Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Venous Thrombosis, Deep Vein Thrombosis (DVT), Thrombophlebitis, and Phlebothrombosis
Management of Venous Disorders
VENOUS
THROMBOSIS,DEEP VEIN THROMBOSIS (DVT), THROMBOPHLEBITIS,AND PHLEBOTHROMBOSIS
Although
the terms venous thrombosis, deep vein thrombosis(DVT),
thrombophlebitis, and
phlebothrombosis do not necessarilyreflect identical disease processes, for
clinical purposes, they are often used interchangeably.
Pathophysiology
Superficial
veins, such as the greater saphenous, lesser saphenous, cephalic, basilic, and
external jugular veins, are thick-walled mus-cular structures that lie just
under the skin. Deep veins are thin walled and have less muscle in the media.
They run parallel to ar-teries and bear the same names as the arteries. Deep and
su-perficial veins have valves that permit unidirectional flow back to the
heart. The valves lie at the base of a segment of the vein that is expanded
into a sinus. This arrangement permits the valves to open without coming into
contact with the wall of the vein, per-mitting rapid closure when the blood
starts to flow backward. Other kinds of veins are known as perforating veins.
These vessels have valves that allow one-way blood flow from the superficial
system to the deep system.
Although
the exact cause of venous thrombosis remains un-clear, three factors, known as
Virchow’s triad, are believed to play a significant role in its development:
stasis of blood (venous sta-sis), vessel wall injury, and altered blood
coagulation (Chart 31-6). At least two of the factors seem to be necessary for
thrombosis to occur. Venous stasis occurs when blood flow is reduced, as in
heart failure or shock; when veins are dilated, as with some med-ication
therapies; and when skeletal muscle contraction is reduced, as in immobility,
paralysis of the extremities, or anesthesia. Moreover, bed rest reduces blood
flow in the legs by at least 50%. Damage to the intimal lining of blood vessels
creates a site for clot formation. Direct trauma to the vessels, as with
fractures or dis-location, diseases of the veins, and chemical irritation of
the vein from intravenous medications or solutions, can damage veins.
In-creased blood coagulability occurs most commonly in patients who have been
abruptly withdrawn from anticoagulant medica-tions. Oral contraceptive use and
several blood dyscrasias (ab-normalities) also can lead to hypercoagulability.

Formation
of a thrombus frequently accompanies thrombo-phlebitis, which is an
inflammation of the vein walls. When a thrombus develops initially in the veins
as a result of stasis or hy-percoagulability but without inflammation, the
process is referred to as phlebothrombosis. Venous thrombosis can occur in any
vein but occurs more in the veins of the lower extremities. The superficial and
deep veins of the extremities may be affected.
Upper extremity venous thrombosis is not as common as lower extremity thrombosis. However, upper extremity venous throm-bosis is more common in patients with intravenous catheters or in patients with an underlying disease that causes hypercoagula-bility. Internal trauma to the vessels may result from pacemaker leads, chemotherapy ports, dialysis catheters, or parenteral nutrition lines.
The lumen of the vein may be decreased as a result of the catheter or
from external compression, such as by neoplasms or an extra cervical rib.
Effort thrombosis of the upper extremity is caused by repetitive motion, such
as experienced by competitive swimmers, tennis players, and construction workers,
that irritates the vessel wall, causing inflammation and subsequent thrombosis.
Venous
thrombi are aggregates of platelets attached to the vein wall, along with a
tail-like appendage containing fibrin, white blood cells, and many red blood
cells. The “tail” can grow or can propagate in the direction of blood flow as
successive layers of the thrombus form. A propagating venous thrombosis is
dangerous because parts of the thrombus can break off and produce an em-bolic
occlusion of the pulmonary blood vessels. Fragmentation of the thrombus can
occur spontaneously as it dissolves naturally, or it can occur in association
with an elevation in venous pressure, as occurs when a person stands suddenly
or engages in muscular activity after prolonged inactivity. After an episode of
acute deep vein thrombosis, recanalization of the lumen typically occurs. The
time required for complete recanalization is an important de-terminant of
venous valvular incompetence, which is one com-plication of venous thrombosis
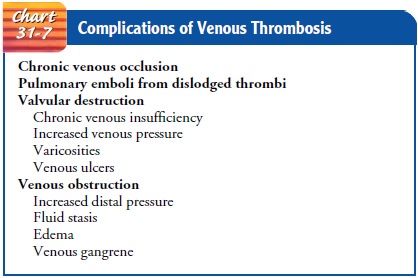
(Meissner et al., 2000). Other complications of venous thrombosis are listed in
Chart 31-7.
Clinical Manifestations
A
major problem associated with recognizing deep vein throm-bosis is that the
signs and symptoms are nonspecific. The excep-tion is phlegmasia cerulea dolens
(massive iliofemoral venous thrombosis), in which the entire extremity becomes
massively swollen, tense, painful, and cool to the touch. Despite this
vari-ability, clinical signs should always be investigated.
DEEP VEINS
With obstruction of the deep veins comes edema and swelling of the extremity because the outflow of venous blood is inhibited.
The
amount of swelling can be determined by measuring the cir-cumference of the
affected extremity at various levels with a tape measure and comparing one
extremity with the other at the same level to determine size differences. If
both extremities are swollen, a size difference may be difficult to detect. The
affected extremity may feel warmer than the unaffected extremity, and the
superficial veins may appear more prominent.
Tenderness,
which usually occurs later, is produced by in-flammation of the vein wall and
can be detected by gently pal-pating the affected extremity. Homans’ sign (pain
in the calf after the foot is sharply dorsiflexed) is not specific for deep
vein throm-bosis because it can be elicited in any painful condition of the
calf. In some cases, signs of a pulmonary embolus are the first indica-tion of
deep vein thrombosis.
SUPERFICIAL VEINS
Thrombosis
of superficial veins produces pain or tenderness, red-ness, and warmth in the
involved area. The risk of the superficial venous thrombi becoming dislodged or
fragmenting into emboli is very low because most of them dissolve
spontaneously. This condition can be treated at home with bed rest, elevation
of the leg, analgesics, and possibly anti-inflammatory medication.
Assessment and Diagnostic Findings
Careful
assessment is invaluable in detecting early signs of venous disorders of the
lower extremities. Patients with a history of vari-cose veins,
hypercoagulation, neoplastic disease, cardiovascular disease, or recent major
surgery or injury are at high risk. Other patients at high risk include those
who are obese or elderly and women taking oral contraceptives.
When
performing the nursing assessment, key concerns in-clude limb pain, a feeling
of heaviness, functional impairment, ankle engorgement, and edema; differences
in leg circumference bilaterally from thigh to ankle; increase in the surface
tempera-ture of the leg, particularly the calf or ankle; and areas of
tender-ness or superficial thrombosis (ie, cordlike venous segment). Homans’
sign (pain in the calf as the foot is sharply dorsiflexed) has been used
historically to assess for DVT. It is not a reliable or valid sign for DVT and
has no clinical value in the assessment of a patient for DVT.
Prevention
Venous
thrombosis, thrombophlebitis, and DVT can be pre-vented, especially if patients
who are considered at high risk are identified and preventive measures are
instituted without delay.Preventive measures include the application of elastic
compres-sion stockings, the use of intermittent pneumatic compression devices,
and special body positioning and exercise (discussed later in the section on nursing
management). A further method to prevent venous thrombosis in surgical patients
is administration of subcutaneous unfractionated or low molecular weight
heparin.
Medical Management
The
objectives of treatment for deep vein thrombosis are to pre-vent the thrombus
from growing and fragmenting (risking pul-monary embolism) and to prevent
recurrent thromboemboli. Anticoagulant therapy (administration of a medication
to delay the clotting time of blood, prevent the formation of a thrombus in
postoperative patients, and forestall the extension of a throm-bus after it has
formed) can meet these objectives, although anti-coagulants cannot dissolve a
thrombus that has already formed.
ANTICOAGULATION THERAPY
Measures
for preventing or reducing blood clotting within the vascular system are
indicated in patients with thrombophlebitis, recurrent embolus formation, and
persistent leg edema from heart failure. They are also indicated in elderly
patients with a hip fracture that may result in lengthy immobilization.
Unfractionated Heparin.
Unfractionated
heparin (heparin) is ad-ministered subcutaneously to prevent development of
deep vein thrombosis, or by intermittent intravenous infusion or continuous
infusion for 5 to 7 days to prevent the extension of a thrombus and the
development of new thrombi. Oral anticoagulants, such as warfarin (Coumadin),
are administered with heparin therapy. Medication dosage is regulated by
monitoring the partial throm-boplastin time, the international normalized ratio (INR), and the platelet count.
Low-Molecular-Weight Heparin.
Subcutaneous
low-molecular-weight heparin (LMWH) is an effective treatment for some cases of
deep vein thrombosis. It has a longer half-life than unfrac-tionated heparin,
so doses can be given in one or two subcuta-neous injections each day. Doses
are adjusted according to weight. LMWH prevents the extension of a thrombus and
development of new thrombi and is associated with fewer bleeding complica-tions
than unfractionated heparin. Because there are several prepa-rations, the
dosing schedule must be based on the product used and the protocol at each
institution. The cost is higher than for unfractionated heparin; however, LMWH
may be used safely in pregnant women, and the patients may be more mobile and
have an improved quality of life.
Thrombolytic Therapy.
Unlike the
heparins, thrombolytic (fibri-nolytic) therapy causes the thrombus to lyse and
dissolve in 50% of patients. Thrombolytic therapy (eg, tissue plasminogen
acti-vator [t-PA, alteplase, Activase], reteplase [r-PA, Retavase],
tenecteplase [TNKase], staphylokinase, urokinase, streptokinase) is given
within the first 3 days after acute thrombosis. Therapy initiated beyond 5 days
after the onset of symptoms is signifi-cantly less effective (Moore, 2002). The
advantages of throm-bolytic therapy include less long-term damage to the venous
valves and a reduced incidence of postthrombotic syndrome and chronic venous
insufficiency. However, thrombolytic therapy re-sults in approximately a
threefold greater incidence of bleeding than heparin. If bleeding occurs and
cannot be stopped, the thrombolytic agent is discontinued.
SURGICAL MANAGEMENT
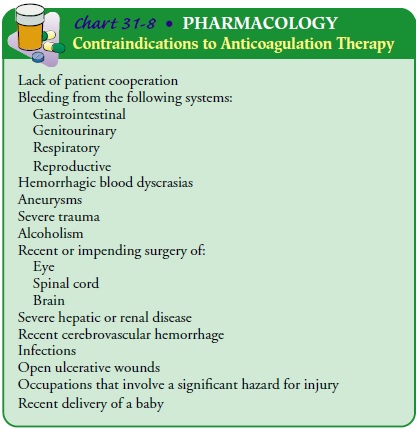
Surgery
is necessary for deep vein thrombosis when anticoagulant or thrombolytic
therapy is contraindicated (Chart 31-8), the danger of pulmonary embolism is
extreme, or the venous drainage is so severely compromised that permanent
damage to the ex-tremity will probably result. A thrombectomy (removal of the
thrombosis) is the procedure of choice. A vena cava filter may be placed at the
time of the thrombectomy; this filter traps large emboli and prevents pulmonary
emboli.
Nursing Management
If the
patient is receiving anticoagulant therapy, the nurse must frequently monitor
the partial thromboplastin time, prothrom-bin time, hemoglobin and hematocrit
values, platelet count, and fibrinogen level. Close observation is also
required to detect bleeding; if bleeding occurs, it must be reported
immediately and anticoagulant therapy discontinued.
ASSESSING AND MONITORING ANTICOAGULANT THERAPY
To
prevent inadvertent infusion of large volumes of heparin, which could cause
hemorrhage, continuous intravenous infusion by electronic infusion device is
the preferred method of adminis-tering unfractionated heparin. Dosage
calculations are based on the patient’s weight, and any possible bleeding
tendencies are detected by a pretreatment clotting profile. If renal
insufficiency exists, lower doses of heparin are required. Periodic coagulation
tests and hematocrit levels are obtained. Heparin is in the effec-tive, or
therapeutic, range when the partial thromboplastin time is 1.5 times the
control.
Intermittent
intravenous injection is another means of ad-ministering heparin; a dilute
solution of heparin is administered every 4 hours. Administration may be
facilitated by using a hep-arin lock, an intravenous catheter or a small,
butterfly-type scalp vein needle with an injection site at the end of the
tubing.
Oral anticoagulants, such as warfarin, are monitored by the prothrombin time or INR. Because their effect is delayed for 3 to 5 days, they are usually administered with heparin until desired anticoagulation has been achieved (ie, when the prothrombin time is 1.5 to 2 times normal or the INR is 2.0 to 3.0).
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Bleeding.
The principal complication of
anticoagulant therapyis spontaneous bleeding anywhere in the body. Bleeding
from the kidneys is detected by microscopic examination of the urine and is
often the first sign of anticoagulant toxicity from excessive dosage. Bruises,
nosebleeds, and bleeding gums are also early signs. To reverse the effects of
heparin promptly, intravenous injections of protamine sulfate may be
administered. Reversing the effects of warfarin, a coumarin derivative, is more
difficult, but effective measures that may be prescribed include vitamin K and
possibly transfusion of fresh frozen plasma.
Thrombocytopenia.
Another
complication of therapy may beheparin-induced thrombocytopenia (decrease in
platelets), which may develop in patients who receive heparin for more than 5
days or on readministration after a brief interruption of heparin therapy.
Beginning warfarin concomitantly with heparin can provide a stable INR or
prothrombin time by day 5 of heparin treatment.
The
use of LMWH is less frequently associated with heparin-induced
thrombocytopenia. The thrombocytopenia is thought to result from an immunologic
mechanism that causes aggregation of platelets. This serious complication
results in thromboembolic manifestations, and the prognosis is extremely
guarded.
Prevention
of thrombocytopenia depends on regular moni-toring of platelet counts. Early
signs of thrombocytopenia are a falling platelet count to less than 100,000/mL,
a decrease in platelet count exceeding 25% at one time, the need for increasing
doses of heparin to maintain the therapeutic level, thromboembolic or
hemorrhagic complications, and a history of heparin sensitivity (Stevens,
2000). If thrombocytopenia does occur, platelet aggre-gation studies are
conducted, the heparin is discontinued, and protamine sulfate is administered
to reverse heparin’s effects.
Drug Interactions.
Because oral
anticoagulants interact withmany other medications and herbal and nutritional
supplements, close monitoring of the patient’s medication schedule is
neces-sary. Medications and supplements that potentiate oral anticoag-ulants
include salicylates, anabolic steroids, chloral hydrate, glucagon,
chloramphenicol, neomycin, quinidine, phenylbuta-zone (Butazolidin), coenzyme
Q10, dong quai, garlic, gingko, ginseng, green tea, and vitamin E; those that
decrease the antico-agulant effect include phenytoin, barbiturates, diuretics,
estrogen, and vitamin C. It is advisable to identify medication interactions
for patients taking specific oral anticoagulants. Contraindications to
anticoagulant therapy are summarized in Chart 31-8.
PROVIDING COMFORT
Bed
rest, elevation of the affected extremity, elastic compression stockings, and
analgesics for pain relief are adjuncts to therapy. They help to improve
circulation and increase comfort. Depend-ing on the extent and location of a
venous thrombosis, bed rest may be required for 5 to 7 days after diagnosis.
This is approxi-mately the time necessary for the thrombus to adhere to the
vein wall, preventing embolization.
Warm,
moist packs applied to the affected extremity reduce the discomfort associated
with deep vein thrombosis, as do mild analgesics prescribed for pain control.
When the patient begins to ambulate, elastic compression stockings are used.
Walking is better than standing or sitting for long periods. Bed exercises,
such as dorsiflexion of the foot, are also recommended.
APPLYING ELASTIC COMPRESSION STOCKINGS
Elastic
compression stockings usually are prescribed for patients with venous
insufficiency. These stockings exert a sustained, evenly distributed pressure
over the entire surface of the calves, reducing the caliber of the superficial
veins in the legs and result-ing in increased flow in the deeper veins. The
stockings may be knee-high, thigh-high, or panty hose. Thigh-high stockings are
difficult for the patient to wear, because they have a tendency to roll down.
The roll of the stocking further restricts blood flow rather than the stocking
providing evenly distributed pressure over the thigh.
When
the stockings are off, the skin is inspected for signs of irritation, and the
calves are examined for possible tenderness. Any skin changes or signs of
tenderness are reported. Stockings are contraindicated in patients with severe
pitting edema because they can produce severe pitting at the knee.
Gerontologic Considerations
Because
of decreased strength and manual dexterity, elderly pa-tients may be unable to
apply elastic compression stockings prop-erly. If such is the case, a family
member or friend should be taught to assist the patient to apply the stockings
so that they do not cause undue pressure on any part of the feet or legs.
USING INTERMITTENT PNEUMATIC COMPRESSION DEVICES
These
devices can be used with elastic compression stockings to prevent deep vein
thrombosis. They consist of an electric con-troller that is attached by air
hoses to plastic knee-high or thigh-high sleeves. The leg sleeves are divided
into compartments, which sequentially fill to apply pressure to the ankle,
calf, and thigh at 35 to 55 mm Hg of pressure. These devices can increase blood
velocity beyond that produced by the stockings. Nursing measures include
ensuring that prescribed pressures are not exceeded and assessing for patient
comfort.
POSITIONING THE BODY AND ENCOURAGING EXERCISE
When
the patient is on bed rest, the feet and lower legs should be elevated
periodically above the level of the heart. This position al-lows the
superficial and tibial veins to empty rapidly and to re-main collapsed. Active
and passive leg exercises, particularly those involving calf muscles, should be
performed to increase venous flow. Early ambulation is most effective in
preventing venous sta-sis. Deep-breathing exercises are beneficial because they
produce increased negative pressure in the thorax, which assists in empty-ing
the large veins. Once ambulatory, patients are instructed to avoid sitting for
more than 2 hours at a time. The goal is to walk at least 10 minutes every 1 to
2 hours. Patients are also instructed to perform active and passive leg
exercises when they are not able to ambulate as frequently as necessary, such
as during long car, train, and plane trips.
PROMOTING HOME AND COMMUNITY-BASED CARE
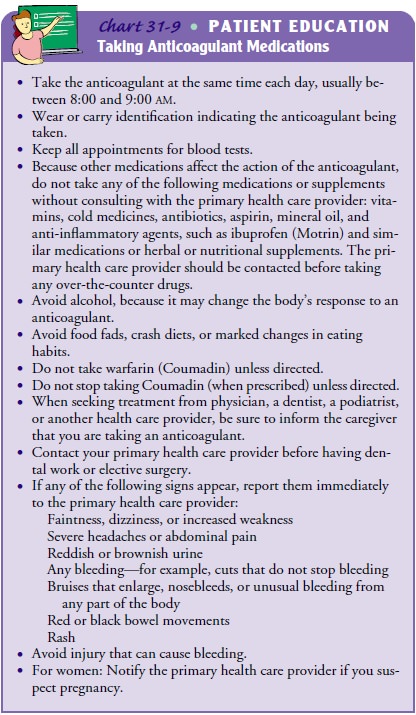
In
addition to teaching the patient how to apply elastic compres-sion stockings
and explaining the importance of elevating the legs and exercising adequately,
the nurse teaches about the medica-tion, its purpose, and the need to take the
correct amount at the specific times prescribed (Chart 31-9). The patient
should also be aware that blood tests are scheduled periodically to determine
whether a change in medication or dosage is required. If the pa-tient fails to
adhere to the therapeutic regimen, continuation of the medication therapy
should be questioned. A person who re-fuses to discontinue the use of alcohol
should not receive anti-coagulants because chronic alcohol use decreases their
effectiveness. In patients with liver problems, the potential for bleeding may
be exacerbated by anticoagulant therapy.
Related Topics