Chapter: Medicine Study Notes : Renal and Genitourinary
Glomerulonephritis - Kidney Disease
Glomerulonephritis
Overview
· Variety of conditions ® inflammatory changes in the glomeruli. If severe enough to cause crescent formation Þ rapidly progressive glomerulonephritis
·
Some forms predominantly present
in one way, but any form can present in any way. Can present as:
o Nephritic Syndrome
o Nephrotic Syndrome
o Acute Renal Failure secondary to rapidly progressive GN
o Chronic Renal Failure
o Asymptomatic Haematuria or proteinuria
o Hypertension
·
Either:
o Primary: limited to the kidney
o Secondary: part of a more widely disseminated immune process
·
Systemic diseases that may
present as GN:
o Lupus nephritis: deposits of immune complexes everywhere within the
glomerulus
o Arteritis: Microscopic polyarteritis
o Amyloid: Nephrotic Syndrome or renal failure. Histology with Congo Red Stain
o Diabetes
o Hypertension
·
Terminology:
o Proliferative: proliferation of endogenous glomeruli cells
o Exudative: infiltration by polymorphs
o Diffuse: involves all glomeruli
o Focal: involves only some glomeruli
o Global: involves the whole glomerular tuft
o Segmental: involves only part of the glomerular tuft
· Diagnosis:
o Urine biochemistry: urine sodium > 20 mmol/L (if pre-renal failure
then < 20, ie frantically trying to reabsorb Na)
o Urine analysis: Blood morphology and casts, protein (usually mild)
o Ultrasound: exclude obstruction, looking for normal or slightly enlarged
kidneys, echogenic (dark on US Þ fluid)
o CXR: look for Goodpastures Syndrome, Wegener‟s Granulomatosis
o Bloods: ANA (connective tissue disorders), ANCA (Anti-neutrophil cytoplasmic antigen Þ
o Wegener‟s Granulomatosis), Anti-dsDNA (Þ SLE),
anti-GBM
· Histology. May see:
o Glomerula epithelial cells usually have interdigitating foot processes. If they swell, ¯ gaps between them ® proteinuria
o Mesangial cells (supporting framework) are the first to react to injury
and the last to return to normal
Management
·
Investigations:
o Urine microscopy
o 24 hour urine for protein and Cr
o Serum: U&E, FBC, ESR, CRP, albumin, ANAs, etc
o Culture: ?blood, throat, ears, skin
o CXR, US, IVU
o Biopsy
·
Treatment:
o Prompt referral
o Keep BP < 145/90
o Specific treatment
o Monitor renal function
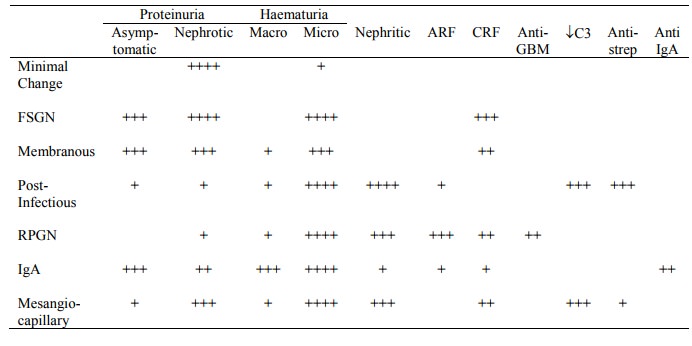
Clinical and lab features
Minimal Change Disease
· Presentation:
o Usually nephrotic syndrome, with severe oedema, uncommonly have
hypertension and 10% have microscopic haematuria
o Commonly after an URTI
o Boys > girls
o 90% of childhood nephrotic syndrome, 20 – 30% of adult nephrotic
syndrome
o Renal function normal, unless it deteriorates secondary to hypovolaemia
o Weak association with Hodgkin‟s Disease
·
Investigations:
o Light Microscopy (LM): glomeruli are normal
o Immunoflourescence (IF): Negative
o Electron Microscopy (EM): fusion of foot processes
·
Management:
o Kids: natural history unpredictable:
§ 90% of kids respond to 8 weeks of steroids. If they relapse, respond to steroids again (eg triggered by intercurrent illness). No renal failure but complications of treatment
§ 10% become steroid dependent or resistant ® use
cyclosporin
o Steroids less effective in adults, but still reasonable response rate
Focal and Segmental Glomerulosclerosis (FSGS)
·
Presentation:
o Usually nephrotic, can be nephritic
o Usually microscopic haematuria
o Accounts for 10 – 20% of nephrotic syndrome in adults
· Investigations:
o LM: segmental sclerosis of the glomerular tufts. May be mesangial matrix, interstitial fibrosis and tubular atrophy
o IF: Weakly positive for IgM and C3 (?artefact)
·
Management:
o Poor prognosis: 50% have a five year renal survival
o Some response but frequent relapse to steroids
Membranous Glomerulonephritis
·
Presentation:
o Nephrotic syndrome, also asymptomatic proteinuria
o Microscopic haematuria, hypertension, renal impairment
o 30% of adult nephrotic syndrome, most commonly middle-aged
·
Usually idiopathic, but 25% of it
is secondary to underlying disease, including:
o Lung or colon cancer (< 10% or adults presenting with Membranous GN)
o Infections: hepatitis B, malaria
o SLE
o Drugs: penicillamine, gold, high dose captopril
·
Investigations:
o Is autoimmune – but there is no antibody you can measure
o LM: thickened, irregular capillary loops, spikes in BM with silver stain
o IF: granular deposition of IgG and C3
o EM: Subepithelial deposits
· Prognosis: variable – 30% progress to end-stage, 30% improve, and the rest retain stable renal function but with ongoing proteinuria
·
Treatment: steroids or cytotoxics
for the progressive group
Post-Infectious Glomerulonephritis
· 8 – 14 days following Group A b-haemolytic strep infection of throat or skin, also SBE, osteomyelitis, etc
· Cultures usually negative, strep serology may be helpful
·
Presentation: Usually nephritic,
may be rapidly progressing ® acute renal failure
·
Biopsy: usually in adults to rule
out a crescentic rapidly progressive GN:
o LM: mesangial and endothelial cell proliferation + neutrophils. Crescents if
severe
o IF: Usually +ive for granular IgG and C3 deposition
·
Treatment: supportive, not immunosuppressive. Treat culture positive family members with
penicillin
·
Prognosis: slow recovery, mild
residual impairment in a few
Goodpasture’s Syndrome
· GN +/- pulmonary involvement (ranging from pulmonary infiltrate on x-ray to frank haemoptysis)
· Pathogenesis: antibodies against an antigen in the glomerular basement membrane and pulmonary tissue
·
Biopsy: Crescents + linear
immunoflourescence on the basement membrane
·
Can measure serum anti-GBM
antibody
· Treatment: immunosuppression (steroids, cyclophosphamide) +/- plasmapheresis
Mesangial IgA disease (Berger’s Disease)
·
Most common form of GN. Common
cause of recurrent haematuria in young men. Usually more benign
·
Presentation, either:
o Macroscopic haematuria +/- URTI (= Synpharyngetic haematuria)
o Asymptomatic microscopic haematuria picked up on dipstick testing
o Nephrotic levels of proteinuria are rare
·
Biopsy:
o LM: Mesangial cell
proliferation + matrix formation
o IF: Mesangial deposits of IgA
and C3
·
Prognosis: only 15 – 20% progress
to end-stage renal failure – these are more likely to have proteinuria,
hypertension and impaired renal function at presentation
· No effective treatment. Consider immunosuppressive treatment if rapidly progressive
·
Similar to Henoch-Scholein
Purpura – but HSP is more widespread, causing purpura (especially buttocks and
ankles) and abdominal pain (which may ® GI bleeding)
Mesangiocapillary (Membranoproliferative) GN*
·
50% present as Nephrotic Syndrome
·
Biopsy:
o LM: cellular expansion of the mesangium.
„Twin track‟ BM
o EM: Subendothelial deposits or
deposits within the BM
Rapidly Progressive Glomerulonephritis
·
What is it:
o A description not a diagnosis
o = Acute renal failure secondary to glomerula disease generally with a nephritic presentation.
o Any form of GN can present in a rapidly progressive form. Generally
caused by immune mediated diseases
·
~ Crescentic glomerulonephritis
(marker for severe RPGN)
o = Cellular proliferation in glomeruli, and crescent formation.
o Pathogenesis of crescents: rupture of the basement membrane ® fibrin leaks into Bowman‟s space, macrophages recruited, epithelioid cells form a crescent. Leads to scarring and fibrosis of glomeruli
·
Presentation:
o Nephritic presentation. Nephrotic
range proteinuria is rare
o ® ¯GFR but
tubular function OK so Na/H20 reabsorbed ® oedema
o Systemic features of immune mediated diseases: myalgia, arthralgia,
fever, etc
·
Investigations:
o Urine chemistry midway between pre-renal ARF and ATN
o Light Microscope: Extensive proliferation of cells, numerous crescents,
generally without polymorphs
o Immunoflouresence:
§ Granular IgG and C3 Þ immune complex mediated (Post strep, Lupus, etc)
§ Linear IgG Þ Goodpastures
§ None Þ pauci-immune
·
Due to:
o Immune complex mediated GN:
§ Post-infectious GN: e.g. post-streptococcal (rarely crescents, dialysis
rarely needed) also staph. Has granular IgG plus neutrophils
§ Lupus Nephritis, Has
granular IgG (plus IgA, IgE, etc)
§ Others, including vasculitis
o Anti-glomerular-basement membrane diseases (Goodpasture‟s syndrome)
o Pauci-immune: (ie no evidence of immune deposits, probably cell mediated immune problem):
§ Wegener‟s Granulomatosis: Causes GN, URTI, LRTI, non-caseating granuloma, cANCA is highly specific, -ive immunoflourescence, typically older patients.
§ Microscopic polyarteritis (also joints)
·
Prognosis dependent on % of
crescents
·
Treatment: immunosuppressive (iv
methylprednisolone, cyclophosphamide) +/- dialysis
Related Topics