Chapter: Medical Surgical Nursing: Management of Patients With Upper Respiratory Tract Disorders
Cancer of the Larynx
Cancer of the Larynx
Cancer
of the larynx is a malignant tumor in the larynx (voice box). It is potentially
curable if detected early. It represents less than 1% of all cancers and occurs
about four times more fre-quently in men than in women, and most commonly in
persons 50 to 70 years of age. The incidence of laryngeal cancer contin-ues to
decline, but the incidence in women versus men continues to increase. Each year
in the United States, approximately 9,000 new cases are discovered, and 3,700
persons with cancer of the larynx will die (American Cancer Society, 2002).
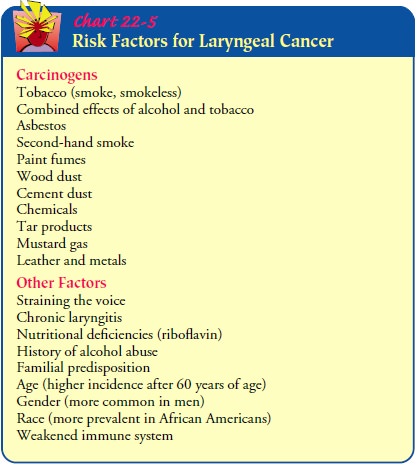
Carcinogens
that have been associated with the development of laryngeal cancer include
tobacco (smoke, smokeless) and alco-hol and their combined effects, exposure to
asbestos, mustard gas, wood dust, cement dust, tar products, leather, and
metals. Other contributing factors include straining the voice, chronic
laryngi-tis, nutritional deficiencies (riboflavin), and family predisposition
(Chart 22-5).
A malignant growth may occur in three different areas of the larynx: the glottic area (vocal cords), supraglottic area (area above the glottis or vocal cords, including epiglottis and false cords), and subglottis (area below the glottis or vocal cords to the cricoid). Two thirds of laryngeal cancers are in the glottic area. Supraglottic cancers account for approximately one third of the cases, sub-glottic tumors for less than 1%. Glottic tumors seldom spread if found early because of the limited lymph vessels found in the vocal cords (Lenhard, Osteen, & Gansler, 2001).
Clinical Manifestations
Hoarseness of more than 2 weeks’ duration is noted early in the patient with cancer in the glottic area because the tumor impedes the action of the vocal cords during speech. The voice may sound harsh, raspy, and lower in pitch. Affected voice sounds are not early signs of subglottic or supraglottic cancer. The patient may complain of a cough or sore throat that does not go away and pain and burning in the throat, especially when consuming hot liquids or citrus juices. A lump may be felt in the neck. Later symptoms include dysphagia, dyspnea (difficulty breathing), unilateral nasal obstruction or discharge, persistent hoarseness, persistent ulcera-tion, and foul breath. Cervical lymph adenopathy, unplanned weight loss, a general debilitated state, and pain radiating to the ear may occur with metastasis.
Assessment and Diagnostic Findings
An
initial assessment includes a complete history and physical ex-amination of the
head and neck. This will include assessment of risk factors, family history,
and any underlying medical condi-tions. An indirect laryngoscopy, using a
flexible endoscope, is initially performed in the otolaryngologist’s office to
visually eval-uate the pharynx, larynx, and possible tumor. Mobility of the
vocal cords is assessed; if normal movement is limited, the growth may affect muscle,
other tissue, and even the airway. The lymph nodes of the neck and the thyroid
gland are palpated to determine spread of the malignancy (Haskell, 2001).
If
a tumor of the larynx is suspected on an initial examination, a direct
laryngoscopic examination is scheduled. This examina-tion is done under local
or general anesthesia and allows evalua-tion of all areas of the larynx.
Samples of the suspicious tissue are obtained for histologic evaluation. The
tumor may involve any of the three areas of the larynx and may vary in
appearance.
Squamous
cell carcinoma accounts for over 90% of the cases of laryngeal carcinoma
(Haskell, 2001). The staging of the tumor serves as a framework for the
therapeutic regimen. The TNM classification system, developed by the American
Joint Commit-tee on Cancer (AJCC) (Chart 22-6), is the accepted method used to
classify head and neck tumors. The classification of the tumor determines the
suggested treatment modalities. Because many of these lesions are submucosal,
biopsy may require that an incision be made using microlaryngeal techniques or
using a CO2 laser to transect the mucosa and
reach the tumor.
Computed
tomography and magnetic resonance imaging (MRI) are used to assess regional
adenopathy and soft tissue and to help stage and determine the extent of a
tumor. MRI is also helpful in post-treatment follow-up in order to detect a
recur-rence. Positron emission tomography (PET scan) may also be used to detect
recurrence of a laryngeal tumor after treatment.
Medical Management
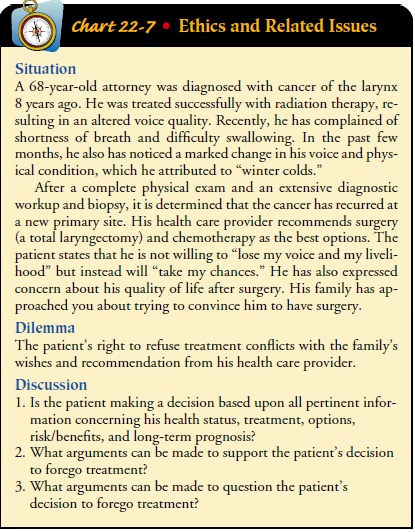
Treatment
of laryngeal cancer depends on the staging of the tumor, which includes the
location, size, and histology of the tumor and the presence and extent of
cervical lymph node in-volvement. Treatment options include surgery, radiation
therapy, and chemotherapy. The prognosis depends on a variety of factors: tumor
stage, the patient’s gender and age, and pathologic features of the tumor,
including the grade and depth of infiltration. The treatment plan also depends
on whether this is an initial diagno-sis or a recurrence. Small glottic tumors,
stage I and II, with no infiltration to the lymph nodes are associated with a
75% to 95% survival rate. Patients with stage III and IV or advanced tumors
have a 50% to 60% survival rate and have a 50% chance of re-currence and a 30%
chance of metastasis. The highest risk of la-ryngeal cancer recurrence is in
the first 2 to 3 years. Recurrence after 5 years is rare and is usually due to
a new primary malig-nancy (Lenhard et al., 2001) (Chart 22-7).
Surgery and radiation therapy are both effective methods in the early stages of cancer of the larynx. Chemotherapy tradition-ally has been used for recurrence or metastatic disease. It has also been used more recently in conjunction with either radiation therapy to avoid a total laryngectomy or preoperatively to shrink a tumor before surgery.
A complete dental examination is per-formed to rule out any oral
disease. Any dental problems are re-solved, if possible, prior to surgery. If surgery
is to be performed, a multidisciplinary team evaluates the needs of the patient
and family to develop a successful plan of care (Forastiere et al., 2001).
SURGICAL MANAGEMENT
Recent
advances in surgical techniques for treating laryngeal can-cer may minimize the
ensuing cosmetic and functional deficits. Depending on the location and staging
of the tumor, four differ-ent types of laryngectomy
(surgical removal of part or all of the larynx and surrounding structures) are
considered:
·
Partial laryngectomy
·
Supraglottic laryngectomy
·
Hemilaryngectomy
·
Total laryngectomy
Some
microlaryngeal surgery can be performed endoscopi-cally. The CO2
laser can be used for the treatment of many laryngeal tumors, with the
exception of large vascular tumors.
Partial Laryngectomy.
A
partial laryngectomy (laryngofissure–thyrotomy) is recommended in the early
stages of cancer in the glottic area when only one vocal cord is involved. The
surgery is associated with a very high cure rate. It may also be performed for
a recurrence when high-dose radiation has failed. A portion of the larynx is
removed, along with one vocal cord and the tumor; all other structures remain.
The airway remains intact and the pa-tient is expected to have no difficulty
swallowing. The voice qual-ity may change or the patient may be hoarse.
Supraglottic Laryngectomy.
A supraglottic laryngectomy is in-dicated in the management of
early (stage I) supraglottic and stage II lesions. The hyoid bone, glottis, and
false cords are re-moved. The true vocal cords, cricoid cartilage, and trachea
remain intact. During surgery, a radical neck dissection is performed on the
involved side. A tracheostomy tube is left in the trachea until the glottic
airway is established. It is usually removed after a few days and the stoma is
allowed to close. Nutri-tion is provided through a nasogastric tube until there
is healing, followed by a semisolid diet. Postoperatively, the patient may
ex-perience some difficulty swallowing for the first 2 weeks. Aspiration is a
potential complication since the patient must learn a new method of swallowing
(supraglottic swallowing). The chief ad-vantage of this surgical procedure is
that it preserves the voice, even though the quality of the voice may change.
Speech therapy is required before and after surgery. The major problem is the
high risk for recurrence of the cancer; therefore, patients are selected
carefully.
Hemilaryngectomy.
A
hemilaryngectomy is performed whenthe tumor extends beyond the vocal cord but
is less than 1 cm in size and is limited to the subglottic area. It may be used
in stage I glottic lesions. In this procedure, the thyroid cartilage of the
lar-ynx is split in the midline of the neck and the portion of the vocal cord
(one true cord and one false cord) is removed with the tumor. The arytenoid
cartilage and half of the thyroid are removed. The patient will have a
tracheostomy tube and nasogastric tube in place for 10 to 14 days following
surgery. The patient is at risk for aspiration postoperatively. Some change may
occur in the voice quality. The voice may be rough, raspy, and hoarse and have
lim-ited projection. The airway and swallowing remain intact.
Total Laryngectomy.
A
total laryngectomy is performed in themost advanced stage IV laryngeal cancer,
when the tumor extends beyond the vocal cords, or for recurrent or persistent
cancer fol-lowing radiation therapy. In a total laryngectomy, the laryngeal
structures are removed, including the hyoid bone, epiglottis, cricoid
cartilage, and two or three rings of the trachea. The tongue, pharyngeal walls,
and trachea are preserved. A total laryngec-tomy will result in permanent loss
of the voice and a change in the airway.
Many
surgeons recommend that a radical neck dissection be performed on the same side
as the lesion even if no lymph nodes are palpable because metastasis to the
cervical lymph nodes is common. Surgery is more difficult when the lesion
involves the midline structures or both vocal cords. With or without neck
dis-section, a total laryngectomy requires a permanent tracheal stoma because
the larynx that provides the protective sphincter is no longer present. The
tracheal stoma prevents the aspiration of food and fluid into the lower
respiratory tract. The patient will have no voice but will have normal swallowing.
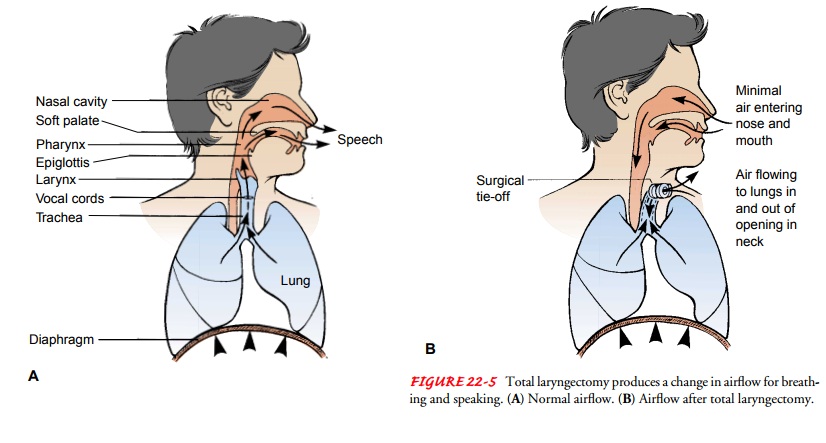
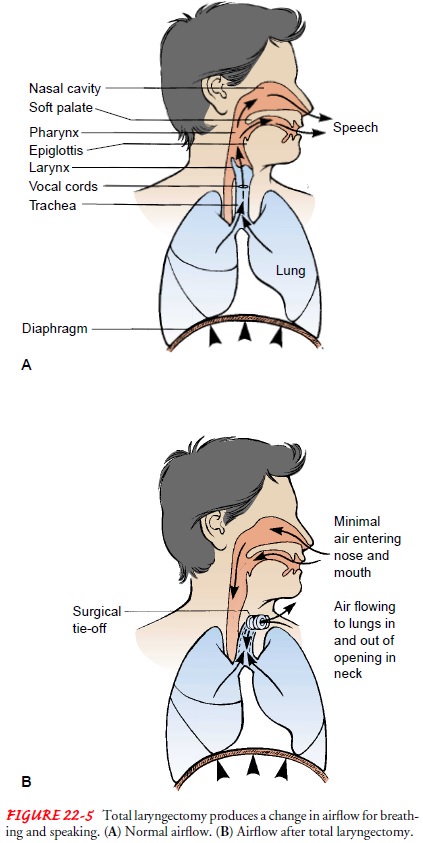
A total laryngectomy changes the manner in which airflow is used for breathing
and speaking, as depicted in Figure 22-5. Complications that may occur include
a salivary leak, wound infection from the develop-ment of a pharyngocutaneous
fistula, stomal stenosis, and dys-phagia secondary to pharyngeal and cervical
esophageal stricture.
RADIATION THERAPY
The
goal of radiation therapy is to eradicate the cancer and pre-serve the function
of the larynx. The decision to use radiation therapy is based on several
factors, including the staging of the tumor (usually used for stage I and stage
II tumors as a standard treatment option) and the patient’s overall health
status, lifestyle (including occupation), and personal preference. Excellent
results have been achieved with radiation therapy in patients with early-stage
(I and II) glottic tumors when only one vocal cord is in-volved and there is
normal mobility (ie, moves with phonation) and in small supraglottic lesions.
One of the benefits of radiation therapy is that patients retain a near-normal
voice. A few may de-velop chondritis (inflammation of the cartilage) or
stenosis; a small number may later require laryngectomy.
Radiation
therapy may also be used preoperatively to reduce the tumor size. Radiation therapy
is combined with surgery in ad-vanced (stages III and IV) laryngeal cancer as
adjunctive therapy to surgery or chemotherapy, and as a palliative measure. A
vari-ety of clinical trials have combined chemotherapy and radiation therapy in
the treatment of advanced laryngeal tumors. Early studies suggest that combined
modality therapy may improve the tumor’s response to radiation therapy.
Radiation therapy com-bined with chemotherapy may be an alternative to a total
laryn-gectomy.
The
complications from radiation therapy are a result of external radiation to the
head and neck area, which may also in-clude the parotid gland responsible for
mucus production. The symptoms may include acute mucositis, ulceration of the
mucous membranes, pain, xerostomia
(dry mouth), loss of taste, dys-phasia, fatigue, and skin reactions. Later
complications may in-clude laryngeal necrosis, edema, and fibrosis.
SPEECH THERAPY
The loss or alteration of speech is discussed with the patient and family before surgery, and the speech therapist conducts a pre-operative evaluation. During this time, the nurse should inform the patient and family about methods of communication that will be available in the immediate postoperative period. These include writing, lip speaking, and communication or word boards. A sys-tem of communication is established with the patient, family, nurse, and physician and implemented consistently after surgery.
A
postoperative communication plan is also developed. The three most common
techniques of alaryngeal communication
are esophageal speech, artificial larynx (electrolarynx), and
tra-cheoesophageal puncture. Training in these techniques begins once medical
clearance is obtained from the physician.
Esophageal Speech.
Esophageal
speech was the primary methodof alaryngeal speech taught to patients until the
1980s. The pa-tient needs the ability to compress air into the esophagus and
expel it, setting off a vibration of the pharyngeal esophageal seg-ment. The
technique can be taught once the patient begins oral feedings, approximately 1
week after surgery. First, the patient learns to
belch and is reminded to do so an hour after eating. Then the technique is
practiced repeatedly. Later, this conscious belching action is transformed into
simple explosions of air from the esophagus for speech purposes. Thereafter,
the speech thera-pist works with the patient in an attempt to make speech
intelli-gible and as close to normal as possible. Because it takes a long time
to become proficient, the success rate is low.
Electric Larynx.
If
esophageal speech is not successful, or untilthe patient masters the technique,
an electric larynx may be used for communication. This battery-powered
apparatus projects sound into the oral cavity. When the mouth forms words
(artic-ulated), the sounds from the electric larynx become audible words. The
voice that is produced sounds mechanical, and some words may be difficult to
distinguish. The advantage is that the patient is able to communicate with relative
ease while working to become proficient at either esophageal or
tracheoesophageal puncture speech.
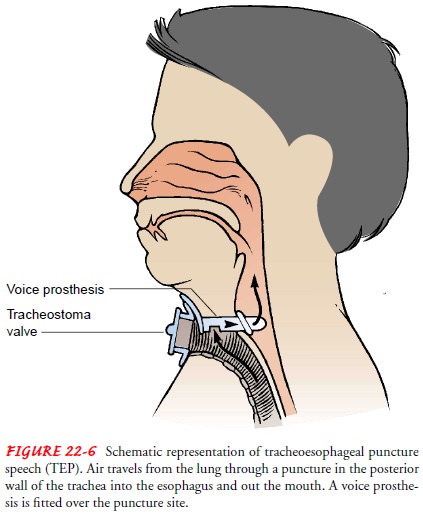
Tracheoesophageal Puncture.
The third technique of alaryngealspeech is tracheoesophageal
puncture (Fig. 22-6). This technique is the most widely used because the speech
associated with it most resembles normal speech (the sound produced is a
combination of esophageal speech and voice), and it is easily learned. A valve
is placed in the tracheal stoma to divert air into the esophagus and out of the
mouth. Once the puncture is surgically created and has healed, a voice
prosthesis (Blom–Singer) is fitted over the punc-ture site. To prevent airway
obstruction, the prosthesis is re-moved and cleaned when mucus builds up. A
speech therapist teaches the patient how to produce sounds. Moving the tongue
and lips to form the sound into words produces speech as before.
Tracheoesophageal speech is successful in 80% to 90% of pa-tients (DeLisa &
Gans, 1998).
Related Topics