Chapter: Medicine Study Notes : Renal and Genitourinary
Urinary Tract Infections
Urinary Tract Infections
Investigations
·
Dipstick: Under-rated
o Nitrites (produced by an enzyme in most
infectious bacteria which breaks nitrates down to nitrites) Þ
presumptive diagnosis
o If no leukocytes, nitrates, protein or blood then no infection. Ie high
negative predictive value. Positive predictive value only about 30 – 40%
o Culture should be done (ie not just dipstick) in pregnancy, diabetics,
atypical presentations recurrent attacks and non-response to treatment
·
Urine Microscopy:
o Some RBC and WBCs are normal
o Look for casts, crystals, bacteria.
Absence of bacteria not significant (treat empirically)
o If RBC > WBC then ?stone
·
Culture:
·
Bacteruria Þ 10E5
colony forming units (cfu) per ml of urine. However, this was set using morning
samples in young women via catheterisation Þ not much value.
o In kids, a much smaller number may be significant, especially if:
§ In a boy
§ Obtained by catheter. In a
supra-pubic aspirate any growth is important
o Most UTIs are caused by a single bug. If multiple organisms then
contaminated sample. Bugs can grow in transit ® send to
lab straight away or refrigerate
o Antibiotic sensitivity: if multi-resistant then usually from Asia where
antibiotics are freely available
·
Haematuria in 50% - but if
asymptomatic ® ?bladder carcinoma
·
Intravenous pyleogram / urogram
(same thing)
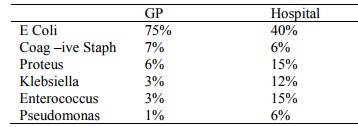
Microbiology
·
Hospital acquired are more
antibiotic resistant
·
Pathogenesis: bacterial adherence
o Uropathic strains: fimbriae – microbial adhesions. Different types in
different bugs, and different densities of receptors in hosts ® genetic
predisposition
o Catheter adhering strains:
§ Tightly adherent ® none grown from urine
§ Thick layer of „biofilm‟ forms in lumen of catheter containing bugs.
Antibiotics can‟t penetrate Þ change catheter
§ Risk factors: duration of use (but regular changing makes it worse), female sex,
absence of systemic antibiotics, catheter care violations
§ Prevention: avoid catheterisation, lots of fluid, alternative method for
bladder drainage (eg condom catheter), closed, sterile bladder drainage,
appropriate aseptic technique at insertion
Adults
·
Epidemiology:
o More common in women, older people, and long term care
o 20% in women 65 – 75, 3% of men
·
Definition: Lots of terms with
subtle variations in meaning: UTI, bacteruria, bladder bacteruria,
asymptomatic, etc, etc
·
Presentation:
o Acute symptomatic urinary infection = urgency, frequency and dysuria
(pain on urination). NB urgency and frequency may be unrelated to infection (eg
bladder instability)
o In elderly may present atypically: delirium, falls, immobility
o Cloudy urine, dark urine (volume depletion), and smelly urine are all normal!
o Asymptomatic bacteruria = 2 consecutive positive cultures without
symptoms attributable to the urinary tract
·
Classification:
o Uncomplicated: normal urinary tract and normal renal function
o Complicated if:
§ Abnormal urinary tract: eg calculi, reflux, obstruction, paraplegia,
catheter, prostatitis, etc
§ Impaired host defences: immunosuppressed, diabetes, etc
§ Impaired renal function
§ Virulent organism (eg Proteus)
§ Male
·
Causes of dysuria:
o Urinary tract infection +/- vaginitis
o Vaginitis (Candida albicans, trichomonas vaginalis, gardnerella vaginalis)
o STDs
o Other: trauma, urethral syndrome
·
Treatment:
o Oral trimethoprim in uncomplicated infections. E coli resistance ® will
need to change this soon
o Oral quinolones are the main second line agents (eg norfloxacine)
o Don’t treat asymptomatic positive urine cultures (ie don‟t test unless
symptoms) unless diabetic or pregnant
o Single dose therapy is worse than conventional therapy (7 – 10 days).
For adult women, single does therapy has an odds ratio compared to conventional
treatment (5 days or more) of 0.7 for TMP/SMZ (trimethoprim/sulphamethoxazole),
and 0.4 for amoxycillin
o Short course possibly as effective as conventional (watch this space)
·
Complications: Ascending
infection ® renal scarring ® hypertension, etc
· Prophylaxis:
o Consider if recurrent infections, eg low dose nightly antibiotics for 3
– 6 months, post-coital antibiotics
o Bladder emptying at night and after intercourse
o Topical oestrogen cream if post-menopausal
o Adequate fluid intake (> 2 litres per day)
·
Men:
o If unknown cause - ?referral to urologist for kidney scan (e.g. stone)
o Always do urine culture in addition to antibiotics
o Do swab if discharge
Urethral syndrome
·
No bacteria isolatable
·
Can be chlamydia (need to do
right test)
· Can become very sensitive after a number of infections (general inflammation)
·
Acidic urine will hurt more if
inflamed ® drink lots (dilute urine) and Uracil
·
More common in older women
UTIs in Children
·
Epidemiology:
o UTI is common:
§ Males usually have them in their first year, for girls it‟s on going
§ By age 7, 9% of girls and 2% of boys will have had at least one episode
o Caused by E coli in over 80% of cases. Others are associated with
complicated UTIs or long term antibiotic therapy (eg Candida)
o Of 1000 kids with UTI:
§ 400 have vesico-ureteric reflux, 100 have renal scars, 10 will develop premature hypertension (eg in older childhood or pregnancy), end stage renal failure in 1
§ 10 – 20 will have obstruction due to urethral valves, VU or PUJ
obstruction
§ Greatest risk usually kids < 4 and especially in first year of life
·
Risk Factors for UTI:
o Previous infection
o Normal anatomy but functional problem: e.g. vesico-urethral reflux (in child, sibling or parent)
o Structural abnormality: e.g. urethral stenosis/stricture (more common in
boys – congenital, trauma or inflammation)
o Vulvoanitis from poor perineal hygiene
o Incomplete or infrequent voiding
o In first year of life, uncircumcised male is 10 times that of circumcised
o Sexual abuse: only 2% of patients investigated for sexual abuse have UTI as a symptom. UTI without other indications (lesions, bleeding, bruising) is very unlikely to be sexual abuse
o Antibiotics: disrupt normal peri-urethral flora ®
predispose to infection
o Constipation a risk factor: ask about this
o Indwelling catheter
·
Risk factors for VUR:
o Children with UTI (30 – 40%)
o Siblings affected
o Antenatal dilation of the urinary tract (8 – 22%)
o No evidence that prophylaxis ® ¯renal scars (controversial)
·
Always have appendicitis as
differential diagnosis: can have white cells in urine with appendicitis where
appendix is in the pelvis (or elsewhere)
·
Symptoms are highly variable:
o 0 – 2: Fever/hypothermia (?sepsis), lethargy, poor feeding, diarrhoea,
vomiting, abdominal distension, failure to thrive
o 2 – 5: fever, rigours, vomiting, diarrhoea, colic, abdominal pain, some
dysuria, offensive urine, haematuria, weak urine stream
o 5 – 12: fever, rigours, abdominal pain (Þ upper
tract infection), dysuria, frequency, urgency, incontinence, haematuria
o If systemic illness then likelihood of pyelonephritis as
well as cystitis. If under one, can have Pyelonephritis without systemic signs ® if UTI
under age 1 then presume Pyelonephritis
·
Diagnosis:
o Urine bag:
§ Wash genitalia before application
§ Test with urine dipstick. If positive, obtain definitive sample with
catheter or supra-pubic aspiration (SPA)
§ Do not routinely send bag specimens for culture. Boys have 93% false
positive
o Catheter:
§ For children who can‟t void on request and where the bladder is in the
pelvis (SPA won‟t work)
§ Uncomfortable. Discard first few
mls
§ Growth > 10E6/litre suggest infection
o Supra-pubic aspirate:
§ If child too young to obtain an MSU
§ Gold standard: any growth suggests infection (but beware contamination
with skin commensals)
o MSU: discard first few mls
·
Exam:
o Often normal, other than fever
o Do blood pressure, search for
loin, abdominal and supra-pubic tenderness, inspect spine and external
genitalia, and brief neuro exam of the lower limbs. Check and plot growth
·
Management:
o Admitted for IV antibiotics if:
§ Neonate or immunocompromised
§ Shocked
§ Vomiting frequently (ie oral antibiotics won‟t stay down)
o Hospital treatment:
§ Bloods: FBC, blood cultures, electrolytes and Cr. If toxic, consider LP and glucose
§ Antibiotics: Amoxycillin 50 mg/kg/6hr (max 2g) (for enterococcus) and gentamicin 2.5 mg/kg/8hr (if older than 1 week and normal renal function) to cover everything else.
§ Discharge on oral antibiotics to take total treatment to 10 – 14 days.
Then prophylaxis until follow-up
§ Repeat urines to check it‟s cleared
§ Follow-up:
· US within, say, 12 hours: checking for obstruction and kidney size. Poor sensitivity for reflux
· If < 2 years then MCU (Miturocysto-urethrogram, for reflux ® risk of scarring) + delayed DMSA scan (eg after 6 months, look for filling defects ® renal scarring)
·
If > 2 years then delayed DMSA
§ If reflux, then prophylactic antibiotics until out of nappies and 6
months since last UTI
o Oral Antibiotic treatment:
§ Don‟t give antibiotics unless a definitive urine specimen has been
obtained
§ Antibiotics standard treatment:
·
Cotrimoxazole 200/40mg in 5 ml, 0.5 ml/kg bd 5 days (= trimethoprim + sulphamethoxazole
– less concern about allergy in kids),
·
Amoxycillin 15 mg/kg tds po (max
500 mg) for 5 days
· Augmentin 15 mg/kg tds po (max 500 mg) for 5 days
§ Prophylaxis in children with recurrent infection is common – but
duration, drug and dose all remain variable. Cotrimoxazole 200/40mg in 5 ml, 0.25 ml/kg po od
·
Repeat urines at conclusion of
antibiotics to check it‟s cleared
·
Referral to urologist:
o Boys: always refer for confirmed UTI, especially if circumcised
o Girls: At least repeat urines after first UTI to check cleared. Refer after second UTI
Related Topics