Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Pneumonia
PNEUMONIA
Pneumonia
is an inflammation of the lung parenchyma that is caused by a microbial agent.
“Pneumonitis” is a more general term that describes an inflammatory process in
the lung tissue that may predispose a patient to or place a patient at risk for
microbial in-vasion. Pneumonia is the most common cause of death from
in-fectious diseases in the United States. It is the seventh leading cause of death
in the United States for all ages and both genders, result-ing in almost 70,000
deaths per year. In persons 65 years of age and older, it is the fifth leading
cause of death (National Center for Health Statistics, 2000; Minino &
Smith, 2001). It is treated extensively on both an inpatient and outpatient
basis.
Bacteria
commonly enter the lower airway but do not cause pneumonia in the presence of
an intact host defense mechanism. When pneumonia does occur, it is caused by
various microorgan-isms, including bacteria, mycobacteria, chlamydiae,
mycoplasma, fungi, parasites, and viruses. Several systems are used to classify
pneumonias. Classically, pneumonia has been categorized into one of four
categories: bacterial or typical, atypical, anaerobic/ cavitary, and
opportunistic. However, there is overlap in the micro-organisms thought to be
responsible for typical and atypical pneumonias. A more widely used
classification scheme categorizes the major pneumonias as community-acquired
pneumonia, hospital-acquired pneumonia, pneumonia in the immunocompromised
host, and aspiration pneumonia (Table 23-1). There is overlap in how specific
pneumonias are classified because they may occur in differing settings.
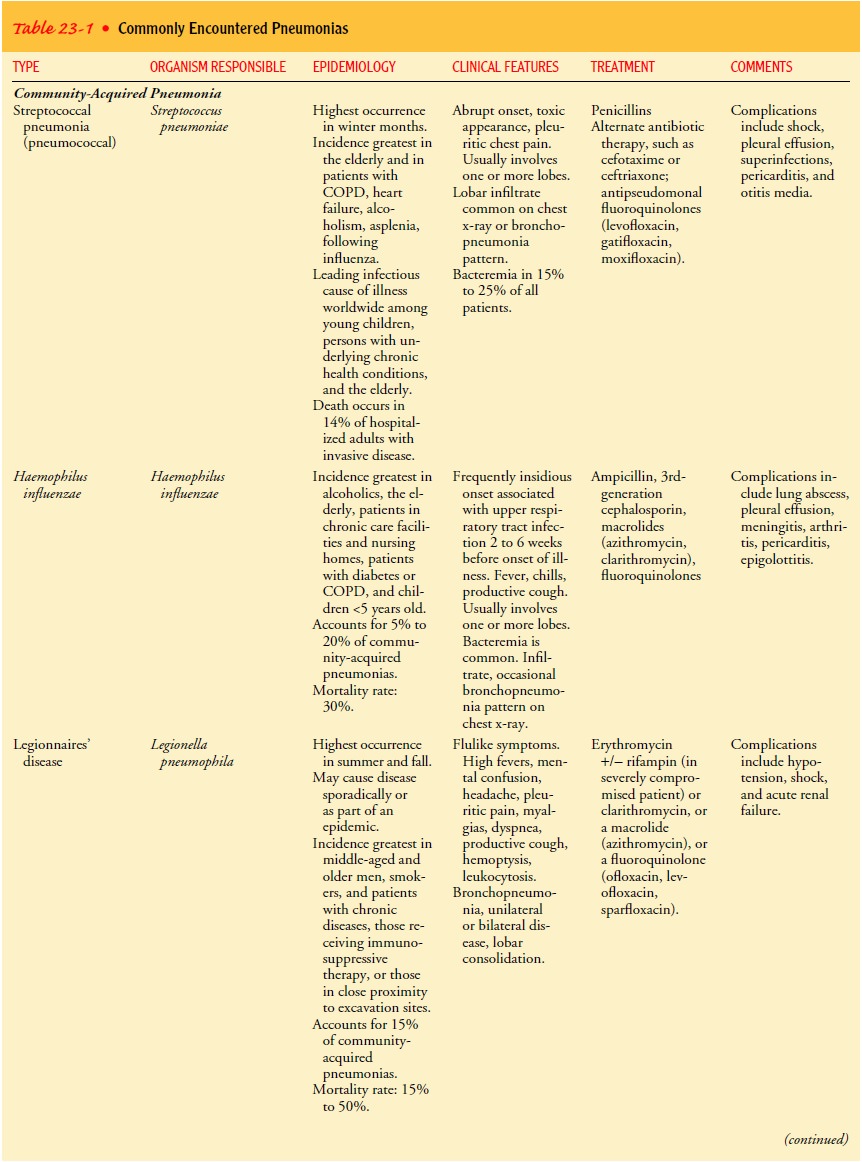
Community-acquired
pneumonia (CAP) occurs either in the community setting or within the first 48
hours of hospitalization or institutionalization. The need for hospitalization
for CAP de-pends on the severity of the pneumonia. The agents that most
fre-quently cause CAP requiring hospitalization are S. pneumoniae,H. influenzae, Legionella, Pseudomonas aeruginosa, and
other gram-negative rods. The specific etiologic agent of CAP is identified in
about 50% of the cases. The absence of a responsible caregiver in the home may
be another indication for hospitalization. More than 5.5 million people develop
CAP and as many as 1.1 million require hospitalization each year (Centers for
Disease Control and Prevention [CDC], 1997; Marston, Plouffe, File et al.,
1997).
Pneumonia
caused by S. pneumoniae
(pneumococcus) is the most common CAP in people younger than 60 without
comor-bidity and in those older than 60 with comorbidity. It is most prevalent
during the winter and spring, when upper respiratory tract infections are most
frequent. S. pneumoniae is a
gram-positive, capsulated, nonmotile coccus that resides naturally in the upper
respiratory tract. The organism colonizes the upper respiratory tract and can
cause the following types of illnesses: disseminated invasive infections,
pneumonia and other lower respiratory tract infections, and upper respiratory
tract infections, including oti-tis media and sinusitis (CDC, 1998). It may
occur as a lobar or bronchopneumonic form in patients of any age and may follow
a recent respiratory illness.
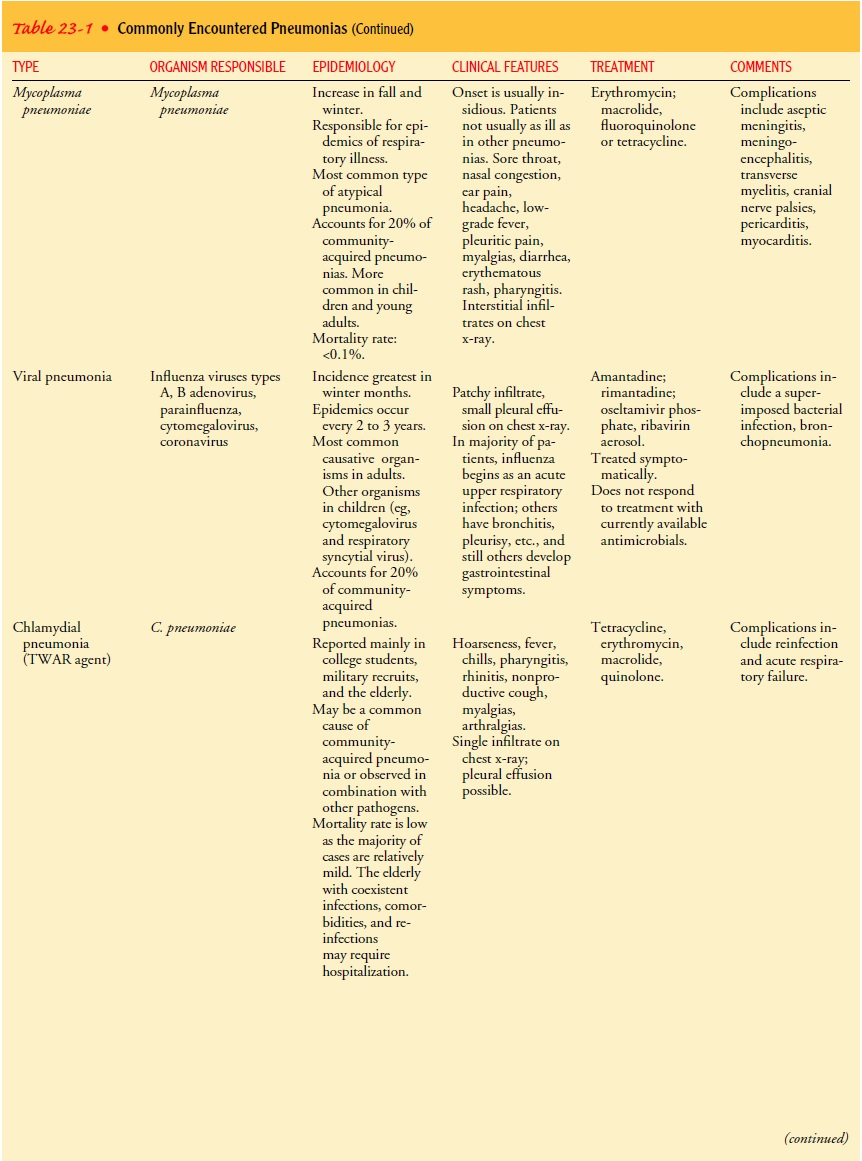
Mycoplasma
pneumonia, another type of CAP, occurs most often in older children and young
adults and is spread by infected respiratory droplets through person-to-person
contact. Patients can be tested for mycoplasma antibodies. The inflammatory
in-filtrate is primarily interstitial rather than alveolar. It spreads
throughout the entire respiratory tract, including the bronchioles, and has the
characteristics of a bronchopneumonia. Earache and bullous myringitis are
common. Impaired ventilation and diffu-sion may occur.
H. influenzae is
another cause of CAP. It frequently affects el-derly people or those with
comorbid illnesses (eg, chronic obstruc-tive pulmonary disease [COPD],
alcoholism, diabetes mellitus). The presentation of this pneumonia is
indistinguishable from that of other forms of bacterial CAP. The presentation
may be subacute, with cough or low-grade fever for weeks before diagnosis.
Chest x-rays may reveal multilobar, patchy bronchopneumonia or areas of consolidation (tissue that solidifies
as a result of collapsed alve-oli or pneumonia).
Viruses are the most common cause of pneumonia in infants and children but are relatively uncommon causes of CAP in adults. The chief causes of viral pneumonia in the immuno-competent adult are influenza viruses types A and B, adenovirus, parainfluenza virus, coronavirus, and varicella-zoster virus. In immunocompromised adults, cytomegalovirus is the most com-mon viral pathogen, followed by herpes simplex virus, adeno-virus, and respiratory syncytial virus. The acute stage of a viral respiratory infection occurs within the ciliated cells of the airways. This is followed by infiltration of the tracheobronchial tree. With pneumonia, the inflammatory process extends into the alveolar area, resulting in edema and exudation. The clinical signs and symptoms of a viral pneumonia are often difficult to distinguish from those of a bacterial pneumonia.
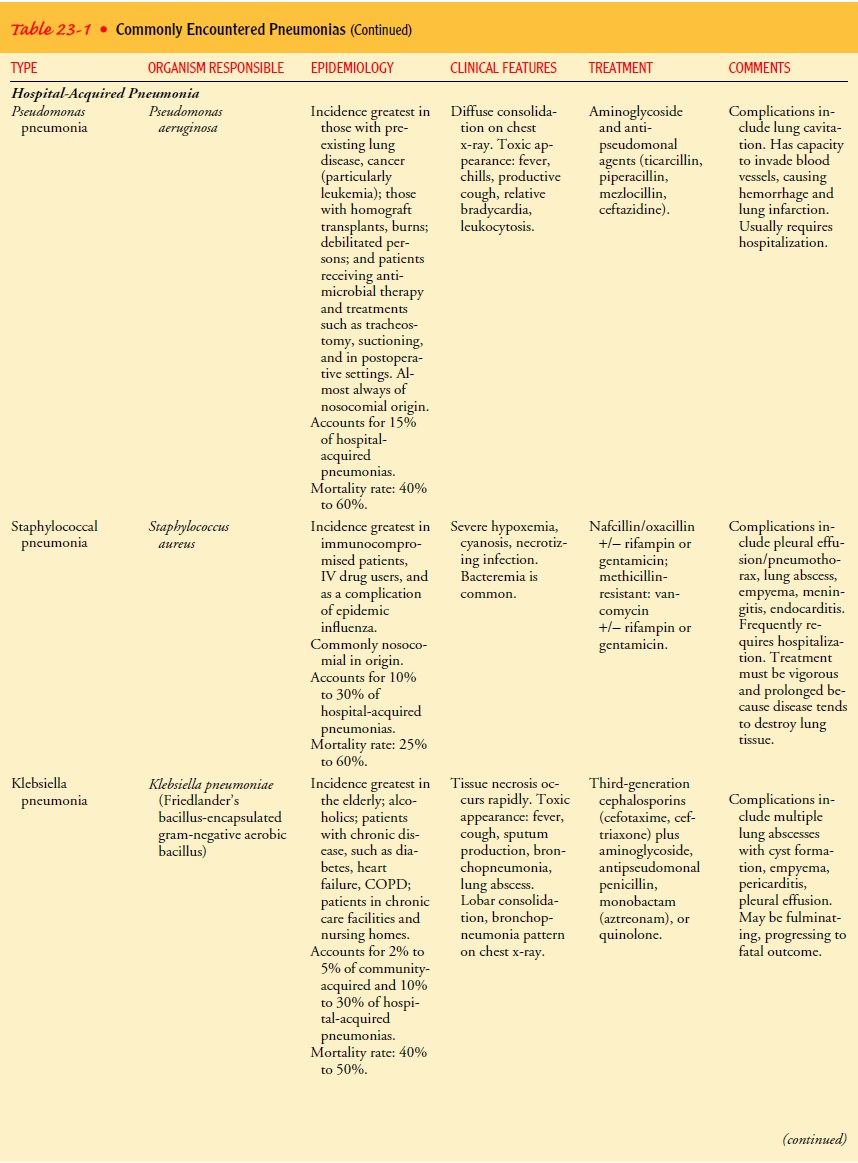
Hospital-acquired
pneumonia (HAP), also known as nosoco-mial
pneumonia, is defined as the onset of pneumonia symptomsmore than 48 hours
after admission to the hospital. HAP ac-counts for approximately 15% of
hospital-acquired infections but is the most lethal nosocomial infection. It is
estimated to occur in 0.5% to 1% of all hospitalized patients and in 15% to 20%
of intensive care patients. Ventilator-associated pneumonia can be considered a
type of nosocomial pneumonia that is associated with endotracheal intubation
and mechanical ventilation.
The common organisms responsible for HAP
include the pathogens Enterobacter
species, Escherichia coli, Klebsiella
species, Proteus, Serratia marcescens, P.
aeruginosa, and methicillin-sensitiveor methicillin-resistant Staphylococcus aureus. These respiratory
infections occur when at least one of three conditions exists: host defenses
are impaired, an inoculum of organisms reaches the pa-tient’s lower respiratory
tract and overwhelms the host’s defenses, or a highly virulentorganism is
present. Certain illnesses may pre-dispose a patient to HAP because of impaired
host defenses. Examples include severe acute or chronic illness, a variety of
co-morbid conditions, coma, malnutrition, prolonged hospitalization,
hypotension, and metabolic disorders. The hospitalized patient is also exposed
to potential bacteria from other sources (eg, respiratory therapy devices and
equipment, transmission of pathogens by the hands of health care personnel).
Numerous intervention-related factors also may play a role in the development
of HAP (eg, therapeutic agents leading to central nervous system depres-sion
with decreased ventilation, impaired removal of secretions, or potential
aspiration; prolonged or complicated thoraco-abdominal procedures, which may
impair mucociliary function and cellular host defenses; endotracheal
intubation; prolonged or inappropriate use of antibiotics; use of nasogastric
tubes). In addi-tion, immunocompromised patients are at particular risk. HAP is
associated with a high mortality rate, in part because of the vir-ulence of the
organisms, their resistance to antibiotics, and the patient’s underlying
disorder.
Dominant
pathogens for HAP are gram-negative bacilli (P. aeruginosa and Enterobacteriaceae/Klebsiella
species, Enter-obacter, Proteus, Serratia)
and S. aureus. Pseudomonal pneumo-nia
occurs in patients who are debilitated, those with altered mental status, and
those with prolonged intubation or with tra-cheostomies. Staphylococcal
pneumonia can occur through in-halation of the organism or spread through the
hematogenous route. It is often accompanied by bacteremia and positive blood
cultures. Although responsible for less than 10% of cases of CAP, staphylococcal
pneumonia may be responsible for more than 30% of cases of HAP. Its mortality
rate is high. Specific strains of staphylococci are resistant to all available
antimicrobials except vancomycin. These strains of S. aureus are referred to as methicillin-resistant S. aureus (MRSA). Overuse and misuse of
antimicrobial agents are major risk factors for the emergence of these
resistant pathogens. Because MRSA is highly virulent, steps must be taken to
prevent the spread of this organism. The patient with MRSA should be isolated
in a private room, and contact precautions (gown, mask, glove, and
antibacterial soap) are used. The num-ber of people in contact with the patient
should be minimized, and appropriate precautions must be taken when
transporting the patient within or between facilities.
The
usual presentation of an HAP is a new pulmonary infil-trate on chest x-ray
combined with evidence of infection such as fever, respiratory symptoms,
purulent sputum, and/or leuko-cytosis. Pneumonias from Klebsiella or other gram-negative organ-isms (E. coli, Proteus, Serratia) are characterized by destruction of
lung structure and alveolar walls, consolidation, and bacteremia. Elderly
patients and those with alcoholism, chronic lung disease, or diabetes are at
particular risk. A sudden onset of cough is a common presentation, and
blood-tinged sputum may be present. In the debilitated or dehydrated patient,
sputum production may be minimal or absent. Pleural effusions, high fevers, and
tachy-cardia are often observed. Even with treatment, the mortality rate
remains high.
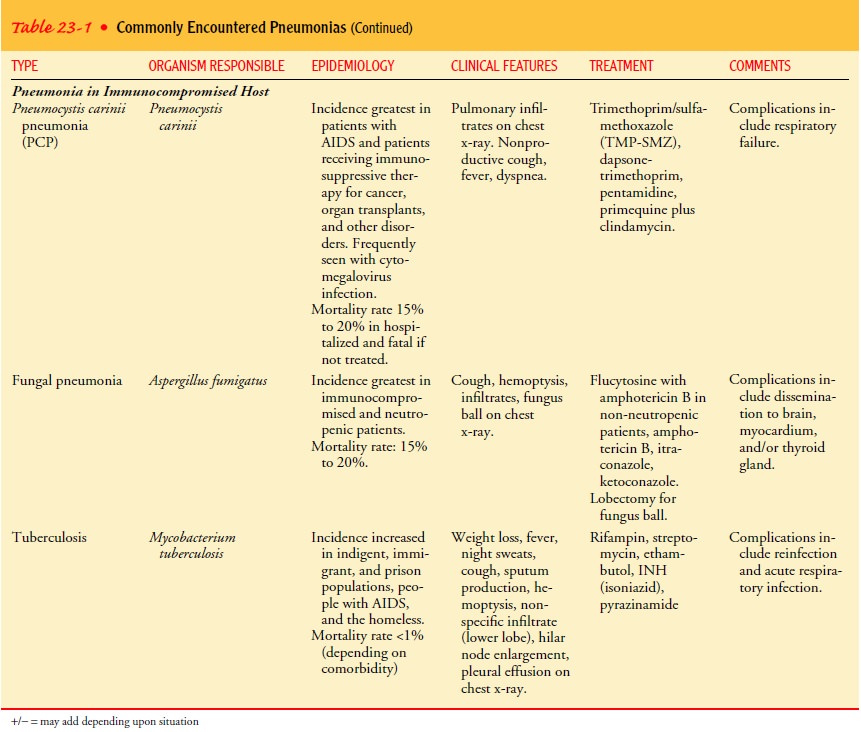
Pneumonia
in the immunocompromised host is seen with greater frequency because
immunocompromised hosts represent a growing portion of the patient population.
Examples of pneu-monia in the immunocompromised host are Pneumocystis carinii pneumonia (PCP), fungal pneumonias, and
mycobacterium tuberculosis. These types of pneumonia may also occur in the
immunocompetent person and in different settings, but these are less common.
Immunocompromised states occur with the use of corticosteroids or other
immunosuppressive agents, chemother-apy, nutritional depletion, use of
broad-spectrum antimicrobial agents, AIDS, genetic immune disorders, and
long-term advanced life-support technology (mechanical ventilation). Patients
with compromised immune systems commonly acquire pneumonia from organisms of
low virulence. In addition, increasing numbers of patients with impaired
defenses develop HAP from gram-negative bacilli (Klebsiella, Pseudomonas, E. coli, Enterobacteri-aceae, Proteus, Serratia).
Pneumonia
in the compromised host may be caused by the or-ganisms also observed in CAP or
HAP (S. pneumoniae, S. aureus,
influenzae,
P. aeruginosa, M. tuberculosis). PCP is rarely ob-served in the
immunocompetent host and is often an initial AIDS-defining complication.
Whether the patient is immuno-compromised or immunocompetent, the clinical
presentation of pneumonia is similar. PCP has a subtle onset with progressive
dyspnea, fever, and a nonproductive cough.
Aspiration
pneumonia refers to the pulmonary consequences resulting from the entry of
endogenous or exogenous substances into the lower airway. The most common form
of aspiration pneumonia is bacterial infection from aspiration of bacteria that
normally reside in the upper airways. Aspiration pneumonia may occur in the
community or hospital setting; common pathogens are S. pneumoniae, H. influenzae, and S. aureus. Other substances may be aspirated into the lung, such as
gastric contents, exogenous chemical contents, or irritating gases. This type
of aspiration or ingestion may impair the lung defenses, cause inflammatory
changes, and lead to bacterial growth and a resulting pneumonia.
Pathophysiology
Upper
airway characteristics normally prevent potentially infec-tious particles from
reaching the normally sterile lower respira-tory tract. Thus, patients with
pneumonia caused by infectious agents often have an acute or chronic underlying
disease that im-pairs host defenses. Pneumonia arises from normally present
flora in a patient whose resistance has been altered, or it results from
aspiration of flora present in the oropharynx. It may also result from
bloodborne organisms that enter the pulmonary circulation and are trapped in
the pulmonary capillary bed, becoming a po-tential source of pneumonia.
Pneumonia
often affects both ventilation and diffusion. An inflammatory reaction can
occur in the alveoli, producing an ex-udate that interferes with the diffusion
of oxygen and carbon dioxide. White blood cells, mostly neutrophils, also
migrate into the alveoli and fill the normally air-containing spaces. Areas of
the lung are not adequately ventilated because of secretions and mucosal edema
that cause partial occlusion of the bronchi or alveoli, with a resultant
decrease in alveolar oxygen tension. Bron-chospasm may also occur in patients
with reactive airway disease. Because of hypoventilation, a
ventilation–perfusion mismatch occurs in the affected area of the lung. Venous
blood entering the pulmonary circulation passes through the underventilated
area and exits to the left side of the heart poorly oxygenated. The mix-ing of
oxygenated and unoxygenated or poorly oxygenated blood eventually results in
arterial hypoxemia.
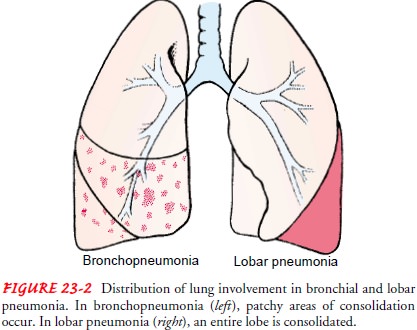
If
a substantial portion of one or more lobes is involved, the disease is referred
to as “lobar pneumonia.” The term “bron-chopneumonia” is used to describe
pneumonia that is distributed in a patchy fashion, having originated in one or
more localized areas within the bronchi and extending to the adjacent
sur-rounding lung parenchyma. Bronchopneumonia is more com-mon than lobar
pneumonia (Fig. 23-2).
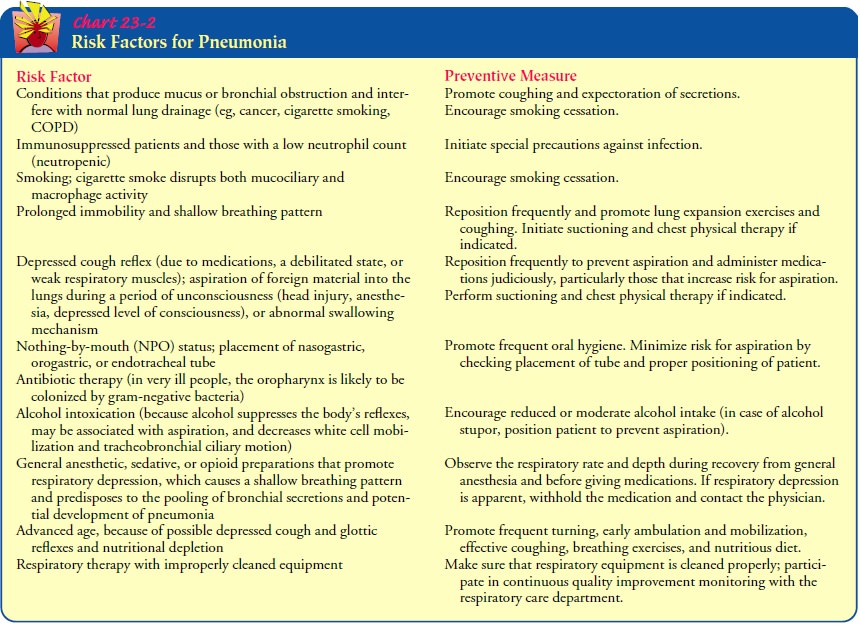
Risk Factors
Being
knowledgeable about the factors and circumstances that commonly predispose a
person to pneumonia will aid in identi-fying patients at high risk for this
disorder (Chart 23-2).
Increasing
numbers of patients who have compromised de-fenses against infections are
susceptible to pneumonia. Some types of pneumonia, such as those caused by
viral infections, occur in previously healthy people and often follow a viral
illness.
Pneumonia
is common with certain underlying disorders such as heart failure, diabetes,
alcoholism, COPD, and AIDS. Certain diseases also have been associated with
specific pathogens. For ex-ample, staphylococcal pneumonia has been noted after
epidemics of influenza, and patients with COPD are at increased risk for
de-veloping pneumonia caused by pneumococci or H. influenzae. In addition, cystic fibrosis is associated with
respiratory infection caused by pseudomonal and staphylococcal organisms, and
PCP has been associated with AIDS. Pneumonias occurring in hospitalized
pa-tients often involve organisms not usually found in CAP, including enteric
gram-negative bacilli and S. aureus.
The
CDC has identified three specific strategies for preventing HAP: (1) staff
education and infection surveillance, (2) interrup-tion of transmission of
microorganisms through person-to-person transmission and equipment
transmission, and (3) modification of host risk of infection (CDC, 1997).
Providing anticipatory and preventive care is an important nursing measure.
To
reduce or prevent serious complications of CAP in high-risk groups, vaccination
against pneumococcal infection is ad-vised for the following:
·
People 65 years of age or older
·
Immunocompetent people who are at
increased risk for ill-ness and death associated with pneumococcal disease
because of chronic illness (eg, cardiovascular, pulmonary, diabetes mellitus,
chronic liver disease)
·
People with functional or anatomic
asplenia
·
People living in environments or
social settings in which the risk of disease is high
·
Immunocompromised people at high
risk for infection (CDC, 1998)
The
vaccine provides specific prevention against pneumo-coccal pneumonia and other
infections caused by this organism (otitis media, other upper respiratory tract
infections). Vaccines should be avoided in the first trimester of pregnancy.
Clinical Manifestations
Pneumonia
varies in its signs and symptoms depending on the organism and the patient’s
underlying disease. However, regard-less of the type of pneumonia (CAP, HAP,
immunocompro-mised host, aspiration), a specific type of pneumonia cannot be
diagnosed by clinical manifestations alone. For example, the pa-tient with
streptococcal (pneumococcal) pneumonia usually has a sudden onset of shaking
chills, rapidly rising fever (38.5° to 40.5°C [101° to 105°F]), and
pleuritic chest pain that is aggra-vated by deep breathing and coughing. The
patient is severely ill, with marked tachypnea (25 to 45 breaths/min), accompanied
by other signs of respiratory distress (eg, shortness of breath, use of
accessory muscles in respiration). The pulse is rapid and bound-ing, and it
usually increases about 10 beats/min for every degree of temperature (Celsius)
elevation. A relative bradycardia for the amount of fever may suggest viral
infection, mycoplasma infec-tion, or infection with a Legionella organism.
Some
patients exhibit an upper respiratory tract infection (nasal congestion, sore
throat), and the onset of symptoms of pneumonia is gradual and nonspecific. The
predominant symp-toms may be headache, low-grade fever, pleuritic pain,
myalgia, rash, and pharyngitis. After a few days, mucoid or mucopurulent sputum
is expectorated. In severe pneumonia, the cheeks are flushed and the lips and
nailbeds demonstrate central cyanosis (a late sign of poor oxygenation
[hypoxemia]).
Typically,
the patient has orthopnea (shortness
of breath when reclining); he or she prefers to be propped up in bed lean-ing
forward (orthopneic position), trying to achieve adequate gas exchange without
coughing or breathing deeply. Appetite is poor, and the patient is diaphoretic
and tires easily. Sputum is often pu-rulent; this is not a reliable indicator
of the etiologic agent. Rusty, blood-tinged sputum may be expectorated with
streptococcal (pneumococcal), staphylococcal, and Klebsiella pneumonia.
Signs
and symptoms of pneumonia may also depend on under-lying conditions. Differing
signs occur in patients with other con-ditions, such as cancer, or in those who
are undergoing treatment with immunosuppressants, which lower the resistance to
infection. Such patients have fever, crackles, and physical findings that
indi-cate consolidation of lung tissue, including increased tactile fremi-tus
(vocal vibration detected on palpation), percussion dullness, bronchial breath
sounds, egophony (when auscultated, the spoken “E” becomes a loud,
nasal-sounding “A”), and whispered pectoril-oquy (whispered sounds are easily
auscultated through the chest wall). These changes occur because sound is
transmitted better through solid or dense tissue (consolidation) than through
normal air-filled tissue;.
Purulent
sputum or slight changes in respiratory symptoms may be the only sign of
pneumonia in patients with COPD. It may be difficult to determine whether an
increase in symptoms is an exacerbation of the underlying disease process or an
addi-tional infectious process.
Assessment and Diagnostic Findings
The
diagnosis of pneumonia is made by history (particularly of a recent respiratory
tract infection), physical examination, chest x-ray studies, blood culture
(bloodstream invasion, called bac-teremia, occurs frequently), and sputum
examination. The sputum sample is obtained by having the patient: (1) rinse the
mouth with water to minimize contamination by normal oral flora, (2) breathe
deeply several times, (3) cough deeply, and (4) expectorate the raised sputum
into a sterile container.
More
invasive procedures may be used to collect specimens. Sputum may be obtained by
nasotracheal or orotracheal suctioning with a sputum trap or by fiberoptic
bronchoscopy. Bronchoscopy is often used in patients with acute severe
infec-tion, patients with chronic or refractory infection, or
immuno-compromised patients when a diagnosis cannot be made from an
expectorated or induced specimen.
Medical Management
The
treatment of pneumonia includes administration of the ap-propriate antibiotic
as determined by the results of the Gram stain. However, an etiologic agent is
not identified in 50% of CAP cases and empiric therapy must be initiated.
Therapy for CAP is continuing to evolve. Guidelines exist to guide antibiotic
choice; however, the resistance patterns, prevalence of etiologic agents,
patient risk factors, and costs and availability of newer antibiotic agents
must all be taken into consideration.
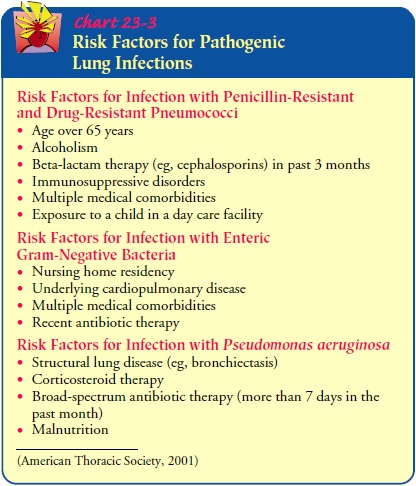
Several
organizations have published guidelines for the medical management of CAP
(Bartlett et al., 2000; American Thoracic Society, 2001). Recommendations are
classified by existing risk factors, setting (inpatient vs. outpatient
treatment), or specific pathogens. Examples of risk factors that may increase
the risk of infection with certain types of pathogens appear in Chart 23-3.
Recommendations
for treatment of outpatients with CAP who have no cardiopulmonary disease or
other modifying factors include a macrolide (erythromycin, azithromycin
[Zithromax], or clarithromycin [Biaxin]), doxycycline (Vibramycin), or a
flu-oroquinolone (eg, gatifloxacin [Tequin], levofloxacin [Levaquin]) with
enhanced activity against S. pneumoniae
(Bartlett et al., 2000; American Thoracic Society, 2001). Erythromycin should
be avoided in areas where H. influenzae
and S. aureus are more preva-lent
(Kenreigh & Wagner, 2000; Lynch, 2000). For those out-patients who have
cardiopulmonary disease or other modifying factors, treatment should include a
beta-lactam (oral cefpodoxime [Vantin], cefuroxime [Zinacef, Ceftin], high-dose
amoxicillin or amoxicillin/clavulanate [Augmentin, Clavulin]) plus a macrolide
or doxycycline. Also, a beta-lactam plus an antipneumococcal fluoro-quinolone
can be used (American Thoracic Society, 2001). These are guidelines; treatment
for individual patients may be modified.
For patients with CAP who are hospitalized and do not have cardiopulmonary disease or modifying factors, management con-sists of intravenous azithromycin (Zithromax) or monotherapy with an antipneumococcal fluoroquinolone. For inpatients with cardiopulmonary disease or modifying factors, the treatment in-volves an intravenous beta-lactam plus an intravenous or oral macrolide or doxycycline. An intravenous antipneumococcal flu-oroquinolone may also be used alone (American Thoracic Soci-ety, 2001). For acutely ill patients admitted to the intensive care unit, management includes an intravenous beta-lactam plus either an intravenous macrolide or fluoroquinolone. For patients at high risk for P. aeruginosa, more select antipseudomonal anti-biotics are administered intravenously.
If
specific pathogens have been identified for the CAP, more specific agents may
be utilized. Mycoplasma pneumonia is treated with doxycycline or a macrolide.
PCP responds best to pentamidine and trimethoprim–sulfamethoxazole (TMP-SMZ).
Amantadine and rimantadine are effective with influenza A and have been shown
to reduce the duration of fever and other systemic com-plications when
administered within 24 to 48 hours of the onset of an uncomplicated influenza
infection. These medications also reduce the duration and quantity of virus shedding
in the res-piratory secretions. They are most effective when used in
com-bination with influenza vaccine. Ganciclovir is used to treat
cytomegalovirus in the non-AIDS patient; cytomegalovirus immunoglobulin may
also be used.
HAP
has a different etiology from CAP. In suspected HAP or nosocomial pneumonia,
empirical treatment is usually ini-tiated with a broad-spectrum intravenous
antibiotic and may be monotherapy or combination therapy. In patients who are
mildly to moderately ill with a low risk of Pseudomonas,
the following antibiotics may be used: second-generation cephalosporins (eg,
cefuroxime [Ceftin, Zinacef] or cefamandole [Mandol]), non-pseudomonal
third-generation cephalosporins (ceftriaxone [Ro-cephin], cefotaxime
[Claforan], ampicillin-sulbactam [Unasyn]), or fluoroquinolones (eg,
ciprofloxacin [Cipro], levofloxacin [Lev-aquin]). For combination therapy, any
of the above may be used with an aminoglycoside.
For
patients at high risk for Pseudomonas
infection, an anti-pseudomonal penicillin plus an aminoglycoside (amikacin
[Amikin], gentamicin) or beta-lactamase inhibitor (ampicillin/ sulbactam
[Unasyn], ticarcillin/clavulanate [Timentin]) may be used. Other types of
combination therapy may also be used de-pending upon the individual characteristics
of the patient.
Of
concern is the rampant rise in respiratory pathogens that are resistant to
available antibiotics. Examples include vancomycin-resistant enterococcus (VRE)
and drug-resistant S. pneumoniae
(McGeer & Low, 2000). There is a tendency for clinicians to ag-gressively
use antibiotics inappropriately or to use broad-spectrum agents when
narrow-spectrum agents are more appropriate. Mechanisms to monitor and minimize
the inappropriate use of antibiotics are in place. Education of clinicians to
use evidence-based guidelines in the treatment of respiratory infection is
im-portant. Monitoring and surveillance of susceptibility patterns for
pathogens are also important.
Therapy
with parenteral agents usually is changed to oral anti-microbial agents when
there is evidence of a clinical response and the patient is able to tolerate
oral medications. The recommended duration of treatment for pneumococcal
pneumonia is 72 hours after the patient becomes afebrile. Most other forms of
pneumo-nia caused by bacterial pathogens are treated for 1 to 2 weeks after the
patient becomes afebrile. Atypical pneumonia is usually treated for 10 to 21
days (Bartlett, Dowell, Mandell et al., 2000).
Treatment
of viral pneumonia is primarily supportive. Anti-biotics are ineffective in
viral upper respiratory infections and pneumonia and may be associated with
adverse effects. Treatment of viral infections with antibiotics is a major
reason for the overuse of these medications in the United States. Antibiotics
are indicated with a viral respiratory infection only when a secondary bacterial pneumonia, bronchitis, or sinusitis
is present. Hydration is a nec-essary part of therapy because fever and
tachypnea may result in insensible fluid losses. Antipyretics may be used to treat
headache and fever; antitussive medications may be used for the associated
cough. Warm, moist inhalations are helpful in relieving bronchial irritation.
Antihistamines may provide benefit with reduced sneez-ing and rhinorrhea. Nasal
decongestants may also be used to treat symptoms and improve sleep; however,
excessive use may cause rebound nasal congestion. Treatment of viral pneumonia
(with the exception of antimicrobial therapy) is the same as that for
bac-terial pneumonia. The patient is placed on bed rest until the in-fection
shows signs of clearing. If hospitalized, the patient is observed carefully
until the clinical condition improves.
If
hypoxemia develops, oxygen is administered. Pulse oximetry or arterial blood
gas analysis is performed to determine the need for oxygen and to evaluate the
effectiveness of the therapy. A high concentration of oxygen is contraindicated
in patients with COPD because it may worsen alveolar ventilation by decreasing
the patient’s ventilatory drive, leading to further respiratory
de-compensation. Respiratory support measures include high oxygen
concentrations (fraction of inspired oxygen [FiO2]),
endotracheal intubation, and mechanical ventilation.
Figure
23-3 provides an algorithm for patients with suspected CAP.
Gerontologic Considerations
Pneumonia
in the elderly patient may occur as a primary prob-lem or as a complication of
a chronic disease process. Pulmonary infections in the elderly frequently are
difficult to treat and have a higher mortality rate than in younger patients.
General deteri-oration, weakness, abdominal symptoms, anorexia, confusion,
tachycardia, and tachypnea may signal the onset of pneumonia. The diagnosis of
pneumonia may be missed because the classic symptoms of cough, chest pain,
sputum production, and fever may be absent or masked in the elderly patient.
Also, the presence of some signs may be misleading. Abnormal breath sounds, for
example, may be due to microatelectasis that occurs in the aged as a result of
decreased mobility, decreased lung volumes, and other respiratory function
changes. Because chronic heart failure is often seen in the elderly, chest
x-rays may be obtained to assist in differentiating it from pneumonia as the
cause of clinical signs and symptoms.
Supportive
treatment includes hydration (with caution and frequent assessment because of
the risk of fluid overload in the elderly), supplemental oxygen therapy,
assistance with deep breath-ing, coughing, frequent position changes, and early
ambulation. All of these are particularly important in the care of the elderly
patient with pneumonia. To reduce or prevent serious complica-tions of
pneumonia in the elderly, vaccination against pneumo-coccal and influenza
infections is recommended.
Complications
SHOCK AND RESPIRATORY FAILURE
Severe
complications of pneumonia include hypotension and shock and respiratory
failure (especially with gram-negative bacte-rial disease in elderly patients).
These complications are encoun-tered chiefly in patients who have received no
specific treatment or inadequate or delayed treatment. These complications are
also en-countered when the infecting organism is resistant to therapy and when
a comorbid disease complicates the pneumonia.
If the patient is seriously ill, aggressive therapy may include hemodynamic and ventilatory support to combat peripheral col-lapse, maintain arterial blood pressure, and provide adequate oxy-genation. A vasopressor agent may be administered intravenously by continuous infusion and at a rate adjusted in accordance with the pressure response. Corticosteroids may be administered par-enterally to combat shock and toxicity in patients who are ex-tremely ill with pneumonia and in apparent danger of dying of the infection. Patients may require endotracheal intubation and mechanical ventilation. Congestive heart failure, cardiac dys-rhythmias, pericarditis, and myocarditis also are complications of pneumonia that may lead to shock.
ATELECTASIS AND PLEURAL EFFUSION
Atelectasis
(from obstruction of a bronchus by accumulated se-cretions) may occur at any
stage of acute pneumonia. Parapneu-monic pleural effusions occur in at least
40% of bacterial pneumonias. A parapneumonic effusion is any pleural effusion
associated with bacterial pneumonia, lung abscess, or bronchiec-tasis. After
the pleural effusion is detected on a chest x-ray, a tho-racentesis may be
performed to remove the fluid. The fluid is sent to the laboratory for
analysis. There are three stages of para-pneumonic pleural effusions based on
pathogenesis: uncompli-cated, complicated, and thoracic empyema. An empyema occurs when thick, purulent
fluid accumulates within the pleural space, often with fibrin development and a
loculated (walled-off) area where the infection is located. A chest tube may be
inserted to treat pleural infection by establishing proper drainage of the
empyema. Sterilization of the empyema cavity requires 4 to 6 weeks of
antibiotics. Sometimes surgical manage-ment is required.
SUPERINFECTION
Superinfection
may occur with the administration of very large doses of antibiotics, such as
penicillin, or with combinations of antibiotics. Superinfection may also occur
in the patient who has been receiving numerous courses and types of
antibi-otics. In such cases, bacteria may become resistant to the antibiotic
therapy. If the patient improves and the fever diminishes after initial
antibiotic therapy, but subsequently there is a rise in temperature with
increasing cough and evi-dence that the pneumonia has spread, a superinfection
is likely. Antibiotics are changed appropriately or discontinued entirely in
some cases.
Related Topics