Chapter: Medical Surgical Nursing: Emergency Nursing
Substance Abuse - Emergency Nursing
Substance
Abuse
Substance abuse is the
misuse of specific substances to alter mood or behavior; drug and alcohol abuse
are two examples of sub-stance abuse. Drug abuse is the use of drugs for other
than legit-imate medical purposes. People who use drugs often take a variety of
drugs simultaneously (such as alcohol, barbiturates, opioids, and
tranquilizers), and the combination may have additive and addictive effects.
IV/injecting drug users are at increased risk for HIV infection, acquired
immunodeficiency syndrome (AIDS), and hepatitis B and are the most frequent
victims of tetanus in the United States.
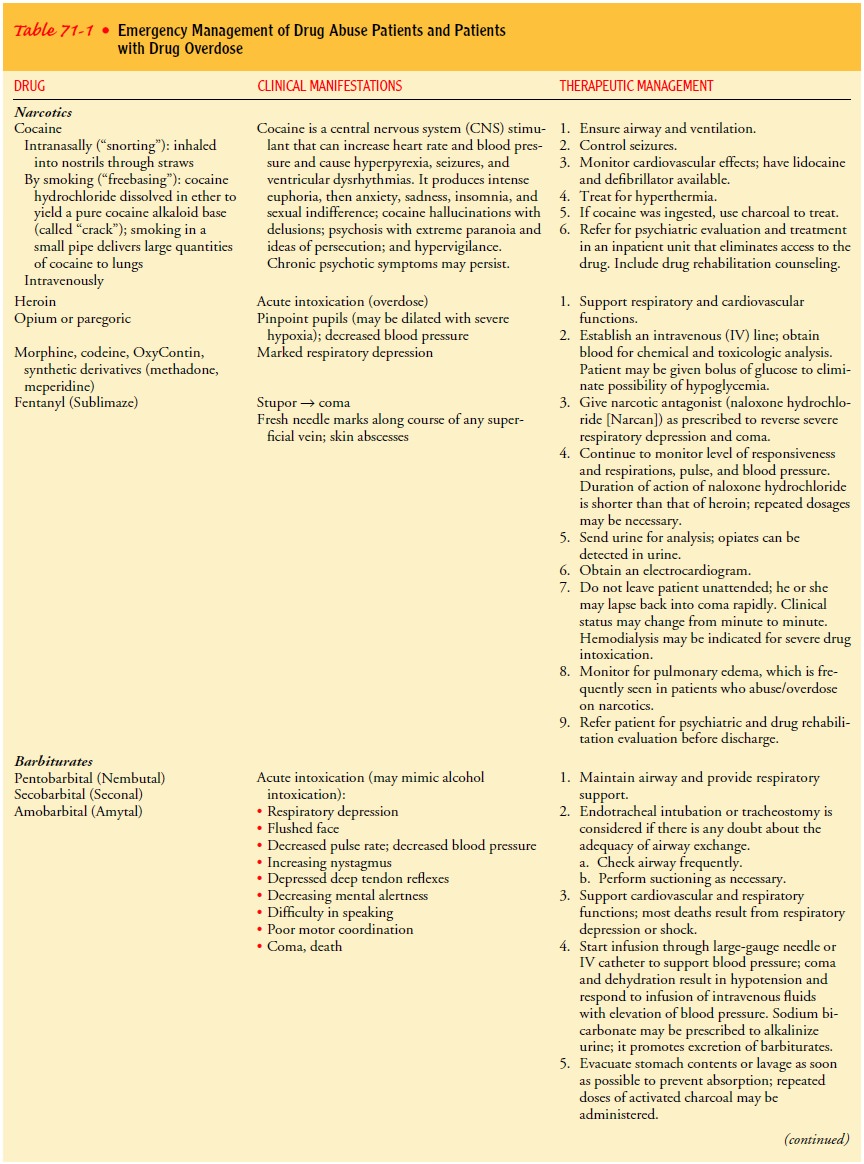
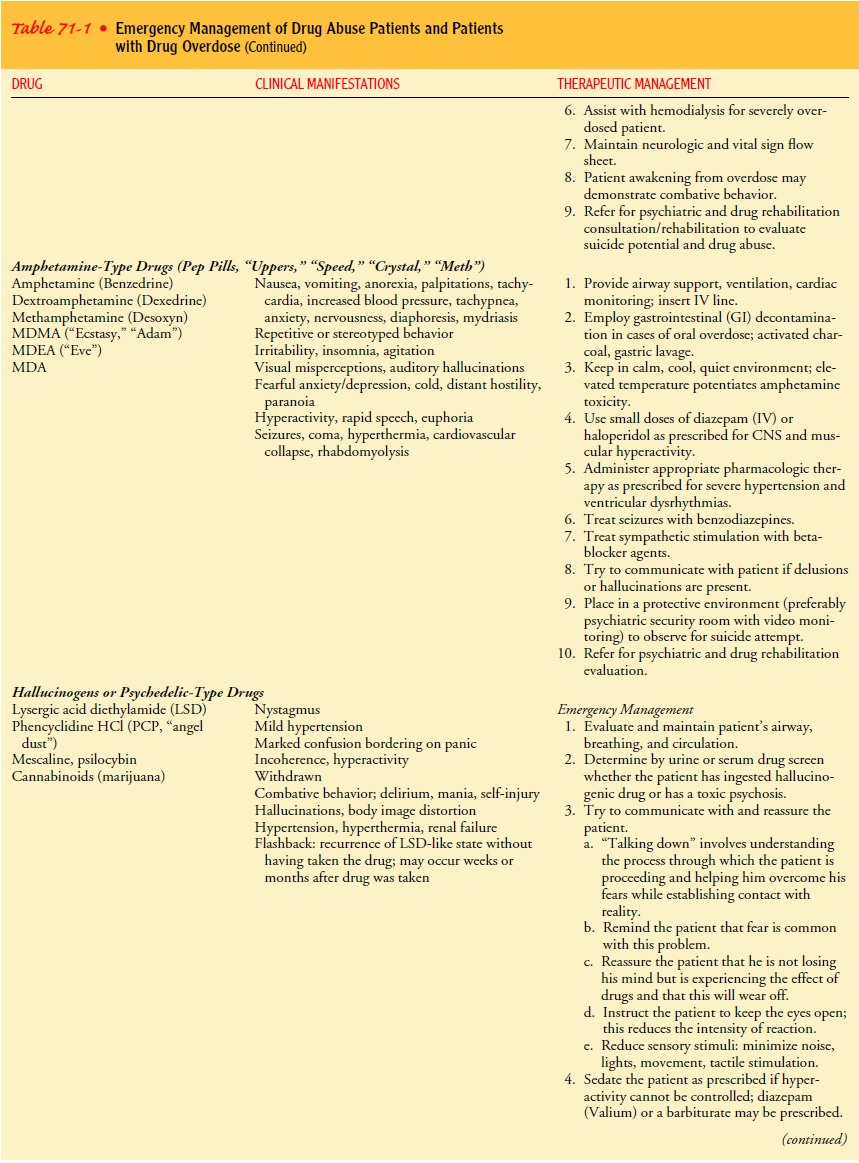
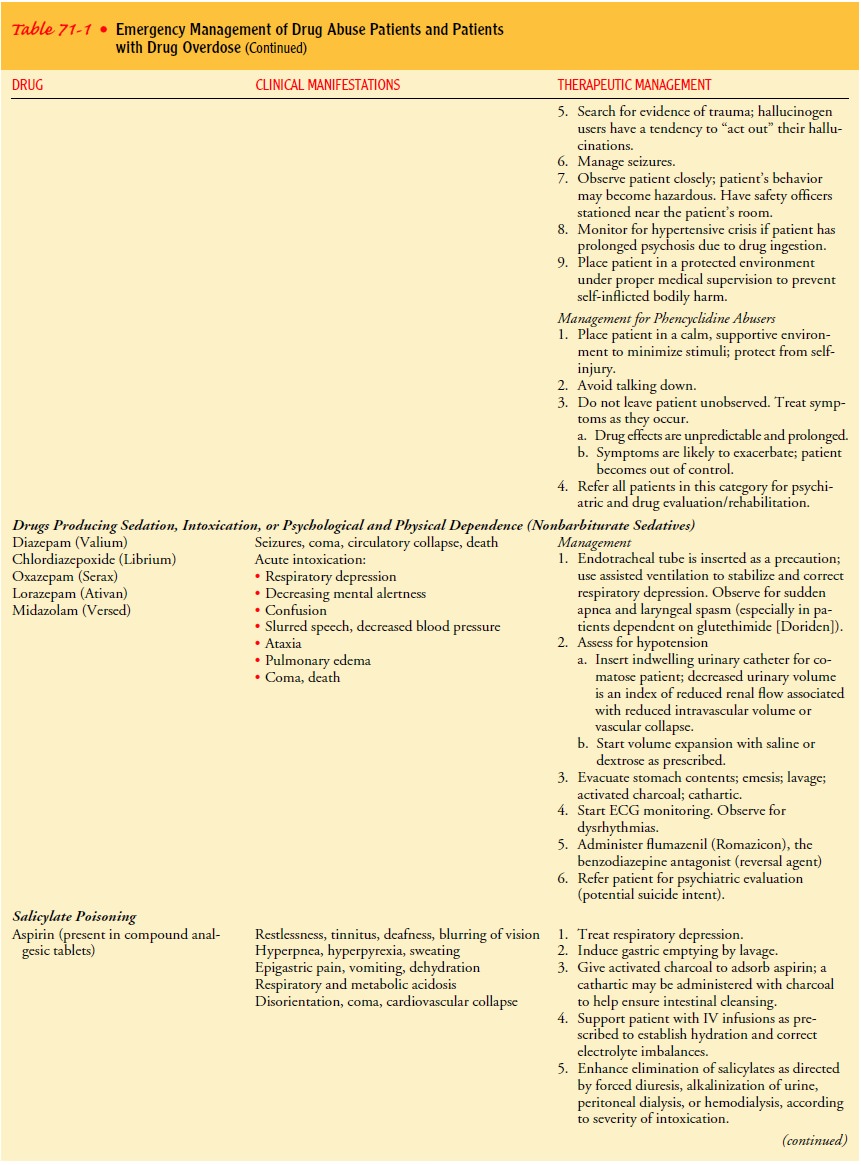
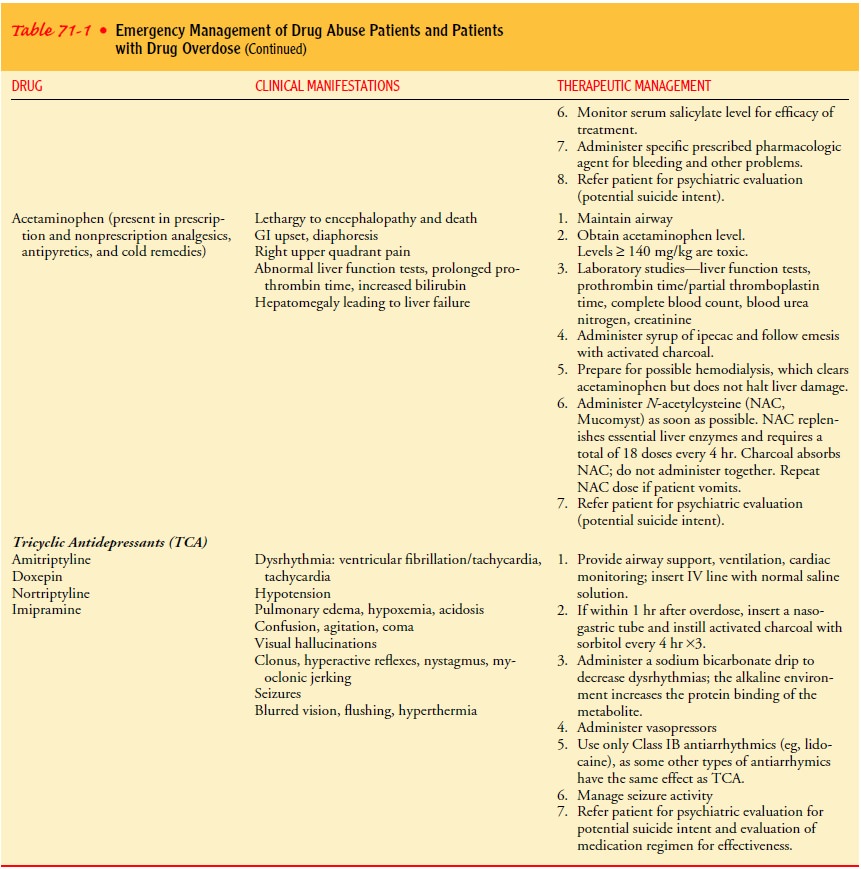
Clinical manifestations
vary with the substance used, but the underlying principles of management are
essentially the same. Table 71-1 identifies commonly abused drugs, listing
their clin-ical manifestations and therapeutic management. Treatment goals for
a patient suffering from drug overdose are to support the respiratory and
cardiovascular functions, to enhance clearance of the agent, and to provide for
safety of the patient and staff.
ACUTE ALCOHOL INTOXICATION
Alcohol is a psychotropic drug that affects mood,
judgment, behavior, concentration, and consciousness. Many heavy drinkers are
young adults or people older than 60 years of age. There is a high prevalence
of alcoholism among ED patients. Because pa-tients who abuse alcohol return
frequently to the ED, they often frustrate and tax the patience of the health
care professionals who care for them. Their management requires patience and
thought-ful, accurate, long-term treatment.
Alcohol, or ethanol, is a direct multisystem toxin and
CNS depressant that causes drowsiness, incoordination, slurring of speech,
sudden mood changes, aggression, belligerence, grandios-ity, and uninhibited
behavior. In excess, it also can cause stupor, coma, and death. In the ED, the
patient is assessed for head in-jury, hypoglycemia (which mimics intoxication),
and other health problems. Possible nursing diagnoses include ineffective
breathing pattern related to CNS depression and risk for violence
(self-directed or directed at others) related to severe intoxication from
alcohol.
Management
Treatment involves
detoxification of the acute poisoning, recovery, and rehabilitation. Commonly,
the patient uses mechanisms of denial and defensiveness. The nurse should
approach the patient in a nonjudgmental manner, using a firm, consistent,
accepting, and reasonable attitude. Speaking in a calm and slow manner is
helpful because alcohol interferes with thought processes. If the patient
appears intoxicated, hypoxia, hypovolemia, and neuro-logic impairment must be
ruled out before it is assumed that the patient is intoxicated. Typically, a
blood specimen is obtained for analysis of the blood alcohol level.
If drowsy, the patient
should be allowed to sleep off the state of alcoholic intoxication. During this
time, maintenance of a patent airway and observation for symptoms of CNS
depression are essential. The patient should be undressed and kept warm with
blankets. On the other hand, if the patient is noisy or belligerent, sedation
may be necessary. If sedation is used, the patient shouldbe
monitored carefully for hypotension and decreased level of consciousness.
Additionally, the
patient is examined for alcohol withdrawal delirium and also for injuries and
organic disease, such as head injury, seizures, pulmonary infections,
hypoglycemia, and nutri-tional deficiencies, that may be masked by alcoholic
intoxication. People with alcoholism suffer more injuries than the general
pop-ulation. Also, acute alcohol intoxication is the cause of trauma for many
nonalcoholic patients. Pulmonary infections are also more common in patients
with alcoholism, resulting from respiratory depression, an impaired defense
system, and a tendency toward aspiration of gastric contents. The patient may
show little in-crease in temperature or white blood cell count. The patient may
be hospitalized or admitted to a detoxification center in an effort to examine
problems underlying substance abuse.
ALCOHOL WITHDRAWAL SYNDROME/DELIRIUM TREMENS
Alcohol withdrawal
syndrome (AWS) is an acute toxic state that occurs as a result of sudden
cessation of alcohol intake after a bout of heavy drinking or, more usually,
after prolonged intake of al-cohol. Severity of symptoms depends on how much
alcohol was ingested and for how long. Delirium tremens may be precipitated by
acute injury or infection (pneumonia, pancreatitis, hepatitis) and is the most
severe form of AWS.
Patients with AWS show
signs of anxiety, uncontrollable fear, tremor, irritability, agitation,
insomnia, and incontinence. They are talkative and preoccupied and experience
visual, tactile, olfactory, and auditory hallucinations that often are
terrifying. Autonomic overactivity occurs and is evidenced by tachycardia,
dilated pupils, and profuse perspiration. Usually, all vital signs are elevated
in the alcoholic toxic state. Delirium tremens is a life-threatening condition
and carries a high mortality rate.
Management
The goals of management
are to give adequate sedation and support to allow the patient to rest and
recover without danger of injury or peripheral vascular collapse. A physical
examination is performed to identify preexisting or contributing illnesses or
injuries (eg, head injury, pneumonia). A drug history is obtained to elicit
informa-tion that may facilitate adjustment of any sedative requirements.
Baseline blood pressure is determined, because the patient’s sub-sequent
treatment may depend on blood pressure changes.
Usually, the patient is
sedated as directed with a sufficient dosage of benzodiazepines to establish
and maintain sedation, which reduces agitation, prevents exhaustion, prevents
seizures, and promotes sleep. The patient should be calm, able to respond, and
able to maintain an airway safely on his or her own. A vari-ety of medications
and combinations of medications are used (for example, chlordiazepoxide
[Librium], lorazepam, and clonidine). Haloperidol or droperidol may be
administered for severe acute AWS. Dosages are adjusted according to the
patient’s symptoms (agitation, anxiety) and blood pressure response.
The patient is placed in a calm, nonstressful environment (usually a private room) and observed closely. The room remains lighted to minimize the potential for illusions and hallucinations. Homicidal or suicidal responses may result from hallucinations. Closet and bathroom doors are closed to eliminate shadows. Some-one is designated to stay with the patient as much as possible. The presence of another person has a reassuring and calming effect, which helps the patient maintain contact with reality.
Any visual misrepresentations (illusions) are
explained, to orient the patient to reality.Fluid losses may result from
gastrointestinal losses (vomiting), profuse perspiration, and respiration
(hyperventilation). In addi-tion, the patient may be dehydrated as a result of
alcohol’s effect of decreasing antidiuretic hormone. The oral or intravenous
route is used to restore fluid and electrolyte balance.
Temperature, pulse, respiration, and blood pressure are
recorded frequently (every 30 minutes in severe forms of delirium) in
an-ticipation of peripheral circulatory collapse or hyperthermia (the two most
lethal complications). Phenytoin (Dilantin) or other antiseizure medications
may be prescribed to prevent or control repeated withdrawal seizures.
Frequently seen
complications include infections (eg, pneu-monia), trauma, hepatic failure,
hypoglycemia, and cardiovascu-lar problems. Hypoglycemia may accompany alcohol
withdrawal, because alcohol depletes liver glycogen stores and impairs
gluco-neogenesis; many patients with alcoholism also are malnourished.
Parenteral dextrose may be prescribed if the liver glycogen level is depleted.
Orange juice, Gatorade, or other forms of carbohydrates are given to stabilize
the blood glucose level and counteract tremu-lousness. Supplemental vitamin
therapy and a high-protein diet are provided as prescribed to counteract
vitamin deficiency. The patient should be referred to an alcoholic treatment
center for follow-up care and rehabilitation.
Related Topics