Chapter: Medical Surgical Nursing: Management of Patients With Upper Respiratory Tract Disorders
Obstruction During Sleep - Upper Respiratory Airway
Obstruction and Trauma of the Upper Respiratory Airway
OBSTRUCTION DURING SLEEP
A
variety of respiratory disorders are associated with sleep, the most common
being sleep apnea syndrome. Sleep apnea syn-drome is defined as cessation of
breathing (apnea) during sleep.
Pathophysiology
Sleep
apnea is classified into three types:
·
Obstructive—lack of air flow due to
pharyngeal occlusion
·
Central—simultaneous cessation of
both air flow and res-piratory movements
·
Mixed—a combination of central and
obstructive apnea within one apneic episode
The
most common type of sleep apnea syndrome, obstructive sleep apnea, will be
presented here.
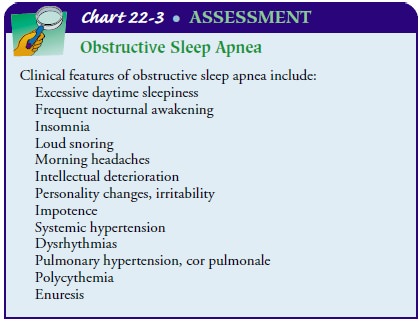
Clinical Manifestations
It
is estimated that 12 million Americans have sleep apnea (Na-tional Institute of
Health, 2000). It is more prevalent in men, es-pecially those who are older and
overweight. Cigarette smoking is a risk factor. Obstructive sleep apnea is
defined as frequent and loud snoring and breathing cessation for 10 seconds or
more for five episodes per hour or more, followed by awakening abruptly with a
loud snort as the blood oxygen level drops. Patients with sleep apnea may
experience anywhere from five apneic episodes per hour to several hundred per
night. Other symptoms include excessive daytime sleepiness, morning headache, sore
throat, in-tellectual deterioration, personality changes, behavioral disorders,
enuresis, impotence, obesity, and complaints by the partner that the patient
snores loudly or is unusually restless during sleep (Chart 22-3).
The
obstruction may be caused by mechanical factors such as a reduced diameter of
the upper airway or dynamic changes in the upper airway during sleep. The
activity of the tonic dilator mus-cles of the upper airway is reduced during
sleep. These sleep-related changes may predispose the patient to increased
upper airway collapse with the small amounts of negative pressure generated
during inspiration. Obstructive sleep apnea may be associated with obesity and
with other conditions that reduce pharyngeal muscle tone (eg, neuromuscular disease,
sedative/ hypnotic medications, acute ingestion of alcohol). The diagnosis of
sleep apnea is made based on clinical features plus polysomno-graphic findings
(sleep test), in which the cardiopulmonary sta-tus of the patient is monitored
during an episode of sleep.
The
effects of obstructive sleep apnea can seriously tax the heart and lungs.
Repetitive apneic events result in hypoxia and hypercapnia, which triggers a
sympathetic response. As a conse-quence, patients have a high prevalence of
hypertension and an increased risk of myocardial infarction and stroke. In
patients with underlying cardiovascular disease, the nocturnal hypoxemia may
predispose to dysrhythmias.
Medical Management
Patients
usually seek medical treatment because their partners ex-press concern or
because they experience excessive sleeplessness at inappropriate times or
settings (eg, while driving a car). A variety of treatments are used. In mild
cases, the patient is advised to avoid alcohol and medications that depress the
upper airway and to lose weight. In more severe cases involving hypoxemia with
se-vere CO2 retention (hypercapnia), the
treatment includes con-tinuous positive airway pressure or bilevel positive
airway pressure therapy with supplemental oxygen via nasal cannula.
Surgical
procedures (eg, uvulopalatopharyngoplasty) may be performed to correct the
obstruction. As a last resort, a trache-ostomy is performed to bypass the
obstruction if the potential for respiratory failure or life-threatening
dysrhythmias exists. The tra-cheostomy is unplugged only during sleep. Although
this is an ef-fective treatment, it is used in a limited number of patients
because of its associated physical disfigurement (Murray & Nadel, 2001).
PHARMACOLOGIC THERAPY
Treatment
of central sleep apnea also includes medication. Pro-triptyline (Triptil) given
at bedtime is thought to increase the respiratory drive and improve upper
airway muscle tone. Med-roxyprogesterone acetate (Provera) and acetazolamide
(Diamox) have been recommended for sleep apnea associated with chronic alveolar
hypoventilation, but their benefits have not been well es-tablished.
Administration of low-flow nasal oxygen at night can help relieve hypoxemia in
some patients but has little effect on the frequency or severity of apnea.
Nursing Management
The
patient with obstructive sleep apnea may not recognize the potential
consequences of the disorder. Therefore, the nurse ex-plains the disorder in
language that is understandable to the patient and relates symptoms (daytime
sleepiness) to the under-lying disorder. The nurse also instructs the patient
and family about treatments, including the correct and safe use of oxygen, if
prescribed.
Related Topics