Chapter: Medical Surgical Nursing: Management of Patients With Upper Respiratory Tract Disorders
Acute Sinusitis - Upper Airway Infections
ACUTE SINUSITIS
The
sinuses, mucus-lined cavities filled with air that drain nor-mally into the
nose, are involved in a high proportion of upper respiratory tract infections.
If their openings into the nasal pas-sages are clear, the infections resolve
promptly. However, if their drainage is obstructed by a deviated septum or by
hypertrophied turbinates, spurs, or nasal polyps or tumors, sinus infection may
persist as a smoldering secondary infection or progress to an acute suppurative
process (causing purulent discharge). Sinusitis
af-fects over 14% of the population and accounts for billions of dol-lars in
direct health care costs (Tierney, McPhee, & Papadakis, 2001). Some
individuals are more prone to sinusitis because of their occupations. For
example, continuous exposure to environ-mental hazards such as paint, sawdust,
and chemicals may result in chronic inflammation of the nasal passages.
Pathophysiology
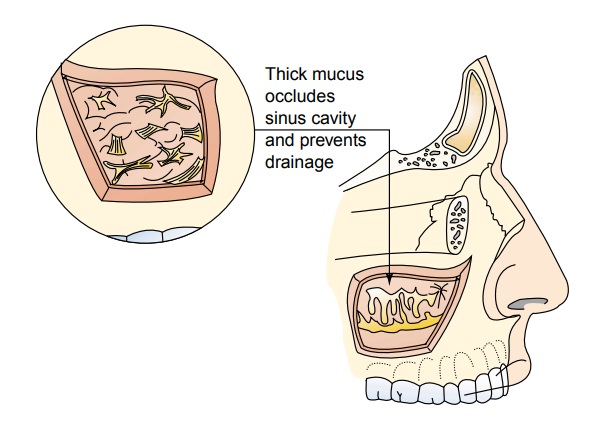
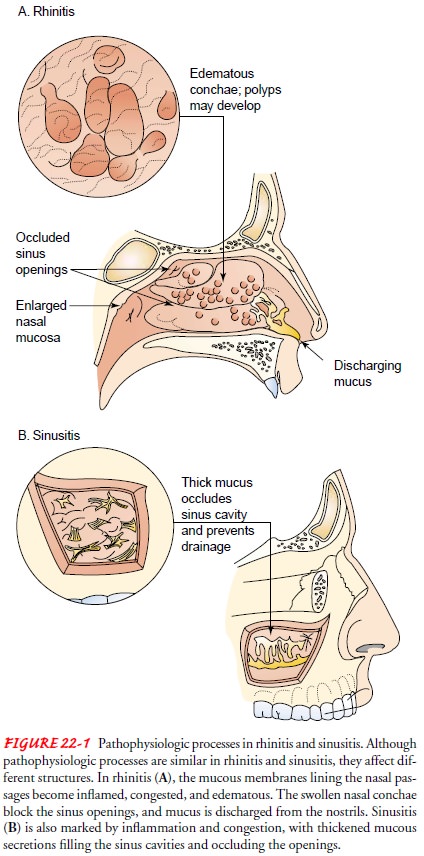
Acute sinusitis is an infection of the
paranasal sinuses. It fre-quently develops as a result of an upper respiratory
infection, such as an unresolved viral or bacterial infection, or an
exacerbation of allergic rhinitis. Nasal congestion, caused by inflammation,
edema, and transudation of fluid, leads to obstruction of the sinus cavi-ties
(see Fig. 22-1). This provides an excellent medium for bac-terial growth.
Bacterial organisms account for more than 60% of the cases of acute sinusitis,
namely Streptococcus pneumoniae,Haemophilus
influenzae, and Moraxella catarrhalis
(Murray &Nadel, 2001). Dental infections also have been associated with
acute sinusitis.
Clinical Manifestations
Symptoms of acute sinusitis may include facial pain or pressure over the affected sinus area, nasal obstruction, fatigue, purulent nasal discharge, fever, headache, ear pain and fullness, dental pain, cough, a decreased sense of smell, sore throat, eyelid edema, or facial congestion or fullness. Acute sinusitis can be difficult to differentiate from an upper respiratory infection or allergic rhinitis.
Assessment and Diagnostic Findings
A
careful history and physical examination are performed. The head and neck,
particularly the nose, ears, teeth, sinuses, pharynx, and chest, are examined.
There may be tenderness to palpation over the infected sinus area. The sinuses
are percussed using the index finger, tapping lightly to determine if the
patient experi-ences pain. The affected area is also transilluminated; with
sinusi-tis, there is a decrease in the transmission of light. Sinus x-rays may
be performed to detect sinus opac-ity, mucosal thickening, bone destruction,
and air–fluid levels. Computed tomography scanning of the sinuses is the most
effec-tive diagnostic tool. It is also used to rule out other local or
sys-temic disorders, such as tumor, fistula, and allergy.
Complications
Acute sinusitis, if left untreated, may
lead to severe and occa-sionally life-threatening complications such as
meningitis, brain abscess, ischemic infarction, and osteomyelitis. Other
complications of sinusitis, although uncommon, include severe orbital
cel-lulitis, subperiosteal abscess, and cavernous sinus thrombosis.
Medical Management
The
goals of treatment of acute sinusitis are to treat the infection, shrink the
nasal mucosa, and relieve pain. There is a growing con-cern over the
inappropriate use of antibiotics for viral upper res-piratory infections; such
overuse has resulted in antibiotics being less effective (more resistant) in
treating bacterial infections such as sinusitis. As a result, careful
consideration is given to the po-tential pathogen before antimicrobial agents
are prescribed.
The
antimicrobial agents of choice for a bacterial infection vary in clinical practice.
First-line antibiotics include amoxicillin (Amoxil),
trimethoprim/sulfamethoxazole (Bactrim, Septra), and erythromycin. Second-line
antibiotics include cephalosporins such as cefuroxime axetil (Ceftin),
cefpodoxime (Vantin), and cef-prozil (Cefzil) and amoxicillin clavulanate
(Augmentin). Newer and more expensive antibiotics with a broader spectrum
include
.macrolides,
azithromycin (Zithromax), and clarithromycin (Biaxin). Quinolones such as
ciprofloxacin (Cipro), levofloxacin (Levaquin) (used with severe penicillin
allergy), and sparfloxacin (Zagam) have also been used. The course of treatment
is usually 10 to 14 days. A recent report found little difference in clinical
outcomes between first-line and second-line antibiotics; however, costs were greater
when newer second-line antibiotics were used (Piccirillo, Mager, Frisse et al.,
2001).
Use
of oral and topical decongestant agents may decrease mu-cosal swelling of nasal
polyps, thereby improving drainage of the sinuses. Heated mist and saline irrigation
also may be effective for opening blocked passages. Decongestant agents such as
pseudo-ephedrine (Sudafed, Dimetapp) have proven effective because of their
vasoconstrictive properties. Topical decongestant agents such as oxymetazoline
(Afrin) may be used for up to 72 hours. It is important to administer them with
the patient’s head tilted back to promote maximal dispersion of the medication.
Guaife-nesin (Robitussin, Anti-Tuss), a mucolytic agent, may also be ef-fective
in reducing nasal congestion.
In
2000, the U.S. Food and Drug Administration issued a public health advisory
concerning phenylpropanolamine, which previously had been commonly used in oral
decongestants and diet pills. The voluntary recall of products containing this
ingre-dient was based on a study linking its use with hemorrhagic stroke in
women. Men may also be at risk (Kernan et al., 2000).
Antihistamines
such as diphenhydramine (Benadryl), ceti-rizine (Zyrtec), and fexofenadine
(Allegra) may be used if an al-lergic component is suspected. If the patient
continues to have symptoms after 7 to 10 days, the sinuses may need to be
irrigated and hospitalization may be required.
Nursing Management
TEACHING PATIENTS SELF-CARE
Patient
teaching is an important aspect of nursing care for the pa-tient with acute
sinusitis. The nurse instructs the patient about methods to promote drainage
such as inhaling steam (steam bath, hot shower, and facial sauna), increasing
fluid intake, and apply-ing local heat (hot wet packs). The nurse also informs
the patient about the side effects of nasal sprays and about rebound
conges-tion. In the case of rebound congestion, the body’s receptors, which
have become dependent on the decongestant sprays to keep the nasal passages
open, close and congestion results after the spray is discontinued.
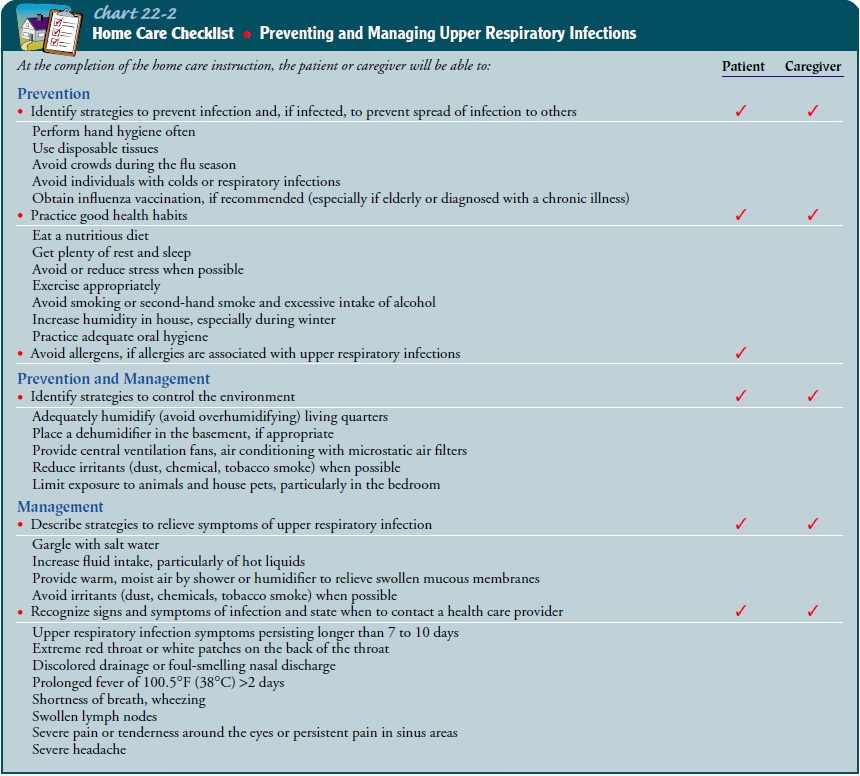
The
nurse stresses the importance of following the recom-mended antibiotic regimen,
because a consistent blood level of the medication is critical to treat the
infection. The nurse teaches the patient the early signs of a sinus infection
and recommends pre-ventive measures such as following healthy practices and
avoiding contact with people who have upper respiratory infections (see Chart
22-2).
The
nurse should explain to the patient that fever, severe headache, and nuchal
rigidity are signs of potential complica-tions. If fever persists despite
antibiotic therapy, the patient should seek additional care.
Related Topics