Chapter: Medicine Study Notes : Renal and Genitourinary
Male Genitourinary
Male Genitourinary
Prostate
Anatomy
·
Normally 20 – 30 g. Grossly enlarged can be 500g
·
Prostate can become infected,
hyperplastic or malignant
·
Used to be described in
lobes. Now described in zones:
o Anterior zone
o Transition and central zone: main site of benign hyperplasia
o Peripheral zone: main site of malignancy. Next to rectum – can palpate on PR
· PR exam:
o Even if normal, don‟t ignore PSA. Cancers can be small or diffuse, or anterior, in an already large prostate ® PR isn‟t sensitive
o Nodularity can be detected on PR. This is due to desmoplasia (fibrous
reaction) – usually to a slower infiltrating
cancer
Prostatitis
·
Acute:
o Gonorrhoea most common cause: pain, discharge, haematuria, tender on PR
o May be infarction secondary to hyperplasia compressing blood supply
·
Granulomatous:
o Tb (rare)
o Fungal (only immunocompromised)
o Leakage of prostatic secretion into interstitium post surgery
o Resolving prostates (hard, knobbly prostate, PSA,
mistaken for malignancy). Suspect post surgery, but still need biopsy
Benign Prostatic Nodular Hyperplasia
·
Not benign if not treated: ®
hydronephros ® kidney failure ® death!
· Common: 75% of all men over 75 years of age
· Testosterone ¯ with age ® oestrogen ® potentiates effect of Dihydrotestosterone (DHT) on the prostate ® prostatic hyperplasia
·
Morphology: nodular proliferation
of ducts, mainly in the central zone
·
Histology: epithelial nodules,
fibrosis, chronic inflammation, focal infarction
·
Management:
o Transurethral prostatic resection (TURP): always ®
retrograde ejaculation + risk of impotence and incontinence
· 5 a Reductase Inhibitors (blocks Testosterone ® DHT). Usually preferred. OK if not acute obstruction
Prostatic Carcinoma
·
Occurs in 25% of males over 70
years. (More if include indolent central
or transition zone tumours)
·
6% mortality in males
· Predominantly adenocarcinoma occurring in the peripheral zone
·
Key histological features: single
cell basal layer in duct epithelium, prominent nucleolus, lots of small glands
·
Prognosis related to Grade (using
Gleason score: 2 is good, 10 is very bad)
·
Spreads to pelvic lymph nodes via
perineural infiltration
· Prostate Specific Antigen:
o PSA – a tumour marker. Screening test only. Serum PSA correlates with tumour burden. PSA is a lytic agent that makes seminal fluid runny. If > 4 then do free to bound ratio, and/or follow/refer patient
o In benign
and malignant tumours, or
inflammation
·
Management:
o Transurethral resection
o Radiotherapy
o Radical prostatectomy (selected on basis of tumour bulk and grade (not
if very high grade – will already have metastasised). 50% have complications
(impotence, incontinence)
Workup of Obstruction from Enlarged Prostate
·
Investigations:
o Cr: checking renal function
o K and Na: checking renal failure
o Blood gases for metabolic acidosis
o PSA
o Ultrasound: look for distended bladder and hydronephrosis
o ECG if K: if ECG changes or if K high then may need anti-arrhythmic
·
Management:
o Catheterise: should see K and Cr resolve over a day (depending on
remaining renal function)
o If high K, then insulin + glucose
· Complications of obstruction:
o Enlarged bladder: hyperplasia of detrussor muscle fibres, space
between trabeculated fibres
o Back
pressure in ureter ® hydronephrosis
§ ¯Filtration
® Cr
§ ¯Function
of tubular epithelium due to poor perfusion ® ¯active transport of K
§ Acidosis
·
Moral: Must act on a distended
bladder to protect the kidney
Prostate Cancer Screening*
·
Notes prepared for Public Health
Test. Does PSA meet the 6 criteria for a good screening test? Source: Readings
on Closed Reserve
·
Is it an important health issue:
o 2nd leading cause of cancer death in men in the US. In NZ, 800 cases and 400 deaths per year
o A disease of the very old. 1% < 55 years, 65% > 75 years. Would
reducing incidence lead to decline in all-causes mortality?
·
Is there a suitable test: PSA
test + digital rectal exam. PSA test is reasonably good at detecting pathology,
and sensitivity is improving (currently ~ 80%)
·
Is the natural history well
understood:
o Wide variety of cancers: from the slow growing, indolent sort to very
aggressive
o Need long enough asymptomatic duration to allow screening at reasonable
intervals
o Screening likely to detect indolent cancers (length bias)
o Incidence of prostate cancer has increased dramatically since
opportunistic screening introduced ® treating many cancers that would
have remained harmless (ie would die WITH cancer but not BECAUSE of cancer)
·
Does treatment at the
asymptomatic stage confer positive benefits over later treatment:
o No firm evidence that radical prostatectomy is better than conservative
treatment for asymptomatic cancers
o For Grade I and II cancers, evidence that conservative treatment is at
least reasonably effective
o Risks of prostatectomy: 30-day mortality of 0.5% + significant levels of
ongoing incontinence and sexual dysfunction
o Assuming 4% rate of detection from screening, 1 in 5000 will die, 1 in
81 will be incontinent, and 1 in 36 will have sexual dysfunction as the result
of the screening
o Conclusion: Screening is good at detection pathology, but don‟t yet know
if treatment is beneficial in net terms
·
Infrastructure and cost: of
lesser relevance until it can be demonstrated that screening is clinically
effective
Penis
· For congential malformations and paediatric presentations
·
Epispadias: abnormal opening of
urethra on ventral surface
·
Fractured Penis: Rupture of
corpus cavernosum during erection
· Condyloma: Genital wart. Usually flat. Associated with HPV.
· Erythroplasia of Queyrat (= Bowen‟s disease): non-invasive cancer of the penis. Premalignant condition. Usually starts in coronal sulcus.
·
Squamous cell carcinoma: Very
rare, risk if not circumcised. Early spread to lymph nodes but doesn‟t
disseminate widely
Scrotum
·
Steatocystoma: benign sebaceous
cysts, hereditary
·
Fournier‟s gangrene: Ischaemic
necrosis. Little collateral flow to the
scrotum so occlusion ® domino
·
effect. Treatment: debridement
·
Squamous cell carcinoma
Testes
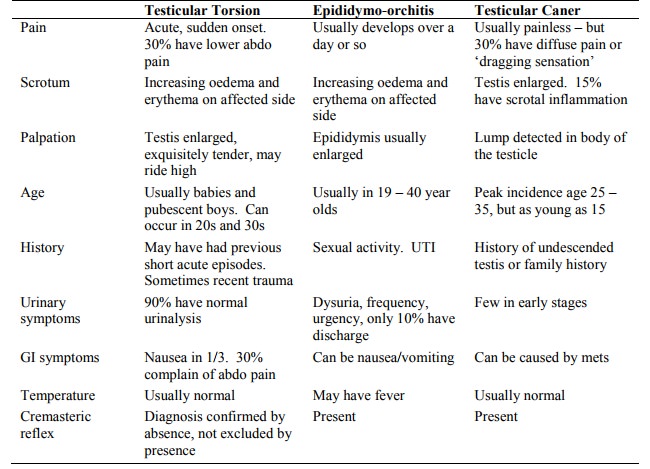
· For Torsion and Hydrocoele, see Testes (Topic)
Infection
·
Epididymo-orchitis:
o Bacterial infection: E Coli, Klebsiella, Proteus
o In adults also Gonorrhoea
o Usually self-limiting ® antibiotics
o Key differential: torsion. If in
doubt, emergency referral and Doppler US to assess blood flow
·
Primary Orchitis:
o Mumps, Tb, tertiary syphilis
o Rare
Other
·
Spermatocoele: dilation of a
chord of epididymis: common benign small lump on testis. Translucent to torch
·
Haematocoele: Haemorrhage into
tunica vaginalis or tunica albicinia (rugby injury, bleeding disorder)
Testicular Tumours
·
Incidence 3.5/100,000
·
3% bilateral
·
7% associated with undescended
testis
·
Germ cell tumours:
o 95% of testicular tumours
o Derived from germ cells
o Peak in 15 – 34 year olds
o Painless swelling of the testis
o Seminoma:
§ 40% of testicular tumours
§ Gross: lobulated pale tumour mass
§ Micro: Undifferentiated germ cells + lymphocytes. Aggressive. Metastasise to inguinal and para-aortic nodes
§ Treatment: Orchidectomy via inguinal region (never via scrotum ®
different lymphatic drainage. Also never biopsy suspected testicular cancers).
Very responsive to radiotherapy
o Teratoma:
§ 30% of testicular tumours
§ All can recapitulate ectodermal, mesodermal and endodermal tissue
§ Benign teratoma: More common in ovary than testis. 3% chance of
malignant change. Mature tissues (usually skin elements – epidermis, hair
follicles, etc)
§ Malignant teratoma: metastasise to para-aortic lymph nodes (especially
neural cells – very
§ aggressive). Gross appearance – lots of variety. Treatment: chemo +/-
radiotherapy. Chemo stimulates cells to mature ® still
malignant but slower growing ® excision of affected lymph nodes
o Embryonal carcinoma: poorly differentiated, resembles adenocarcinoma. Highly malignant. May express tumour marker alpha-fetoprotein
o Choriocarcinoma: Placental tissues (resembles hydatiform mole). Expresses bHCG ® positive for pregnancy test.
Contains highly malignant syncytiotrophoblast and cytotrophoblast cells.
Responds well to chemotherapy
o Mixed tumours: Teratoma and seminoma
·
Sex chord/stromal tumours:
o Leydig tumours: 90% benign. Small brown mass. Present with overproduction of testosterone: precocious puberty or gynaecomastia in post-puberty. Can produce androgens, oestrogen or corticosteroids
o Sertoli cell tumours: Rare. 90% benign. Within seminephrous tubules of the testis. Local infiltration
·
Lymphoma: Older males, often bilateral,
poorly differentiated and poor prognosis
·
Testicular tumours present
relatively young, lymphoma in older men
Differential of Testicular Swelling
Related Topics