Chapter: Medical Surgical Nursing: Management of Patients With Upper Respiratory Tract Disorders
Nursing Process: The Patient Undergoing Laryngectomy
NURSING PROCESS: THE PATIENT UNDERGOING LARYNGECTOMY
Assessment
The
nurse assesses the patient for the following symptoms: hoarseness, sore throat,
dyspnea, dysphagia, or pain and burning in the throat. The neck is palpated for
swelling.
If
treatment includes surgery, the nurse must know the nature of the surgery to
plan appropriate care. If the patient is expected to have no voice, a
preoperative evaluation by the speech thera-pist is indicated. The patient’s
ability to hear, see, read, and write is assessed. Visual impairment and
functional illiteracy may cre-ate additional problems with communication and
require creative approaches to ensure that the patient is able to communicate
any needs.
In
addition, the nurse determines the psychological readiness of the patient and family.
The idea of cancer is terrifying to most people. Fear is compounded by the
possibility of permanently losing one’s voice and, in some cases, of having
some degree of disfigurement. The nurse evaluates the patient’s and family’s
cop-ing methods to support them effectively both preoperatively and
postoperatively.
Diagnosis
NURSING DIAGNOSES
Based
on all the assessment data, major nursing diagnoses may include the following:
• Deficient knowledge about the surgical
procedure and post-operative course
• Anxiety and depression related to the
diagnosis of cancer and impending surgery
• Ineffective airway clearance related to
excess mucus pro-duction secondary to surgical alterations in the airway
• Impaired verbal communication related to
anatomic deficit secondary to removal of the larynx and to edema
• Imbalanced nutrition: less than body
requirements, related to inability to ingest food secondary to swallowing
difficulties
• Disturbed body image and low self-esteem
secondary to major neck surgery, change in the structure and function of the
larynx
• Self-care deficit related to pain,
weakness, fatigue, muscu-loskeletal impairment related to surgical procedure
and post-operative course
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on assessment data, potential complications that may de-velop include:
·
Respiratory distress (hypoxia,
airway obstruction, tracheal edema)
·
Hemorrhage
·
Infection
·
Wound breakdown
Planning and Goals
The
major goals for the patient may include attainment of an ad-equate level of
knowledge, reduction in anxiety, maintenance of a patent airway (patient is
able to handle own secretions), effective use of alternative means of
communication, attainment of optimal levels of nutrition and hydration,
improvement in body image and self-esteem, improved self-care management, and
ab-sence of complications.
Nursing Interventions
TEACHING THE PATIENT PREOPERATIVELY
The
diagnosis of laryngeal cancer is associated with misconcep-tions and fears.
Many people assume that loss of speech and dis-figurement are inevitable with
this condition. Once the physician explains the diagnosis to the patient, the
nurse clarifies any mis-conceptions by identifying the location of the larynx,
its function, the nature of the surgical procedure, and its effect on speech.
In-formational materials (written and audiovisual) about the surgery are given
to the patient and family for review and reinforcement.
If
a complete laryngectomy is planned, the patient should know that the natural
voice will be lost, but that special training can provide a means for
communicating. However, the ability to sing, laugh, or whistle will be lost.
Until this training is initiated, the patient needs to know that communication
will be possible by using the call light or special communication board and by
writing. The nurse answers questions about the nature of the surgery and
reinforces the physician’s explanation that the patient will lose the ability
to vocalize, but that a rehabilitation program is available. The multidisciplinary
team conducts an initial as-sessment of the patient and family. The team might
include the nurse, physician, respiratory therapist, speech therapist, clinical
nurse specialist, social worker, dietitian, and home care nurse.
Next,
the nurse reviews equipment and treatments for post-operative care with the
patient and family, teaches important coughing and deep-breathing exercises,
and assists the patient to perform a return demonstration. The nurse clarifies
the patient’s role in the postoperative and rehabilitation periods.
REDUCING ANXIETY AND DEPRESSION
Because
surgery of the larynx is performed most commonly for a malignant tumor, the
patient may have many questions: Will the surgeon be able to remove all of the
tumor? Is it cancer? Will I die? Will I choke? Will I suffocate? Will I ever
speak again? What will I look like? The psychological preparation of the
patient is as important as the physical preparation.
Any
patient undergoing surgery may have many fears. In la-ryngeal surgery, these
fears may relate to the diagnosis of cancer and may be compounded by the
possibility of permanent loss of the voice and disfigurement. The nurse
provides the patient and family with opportunities to ask questions, verbalize
feelings, and discuss perceptions. It is important to address any questions and
misconceptions the patient and family have. During the pre-operative or
postoperative period, a visit from someone who has had a laryngectomy may
reassure the patient that people are avail-able to help and that rehabilitation
is possible.
MAINTAINING A PATENT AIRWAY
The
nurse promotes a patent airway by positioning the patient in the semi-Fowler’s
or Fowler’s position after recovery from anes-thesia. Observing the patient for
restlessness, labored breathing, apprehension, and increased pulse rate helps
the nurse identify possible respiratory or circulatory problems. Medications
that de-press respiration, particularly opioids, should be used cautiously. As
with other surgical patients, the nurse encourages the laryn-gectomy patient to
turn, cough, and take deep breaths. If neces-sary, suctioning may be performed
to remove secretions. The nurse also encourages and assists the patient with
early ambula-tion to prevent atelectasis and pneumonia.
If
a total laryngectomy was performed, a laryngectomy tube will most likely be in
place. (In some instances a laryngectomy tube is not used; in others it is used
temporarily, and in many it is used permanently.) The laryngectomy tube, which
is shorter than a tracheostomy tube but has a larger diameter, is the
pa-tient’s only airway. The care of this tube is the same as for a
tra-cheostomy tube. The nurse cleans the stoma daily with saline solution or
another prescribed solution. If a non–oil-based antibiotic ointment is prescribed,
the nurse applies it around the stoma and suture line. If crusting appears
around the stoma, the nurse removes the crusts with sterile tweezers and
ap-plies additional ointment.
Wound
drains may be in place to assist in removal of fluid and air from the surgical
site. Suction also may be used, but cautiously, to avoid trauma to the surgical
site and incision. The nurse ob-serves, measures, and records drainage. When
drainage is less than 50 to 60 mL/day, the physician usually removes the drains.
Frequently,
the patient coughs up large amounts of mucus through this opening. Because air
passes directly into the trachea without being warmed and moistened by the
upper respiratory mucosa, the tracheobronchial tree compensates by secreting
ex-cessive amounts of mucus. Therefore, the patient will have fre-quent
coughing episodes and may develop a brassy-sounding, mucus-producing cough. The
nurse should reassure the patient that these problems will diminish in time as
the tracheobronchial mucosa adapts to the altered physiology.
After
the patient coughs, the tracheostomy opening must be wiped clean and clear of
mucus. A simple gauze dressing, wash-cloth, or even paper towel (because of its
size and absorbency) worn below the tracheostomy may serve as a barrier to
protect the clothing from the copious mucus that the patient may expel
initially.
One
of the most important factors in decreasing cough, mucus production, and
crusting around the stoma is adequate humidi-fication of the environment.
Mechanical humidifiers and aerosol generators (nebulizers) increase the
humidity and are important for the patient’s comfort.
The
laryngectomy tube may be removed when the stoma is well healed, within 3 to 6
weeks after surgery. The nurse can teach the patient how to clean and change
the tube and remove secretions.
PROMOTING ALTERNATIVE COMMUNICATION METHODS
Understanding the patient’s postoperative needs is critical.
Alter-native means of communication are established and used consis-tently by
all personnel who come in contact with the patient—for example, a call bell or
hand bell may be placed within easy reach of the patient. Because a Magic Slate
often is used for communi-cation, the nurse should document which hand the
patient uses for writing so that the opposite arm can be used for intravenous
infusions. (The nurse should discard any old notes used for com-munication to
ensure the patient’s privacy.) If the patient cannot write, a
picture-word-phrase board or hand signals can be used. Preoperatively, the
nurse reviews the system of communication to be used postoperatively with the
patient.
Because
it is very time-consuming to have to write everything or communicate through
gestures, the inability to speak can be very frustrating. The patient may
become impatient and angry when not understood. In such cases, other staff
members need to be alert to the problem and also recognize that the patient
will be unable to use the intercom system.The return of communication is
generally the ultimate goal in the rehabilitation of the laryngectomy patient.
The nurse works with the patient, speech therapist, and family to encourage use
of alternative communication methods.
PROMOTING ADEQUATE NUTRITION
Postoperatively,
the patient may not be permitted to eat or drink for 10 to 14 days. Alternative
sources of nutrition and hydration include intravenous fluids, enteral feedings
through a nasogastric tube, and parenteral nutrition.
Once
the patient is ready to start oral feedings, the nurse ex-plains that thick
liquids will be used first because they are easy to swallow. The nurse
instructs the patient to avoid sweet foods, which increase salivation and
suppress the appetite. Solid foods are introduced as tolerated. The nurse
instructs the patient to rinse the mouth with warm water or mouthwash and to
brush the teeth frequently.
The
patient can expect to have a diminished sense of taste and smell for a period
of time after surgery. Inhaled air passes directly into the trachea, bypassing
the nose and the olfactory end organs. Because taste and smell are so closely
connected, taste sensations are altered. In time, however, the patient usually
accommodates to this problem and olfactory sensation adapts, often with return
of interest in eating. The nurse observes the patient for any diffi-culty
swallowing, particularly when eating resumes, and reports its occurrence to the
physician.
PROMOTING POSITIVE BODY IMAGE AND SELF-ESTEEM
Disfiguring surgery and an altered communication pattern are a
threat to a patient’s body image and self-esteem. The reaction of family
members and friends is a major concern for the patient. The nurse encourages
the patient to express any feelings about the changes brought about by surgery,
particularly those related to fear, anger, depression, and isolation.
A
positive approach is important when caring for the patient. Promoting self-care
activities is part of this approach. It is im-portant for the patient and
family to begin participating in self-care activities as soon as possible. The
nurse needs to be a good listener and a support to the family, especially when
explaining the tubes, dressings, and drains that are in place postoperatively.
Referral to a support group, such as Lost Chord or New Voice clubs (through the
International Association of Laryngectomees) and I Can Cope (through the
American Cancer Society), may help the patient and family deal with the changes
in their lives. Groups such as Lost Chord and New Voice promote and support the
re-habilitation of people who have had a laryngectomy by providing an
opportunity for exchanging ideas and sharing information.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
The
immediate potential complications after laryngectomy in-clude respiratory
distress and hypoxia, hemorrhage, infection, and wound breakdown.
Respiratory Distress and Hypoxia
The
nurse monitors the patient for signs and symptoms of respi-ratory distress and
hypoxia, particularly restlessness, irritation, agitation, confusion,
tachypnea, use of accessory muscles, and de-creased oxygen saturation on pulse
oximetry (SpO2). Any change in the respiratory
status requires immediate intervention. Ob-struction needs to be ruled out
immediately by suctioning and having the patient cough and breathe deeply.
Hypoxia and air-way obstruction, if not immediately treated, are
life-threatening.
The
nurse contacts the physician immediately if nursing measures do not improve the
patient’s respiratory status.
Hemorrhage
Bleeding
at the surgical site from the drains or with tracheal suc-tioning may signal
the occurrence of hemorrhage. The nurse should notify the surgeon of any active
bleeding immediately. Bleeding may occur at a variety of sites, including the
surgical site, drains, or trachea. Rupture of the carotid artery is especially
dan-gerous. Should this occur, the nurse should apply direct pressure over the
artery, summon assistance, and provide emotional sup-port to the patient until
the vessel can be ligated. It is important to monitor vital signs for changes,
particularly increased pulse rate, decreased blood pressure, and rapid deep
respirations. Cold, clammy, pale skin may indicate active bleeding.
Infection
The
nurse observes for postoperative infection. Early signs of in-fection include
an increase in temperature and pulse, a change in the type of wound drainage,
or increased areas of redness or ten-derness at the surgical site. Other signs
include purulent drainage, odor, and increased wound drainage. The nurse
reports any sig-nificant change to the surgeon.
Wound Breakdown
Wound
breakdown due to infection, poor wound healing, or de-velopment of a fistula or
as a result of radiation therapy or tumor growth can create a life-threatening
emergency. The carotid artery, which is close to the stoma, may rupture from
erosion if the wound does not heal properly. The nurse observes the stoma area
for wound breakdown, hematoma, and bleeding and reports any significant changes
to the surgeon. If wound breakdown oc-curs, the patient must be monitored
carefully and identified as being at high risk for carotid hemorrhage.
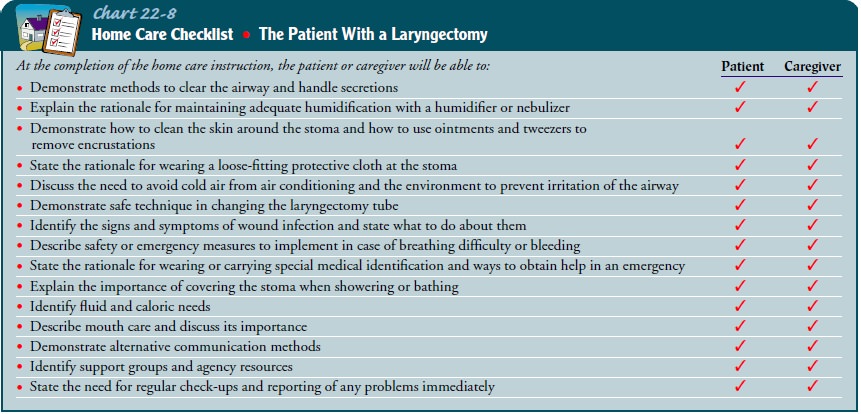
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
nurse has an important role in the recovery and rehabilita-tion of the
laryngectomy patient. In an effort to facilitate the pa-tient’s ability to
manage self-care, discharge instruction begins as soon as the patient is able
to participate. Nursing care and patient teaching in the hospital, outpatient
setting, and rehabilitation or long-term care facility must take into
consideration the many emotions, physical changes, and lifestyle changes
experienced by the patient. In preparing the patient to go home, the nurse
as-sesses the patient’s readiness to learn and the level of knowledge about
self-care management. The nurse also reassures the patient and family that most
self-care management strategies can be mas-tered. The patient will need to
learn a variety of self-care behav-iors, including tracheostomy and stoma care,
wound care, and oral hygiene. In addition, the nurse instructs the patient
about the need for safe hygiene and recreational activities.
Tracheostomy and Stoma Care.
The nurse provides specific in-structions to the patient and
family about what to expect from the tracheostomy and its management. The nurse
teaches the pa-tient and family caregiver to perform suctioning and emergency
measures and tracheostomy and stoma care. The nurse stresses the importance of
humidification at home and instructs the fam-ily to set up a humidification
system before the patient returns home. In addition, the nurse cautions the
patient and family that air-conditioned air may be too cool or too dry, and
thus too irri-tating, for the patient with a new laryngectomy.
Hygiene and Safety Measures.
The nurse instructs the patientand family about safety precautions
needed because of the struc-tural changes resulting from the surgery. Special
precautions are needed in the shower to prevent water from entering the stoma.
Wearing a loose-fitting plastic bib over the tracheostomy or sim-ply holding
the hand over the opening is effective. Swimming is not recommended, however,
because people with a laryngectomy can drown without getting their face wet.
Barbers and beauticians need to be alerted so that hair sprays, loose hair, and
powder do not get near the stoma, because they can block or irritate the
tra-chea and possibly cause infection. These self-care points are sum-marized
in Chart 22-8.
Recreation
and exercise are important, and all but very strenu-ous exercise can be enjoyed
safely. Avoidance of strenuous exercise and fatigue is important because, when
tired, the patient has more difficulty speaking, which can be discouraging.
Additional safety points to address include the need for the patient to wear or
carry medical identification, such as a bracelet or card, to alert medical
personnel to the special requirements for resuscitation should this need arise.
When resuscitation is needed, direct mouth-to-stoma ventilation should be
performed. For home emergency situations, prerecorded emergency messages for
police, the fire department, or other rescue services can be kept near the
phone to be used quickly.
The
nurse instructs and encourages the patient to perform oral care on a regular
basis to prevent halitosis and infection. If the pa-tient is receiving
radiation therapy, there will be a decrease in saliva, and synthetic saliva may
be required. The nurse instructs the patient to drink water or sugar-free
liquids throughout the day and to use a humidifier at home. Brushing the teeth
or den-tures and rinsing the mouth several times a day will assist in
main-taining proper oral hygiene.
Continuing Care
Referral
for home care is an important aspect of postoperative care for the patient who
has had a laryngectomy and will assist the patient and family in the transition
to the home. The home care nurse assesses the patient’s general health status
and the ability of the patient and family to care for the stoma and
tracheostomy.The nurse assesses the surgical incisions, nutritional and
respira-tory status, and adequacy of pain management. The nurse assesses not
only for signs and symptoms of complications but also for the patient’s and
family’s knowledge of which signs and symptoms to report to the physician.
During the home visit, the nurse iden-tifies and addresses other learning needs
of the patient and family, such as adaptation to physical, lifestyle, and
functional changes. It is important to assess the patient’s psychological
status as well. The home care nurse reinforces previous teaching and provides
reassurance and support to the patient and family as needed.
The
nurse encourages the person who has had a laryngectomy to have regular physical
examinations and to seek advice con-cerning any problems related to recovery
and rehabilitation. The patient is also reminded to participate in health promotion
activ-ities and health screening and about the importance of keeping scheduled
appointments with the physician, speech therapist, and other health care
providers.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1.
Acquires an adequate level of
knowledge, verbalizing an understanding of the surgical procedure and
performing self-care adequately
2.
Demonstrates less anxiety and
depression
a.
Expresses a sense of hope
b.
Is aware of available community
organizations and agen-cies such as the Lost Chord or New Voice groups
c.
Participates in support group, such
as I Can Cope
3.
Maintains a clear airway and handles
own secretions; also demonstrates practical, safe, and correct technique for
clean-ing and changing the laryngectomy tube
4.
Acquires effective communication
techniques
a.
Uses assistive devices and
strategies for communication (Magic Slate, call bell, picture board, sign
language, lip reading, computer aids)
b. Follows the recommendations of the speech therapist
5.
Maintains balanced nutrition and
adequate fluid intake
6.
Exhibits improved body image,
self-esteem, and self-concept
a.
Expresses feelings and concerns
b.
Participates in self-care and
decision making
c.
Accepts information about support
group
7.
Exhibits no complications
a.
Vital signs (blood pressure,
temperature, pulse, respira-tory rate) normal
b.
No redness, tenderness, or purulent
drainage at surgical site
c.
Demonstrates a patent airway and
appropriate respira-tions
d.
No bleeding from surgical site and
minimal bleeding from drains
e.
No wound breakdown
8.
Adheres to rehabilitation and home
care program
a.
Practices recommended speech therapy
b.
Demonstrates proper methods for
caring for stoma and laryngectomy tube (if present)
c.
Verbalizes understanding of symptoms
that require medical attention
d.
States safety measures to take in
emergencies
e.
Performs oral hygiene as prescribed
Related Topics