Chapter: Medical Surgical Nursing: Management of Patients With Upper Respiratory Tract Disorders
Nursing Process: The Patient With Upper Airway Infection
NURSING PROCESS: THE PATIENT WITH UPPER AIRWAY INFECTION
Assessment
A
health history may reveal signs and symptoms of headache, sore throat, pain
around the eyes and on either side of the nose, diffi-culty in swallowing,
cough, hoarseness, fever, stuffiness, and gen-eralized discomfort and fatigue.
Determining when the symptoms began, what precipitated them, what if anything
re-lieves them, and what aggravates them is part of the assessment. It also is
important to determine any history of allergy or the ex-istence of a
concomitant illness.
Inspection
may reveal swelling, lesions, or asymmetry of the nose as well as bleeding or
discharge. The nurse inspects the nasal mucosa for abnormal findings such as
increased redness, swelling, or exudate, and nasal polyps, which may develop in
chronic rhinitis.
The
nurse palpates the frontal and maxillary sinuses for ten-derness, which
suggests inflammation, and then inspects the throat by having the patient open
the mouth wide and take a deep breath. The tonsils and pharynx are inspected
for abnormal findings such as redness, asymmetry, or evidence of drainage,
ulcera-tion, or enlargement.
Next
the nurse palpates the trachea to determine the midline position in the neck
and to detect any masses or deformities. The neck lymph nodes also are palpated
for associated enlargement and tenderness.
Diagnosis
NURSING DIAGNOSES
• Ineffective airway clearance related to excessive mucus pro-duction secondary to retained secretions and inflammation
• Acute pain related to upper airway irritation secondary to an infection
• Impaired verbal communication related to physiologic changes and upper airway irritation secondary to infection or swelling
• Deficient fluid volume related to increased fluid loss sec-ondary to diaphoresis associated with a fever
• Deficient knowledge regarding prevention of upper respi-ratory infections, treatment regimen, surgical procedure, or postoperative care
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on assessment data, potential complications may include:
• Sepsis
• Meningitis
• Peritonsillar abscess
• Otitis media
• Sinusitis
Planning and Goals
The
major goals for the patient may include maintenance of a patent airway, relief
of pain, maintenance of effective means of communication, normal hydration,
knowledge of how to prevent upper airway infections, and absence of
complications.
Nursing Interventions
MAINTAINING A PATENT AIRWAY
An
accumulation of secretions can block the airway in patients with an upper
airway infection. As a result, changes in the respi-ratory pattern occur, and
the work of breathing required to get beyond the blockage increases. The nurse
can implement several measures to loosen thick secretions or to keep the secretions
moist so that they can be easily expectorated. Increasing fluid intake helps
thin the mucus. Use of room vaporizers or steam inhalation also loosens
secretions and reduces inflammation of the mucous membranes. To enhance
drainage from the sinuses, the nurse in-structs the patient about the best
position to assume; this depends on the location of the infection or
inflammation. For example, drainage for sinusitis or rhinitis is achieved in
the upright posi-tion. In some conditions, topical or systemic medications,
when prescribed, help to relieve nasal or throat congestion.
PROMOTING COMFORT
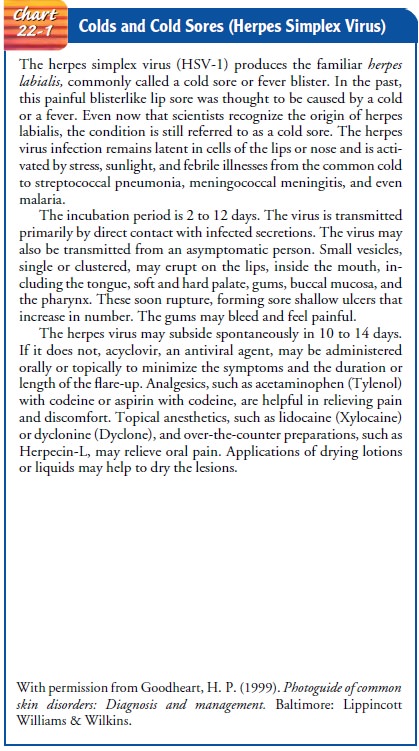
Upper
respiratory tract infections usually produce localized dis-comfort. In
sinusitis, pain may occur in the area of the sinuses or may produce a general headache. In
pharyngitis, laryngitis, or tonsillitis, a sore throat occurs. The nurse
encourages the patient to take analgesics, such as acetaminophen with codeine,
as pre-scribed, which will help relieve this discomfort. Other helpful measures
include topical anesthetic agents for symptomatic relief of herpes simplex
blisters (see Chart 22-1) and sore throats, hot packs to relieve the congestion
of sinusitis and promote drainage, and warm water gargles or irrigations to
relieve the pain of a sore throat. The nurse encourages rest to relieve the
generalized dis-comfort and fever that accompany many upper airway conditions
(especially rhinitis, pharyngitis, and laryngitis). The nurse in-structs the
patient in general hygiene techniques to prevent the spread of infection. For
postoperative care following tonsillec-tomy and adenoidectomy, an ice collar
may reduce swelling and decrease bleeding.
PROMOTING COMMUNICATION
Upper
airway infections may result in hoarseness or loss of speech. The nurse
instructs the patient to refrain from speaking as much as possible and to
communicate in writing instead, if possible. Additional strain on the vocal
cords may delay full return of the voice.
ENCOURAGING FLUID INTAKE
In
upper airway infections, the work of breathing and the respi-ratory rate
increase as inflammation and secretions develop. This, in turn, may increase
insensible fluid loss. Fever further increases the metabolic rate, diaphoresis,
and fluid loss.
Sore
throat, malaise, and fever may interfere with a patient’s willingness to eat.
The nurse encourages the patient to drink 2 to 3 L of fluid per day during the
acute stage of airway infection, un-less contraindicated, to thin secretions
and promote drainage. Liquids (hot or cold) may be soothing, depending on the illness.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Prevention
of most upper airway infections is difficult because of the many potential
causes. However, most upper respiratory in-fections are transmitted by
hand-to-hand contact. Therefore, it is important to teach the patient and
family how to minimize the spread of infection to others. Other preventive
strategies are iden-tified in Chart 22-2. The nurse advises the patient to
avoid ex-posure to others at risk for serious illness if respiratory infection
is transmitted. Those at risk include elderly adults, immuno-suppressed people,
and those with chronic health problems.
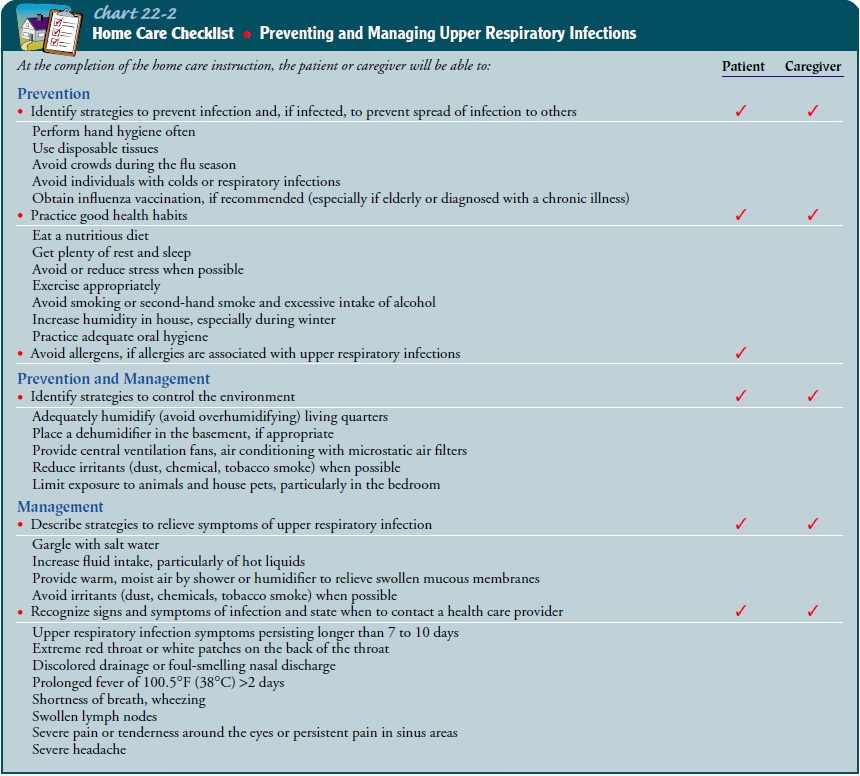
The
nurse teaches patients and their families strategies to re-lieve symptoms of
upper respiratory infections. These include in-creasing the humidity level,
encouraging adequate fluid intake, getting adequate rest, using warm water
gargles or irrigations and topical anesthetic agents to relieve sore throat,
and applying hot packs to relieve congestion. The nurse reinforces the need to
com-plete the treatment regimen, particularly when antibiotics are prescribed.
Continuing Care
Referral
for home care is rare. However, it may be indicated for the person whose health
status was compromised before the onset of the respiratory infection and for
those who cannot manage self-care without assistance. In such circumstances,
the home care nurse assesses the patient’s respiratory status and progress in
re-covery. The nurse may advise elderly patients and those who would be at increased
risk from a respiratory infection to consider an annual influenza vaccine. A
follow-up appointment with the primary care provider may be indicated for
patients with com-promised health status to ensure that the respiratory
infection has resolved.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
While
major complications of upper respiratory infections are rare, the nurse must be
aware of them and assess the patient for them. Because most patients with upper
respiratory infections are managed at home, patients and their families must be
instructed to monitor for signs and symptoms and to seek immediate med-ical
care if the patient’s condition does not improve or if the pa-tient’s physical
status appears to be worsening.
Sepsis
and meningitis may occur in patients with compro-mised immune status or in
those with an overwhelming bacterial infection. The patient with an upper
respiratory infection and family members are instructed to seek medical care if
the patient’s condition fails to improve within several days of the onset of
symptoms, if unusual symptoms develop, or if the patient’s con-dition
deteriorates. They are instructed about signs and symp-toms that require
further attention: persistent or high fever, increasing shortness of breath,
confusion, and increasing weak-ness and malaise. The patient with sepsis
requires expert care to treat the infection, stabilize vital signs, and prevent
or treat sep-ticemia and shock. Deterioration of the patient’s condition
ne-cessitates intensive care measures (eg, hemodynamic monitoring and
administration of vasoactive medications, intravenous fluids, nutritional
support, corticosteroids) to monitor the patient’s sta-tus and to support the
patient’s vital signs. High doses of antibi-otics may be administered to treat
the causative organism. The nurse’s role is to monitor the patient’s vital
signs, hemodynamic status, and laboratory values, administer needed treatment,
alle-viate the patient’s physical discomfort, and provide explanations,
teaching, and emotional support to the patient and family.
Peritonsillar
abscess may develop following an acute infection of the tonsils. The patient
requires treatment to drain the abscess and receives antibiotics for infection
and topical anesthetic agents and throat irrigations to relieve pain and sore
throat. Follow-up is necessary to ensure that the abscess resolves;
tonsillectomy may be required. The nurse assists the patient in administering
throat irrigations and instructs the patient and family about the impor-tance
of adhering to the prescribed treatment regimen and rec-ommended follow-up
appointments.
Otitis
media and sinusitis may develop with upper respiratory infection. The patient
and family are instructed about the signs and symptoms of otitis media and
sinusitis and about the impor-tance of follow-up with the primary health care
practitioner to ensure adequate evaluation and treatment of these conditions.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1.
Maintains a patent airway by managing
secretions
a.
Reports decreased congestion
b.
Assumes best position to facilitate
drainage of secretions
2.
Reports feeling more comfortable
a.
Uses comfort measures: analgesics,
hot packs, gargles, rest
b.
Demonstrates adequate oral hygiene
3.
Demonstrates ability to communicate
needs, wants, level of comfort
4.
Maintains adequate fluid intake
5.
Identifies strategies to prevent
upper airway infections and allergic reactions
a.
Demonstrates hand hygiene technique
b.
Identifies the value of the
influenza vaccine
6.
Demonstrates an adequate level of
knowledge and per-forms self-care adequately
7.
Becomes free of signs and symptoms
of infection
a.
Exhibits normal vital signs
(temperature, pulse, respira-tory rate)
b.
Absence of purulent drainage
c.
Free of pain in ears, sinuses, and
throat
Related Topics