilation.
Regardless
of the type of treatment, the patient is carefully monitored by serial chest
x-rays, arterial blood gas analysis, pulse oximetry, and bedside pulmonary
function monitoring. Pain management is key to successful treatment.
Patient-controlled analgesia, intercostal nerve blocks, epidural analgesia, and
intra-pleural administration of opioids may be used to control tho-racic pain.
Pulmonary Contusion
Pulmonary
contusion is observed in about 20% of adult patients with multiple traumatic
injuries and in a higher percentage of children due to increased compliance of
the chest wall. It is de-fined as damage to the lung tissues resulting in
hemorrhage and localized edema. It is associated with chest trauma when there
is rapid compression and decompression to the chest wall (ie, blunt trauma). It
may not be evident initially on examination but will develop in the
posttraumatic period.
PATHOPHYSIOLOGY
The
primary pathologic defect is an abnormal accumulation of fluid in the
interstitial and intra-alveolar spaces. It is thought that injury to the lung
parenchyma and its capillary network results in a leakage of serum protein and
plasma. The leaking serum protein exerts an osmotic pressure that enhances loss
of fluid from the cap-illaries. Blood, edema, and cellular debris (from
cellular response to injury) enter the lung and accumulate in the bronchioles
and alveolar surface, where they interfere with gas exchange. An in-crease in
pulmonary vascular resistance and pulmonary artery pressure occurs. The patient
has hypoxemia and carbon dioxide retention. Occasionally, a contused lung
occurs on the other side of the point of body impact; this is called a
contrecoup contusion.
CLINICAL MANIFESTATIONS
Pulmonary
contusion may be mild, moderate, or severe. The clinical manifestations vary
from tachypnea, tachycardia, pleu-ritic chest pain, hypoxemia, and blood-tinged
secretions to more severe tachypnea, tachycardia, crackles, frank bleeding,
severe hy-poxemia, and respiratory acidosis. Changes in sensorium, in-cluding increased
agitation or combative irrational behavior, may be signs of hypoxemia.
In
addition, the patient with moderate pulmonary contusion has a large amount of
mucus, serum, and frank blood in the tra-cheobronchial tree; the patient often
has a constant cough but cannot clear the secretions. A patient with severe
pulmonary con-tusion has the signs and symptoms of ARDS; these may include
central cyanosis, agitation, combativeness, and productive cough with frothy,
bloody secretions.
ASSESSMENT AND DIAGNOSTIC FINDINGS
The
efficiency of gas exchange is determined by pulse oximetry and arterial blood
gas measurements. Pulse oximetry is also used to measure oxygen saturation
continuously. The chest x-ray may show pulmonary infiltration. The initial
chest x-ray may show no changes; in fact, changes may not appear for 1 or 2
days after the injury.
MEDICAL MANAGEMENT
Treatment
priorities include maintaining the airway, providing adequate oxygenation, and
controlling pain. In mild pulmonary contusion, adequate hydration via
intravenous fluids and oral in-take is important to mobilize secretions.
However, fluid intake must be closely monitored to avoid hypervolemia. Volume
ex-pansion techniques, postural drainage, physiotherapy including coughing, and
endotracheal suctioning are used to remove the se-cretions. Pain is managed by
intercostal nerve blocks or by opi-oids via patient-controlled analgesia or
other methods. Usually, antimicrobial therapy is administered because the
damaged lung is susceptible to infection. Supplemental oxygen is usually given
by mask or cannula for 24 to 36 hours.
The
patient with moderate pulmonary contusion may require bronchoscopy to remove
secretions; intubation and mechanical ventilation with PEEP may also be
necessary to maintain the pressure and keep the lungs inflated. Diuretics may
be given to reduce edema. A nasogastric tube is inserted to relieve
gastro-intestinal distention.
The
patient with severe contusion may develop respiratory failure and may require
aggressive treatment with endotracheal intubation and ventilatory support,
diuretics, and fluid restric-tion. Colloids and crystalloid solutions may be
used to treat hypovolemia.
Antimicrobial
medications may be prescribed for the treat-ment of pulmonary infection. This
is a common complication of pulmonary contusion (especially pneumonia in the
contused seg-ment), because the fluid and blood that extravasates into the
alve-olar and interstitial spaces serve as an excellent culture medium.
Related Topics