Chapter: Medicine Study Notes : Renal and Genitourinary
Chronic Renal Failure
Chronic Renal Failure
·
= Reduction in renal function for
> 6 months
·
Causes in NZ in 1997:
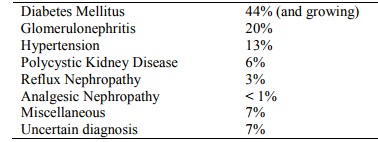
§ Miscellaneous causes include: stone disease, interstitial nephritis,
amyloidosis, myeloma, lithium toxicity, obstructive uropathy, renal cell
carcinoma, post-partum failure
·
Symptoms:
o Earlier: nausea, anorexia, lethargy, itch, nocturia, impotence
o Later: oedema, SOB, chest pain (from pericarditis), vomiting, confusion,
fits
·
See also:
o Wegner‟s granulomatosis, Microscopic Polyarteritis, and Henoch-Schonlein Purpura, Vasculitis
Diabetic Nephropathy
·
Epidemiology: Nephropathy in
o 30 – 50% of type 1 diabetic patients (after ~ 10 – 15 years of disease)
o 20 – 30% of type 2 diabetic patients – many with overt disease at the time of presentation
o In both cases is associated with poor glycaemic control, hypertension
and proteinuria
·
Definitions:
o Overt diabetic nephropathy = proteinuria > 500 mg/day in the absence
of other renal disease
o Microalbuminuria:
§ Albumin excretion 30 – 300 mg/day (= 20 – 200 mg/minute). Concentration is not relevant – it is the amount excreted per unit time. Albumin is more specific for nephropathy than total urine protein (normal protein < 150 mg/day – mainly from tubular cells). Normal dipsticks not sensitive enough at this level. Random early morning urine is dependent on concentration. Urinary albumin:creatinine ratio is a useful screening test
§ Marker for endothelial damage elsewhere.
Strong association with retinopathy, IHD, etc
§ Prognosis for a diabetic with microalbuminaemia is worse than for HIV!
·
Natural History:
o Type 1 Diabetes:
§ Not usually evident until after 10 – 15 years of disease. If none by 25
years then nephropathy unlikely
§ Once overt nephropathy starts, progresses to ESRF over 5 – 7 years
§ Initial hyperfiltration in about 50% of diabetics (GFR by
about 25 – 50%). Overtime this reduces and hypertension ensues
o Type 2 Diabetes: Similar progression to ESRF once overt nephropathy
·
Pathology:
o Intra-glomerular pressure, glomerular hypertrophy, ?deposition of advanced glycosylation end products
o Glomeruli:
§ Glomerulosclerosis: nodular (Kimmelstiel-Wilson) or diffuse
§ Mesangial broadening with deposition of eosinophilic material
§ GBM irregularly thickened
o Arterioles show evidence of subintimal arteriosclerosis and
hyalinisation
o Interstitial changes: tubular atrophy and fibrosis
·
Look for other renal pathology
if:
o No retinopathy
o Active urinary sediment
o Rapid onset nephrotic syndrome
o Type 2 diabetes
·
Management:
o Glycaemic control. HBA1c < 8.5% delays progression in early phases – not later
o Anti-hypertensive treatment: All effective. ACE inhibitors are best at ¯ protein and ¯intra-glomerular pressure. May delay progression even in normotensive patients. Aim to lower blood pressure by as much as possible without creating hypotensive symptoms. Also calcium antagonists (diltiazem and Verapamil ® ¯proteinuria)
o Protein Restriction: Limiting intake may reduce progression. High intake ® intraglomerular pressure and hyperfiltration
o Dialysis: worse prognosis than non-diabetics due to concurrent IHD. Peritoneal dialysis better if CVS instability
o Transplant: best prognosis in the absence of CV disease. Disease can
recur in the graft 5 – 10 years later
·
Other renal complications:
o Urinary tract sepsis. Should be treated even if asymptomatic
o Risk of
pyelonephritis
o Papillary necrosis. May ®
macroscopic haematuria or ureteric obstruction
o Autonomic neuropathy ® neurogenic bladder ® infection/obstruction
o Contrast nephropathy: always hydrate aggressively
Systemic Lupus Erythematosus
·
Renal involvement common:
o Clinically apparent in around 50%
o Histologic lupus nephritis in 100%
o 5% present with a renal syndrome
·
Presentation:
o Usually heavy proteinuria, nephritic syndrome or RPGN
o Test for SLE antibodies(see Blood tests in Inflammatory Arthritis)
o Most patients have ¯complement
·
Histology:
o Mimics anything!
o Most severe: Diffuse proliferative glomerulonephritis with crescents
o Common: membranous pattern, tubulo-interstitial damage
o Immunoflouresence (IF): extensive deposition of IgG and C3, also C1q, IgA, IgM and fibrin
Reflux Nephropathy
· Most common cause of end-stage renal failure in children, secondary to vesico-ureteric reflux + infection in infancy
·
May not appear till adulthood (ie
slowly progressive)
·
Investigations:
o Renal cortical scarring on ultrasound or DMSA scan
o IVU may show clubbing of calyces
o Biopsy: chronic interstitial disease with secondary focal
glomerulosclerosis
·
Treatment: aggressive blood
pressure control
Thrombotic Microangiopathy
·
Includes Haemolytic Uraemic
Syndrome (HUS), Thrombotic Thrombocytopaenic Purpura (TTP) and HELLP Syndrome
of Pregnancy (Haemolysis, elevated liver enzymes and low platelets)
·
Presentation:
o Microangiopathic haemolytic anaemia, low platelets and renal and
neurological manifestations
o Renal involvement: haematuria and proteinuria, renal failure in 40 – 80%
·
Investigations: Blood film ® marked
fragmentation of red cells, Comb‟s test –ive
·
Treatment: 90% response to
plasmapheresis with or without corticosteroids
Amyloidosis
·
A dysproteinaemia that usually
presents renally with nephrotic syndrome
· Types:
o Primary amyloidosis: idiopathic or associated with myeloma. Amyloid protein is part of the Ig light chain. Poor prognosis
o Secondary amyloidosis: deposition of a different form of protein.
Associated with chronic inflammatory or infective conditions (eg Rheumatoid
arthritis, Tb, etc)
·
Particularly affects glomerular
capillary walls, seen with Congo Red Stain
Related Topics