Chapter: Medicine Study Notes : Renal and Genitourinary
Assessment of Renal Function
Assessment of Renal Function
Urinalysis
·
Dipstick:
o Blood: indicates bleeding in the urinary tract or free haemoglobin or myoglobin
o Proteinuria: sensitive to protein – but use 24 hour urine to quantify, or spot check with protein:Cr ratio in morning urine. Urine protein is normally albumin. Hyaline and granular casts and Bense Jones Proteins don’t test +ive for protein
o Glucose: diabetes, pregnancy, sepsis, tubular damage or low renal threshold
o Nitrates Þ UTI
·
Microscopy:
o Blood: should be less than 8 * 10E6 cells per litre
§ Normal morphology suggests bleeding from the lower urinary tract: calculi, infection, neoplasia
§ Dysmorphic cells suggests glomerular bleeding: glomerulonephritis and
vasculitis (including endocarditis). Microhaematuria can be either nephrotic or
nephritic. Macro haematuria is normally nephritic
o WBCs indicate infection, less commonly renal tuberculosis, renal stones and papillary necrosis
o Eosinophils Þ interstitial nephritis
o Casts:
· Hyaline casts: just protein, no cellular elements and may be normal (especially concentrated urine)
·
Granular casts: Degenerative
cellular material – usually tubular cells Þ pathology
·
Red cell casts: glomerular
bleeding ® usually active GN
·
White cell casts: pyelonephritis,
interstitial nephritis or glomerulonephritis
Glomerular Filtration Rate (GFR)
· Marker of renal excretory function
· Determined by intra-glomerular pressure, which in turn is determined by the difference in vascular tone between afferent and efferent arterioles. Maintained by autoregulation except when blood pressure is very high or very low
· Creatinine:
o Filtered at the glomerulus and not reabsorbed, but a small amount is excreted from the tubules (ie GRF less reliable at small urine flows)
o Affected by muscle mass, protein intake and age ® poor indicator of renal function. Serial measurements helpful
o Normal Creatinine < 0.110 mmol/L
·
Use Cockcroft-Gault formula:
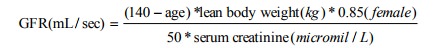
o Normal is > 1.5 ml/sec (> 90 ml/min)
o Use total body weight but recognise it overestimates if obese
·
Or collect 24 hour urine and
compare to plasma concentration with UV/P
·
Can measure with radionucliotides
Other
·
Do volume assessment: lying and
standing BP, JVP, change in weight, etc
·
Tubular Function: test
concentrating ability with fluid deprivation and ADH administration
·
Urinary Acidification: give
ammonium chloride and then measure urinary pH
·
Also consider blood tests: Ca,
PO4, FBC, complement, autoantibodies, etc
Renal Imaging
·
Plain X-ray: shows radio-opaque
renal stones (90% are) not uric acid stones (eg Gout). Methodology:
o Gas:
§ Renal colic/pancreatitis ® focal ileus
§ Emphysematous pyelonephritis ® gas in kidney
§ Emphysematous cystitis ® gas in bladder
o Stripes:
§ Find the psoas muscle and move out parallel to this to find the kidneys
§ Assess size: length of kidney = length of 3 vertebrae + disc spaces. Up to 2 cm variation in size between kidney‟s OK
o Stones: check down ureters: down psoas, anterior to sacro-iliac
junction, around pelvis, into bladder
o Bones: renal osteodystrophy, etc
·
Intravenous Urogram (Plain film +
contrast) = IVU = IVP (Intravenous pyleogram)
o Gives anatomical and functional information
o Shows renal contours, presence of scarring, reflux nephropathy,
obstruction
o Depends on renal uptake of the contrast.
Little use if significant renal impairment (eg CR > 200)
o Interpretation:
§ Nephrogram phase (1 minute post injection): renal contour, position,
equal in intensity?
§ Pyelogram phase (5 minutes): see major and minor calicies and bladder
§ Post micturition phase: look for normal voiding
· Antegrade and retrograde pyelography: direct injection of contrast into the renal pelvis or the ureter
·
Micturating Cystourethrogram:
Fill bladder with contrast and image following micturition. For assessment of
vesico-ureteric reflux in children
·
Ultrasound:
o For renal size and contour
o Shows hydronephrosis – but may not show the site of obstruction. Reasonable view of renal masses and cysts
o Scarring: asymmetric indentation of renal outline. If young ® ?reflux. If older ® ?ischaemia
·
CT: for complex cysts, masses,
renal colic and stones.
o Modality of choice for stones. 5 mm slices:
§ Sensitivity
§ No contrast risk (mortality 1 in 40,000)
§ Can sort out differentials of colic (eg appendicitis) on CT that you won‟t see on IVP
o Stone filling the whole of the renal calicies = staghorn calyx (in
recurrent infection and alkaline urine)
· Nuclear medicine studies:
o Renogram for assessing function of each kidney, avoids nephrotoxic
contrasts. Eg Technetium labelled DTPA and Mag3. Especially good for renal
artery stenosis and obstruction
o DMSA: highlights proximal tubules.
Good for showing renal scarring, eg reflux nephropathy
·
Arteriography: Renal artery stenosis
Renal Biopsy
·
Under local
·
Indications: acute renal failure,
nephrotic syndrome, heavy proteinuria or haematuria
·
Only if histology will influence
management
· Major contraindication: bleeding tendency (check FBC and clotting first)
·
Complications: bleeding and
development of a perirenal haematoma (eg in amyloid disease when rigid
arterioles won‟t contract following bleeding)
·
Risk of serious complications
< 1% (fistula, haematoma, infection, surgery, etc)
Related Topics