Chapter: Medical Surgical Nursing: Oncology: Nursing Management in Cancer Care
Surgery - Management of Cancer
SURGERY
Surgical removal of the
entire cancer remains the ideal and most frequently used treatment method. The
specific surgical ap-proach, however, may vary for several reasons. Diagnostic
surgery is the definitive method of identifying the cellular characteristics
that influence all treatment decisions. Surgery may be the primary method of
treatment, or it may be prophylactic, palliative, or reconstructive.
Diagnostic Surgery
Diagnostic surgery, such as a biopsy,
is usually performed to ob-tain a tissue sample for analysis of cells suspected
to be malignant. In most instances, the biopsy is taken from the actual tumor.
The three most common biopsy methods are the excisional, inci-sional, and
needle methods.
Excisional biopsy is most frequently used for easily accessible tumors
of the skin, breast, upper and lower gastrointestinal tract, and upper
respiratory tract. In many cases, the surgeon can re-move the entire tumor and
surrounding marginal tissues as well. This removal of normal tissue beyond the
tumor area decreases the possibility that residual microscopic disease cells
may lead to a recurrence of the tumor. This approach not only provides the
pathologist who stages and grades the cells with the entire tissue specimen but
also decreases the chance of seeding the tumor (dis-seminating cancer cells
through surrounding tissues).
Incisional biopsy is
performed if the tumor mass is too large to be removed. In this case, a wedge
of tissue from the tumor is removed for analysis. The cells of the tissue wedge
must be rep-resentative of the tumor mass so that the pathologist can provide
an accurate diagnosis. If the specimen does not contain represen-tative tissue
and cells, negative biopsy results do not guarantee the absence of cancer.
Excisional and
incisional approaches are often performed through endoscopy. Surgical incision,
however, may be required to determine the anatomic extent or stage of the
tumor. For ex-ample, a diagnostic or staging laparotomy, the surgical opening
of the abdomen to assess malignant abdominal disease, may be necessary to
assess malignancies such as gastric cancer.
Needle biopsies are performed to sample suspicious masses that are
easily accessible, such as some growths in the breasts, thy-roid, lung, liver,
and kidney. Needle biopsies are fast, relatively inexpensive, and easy to
perform and usually require only local anesthesia. In general, the patient
experiences slight and tempo-rary physical discomfort. In addition, the
surrounding tissues are disturbed only minimally, thus decreasing the likelihood
of seed-ing cancer cells. Needle aspiration biopsy involves aspirating tis-sue
fragments through a needle guided into an area suspected of bearing disease.
Occasionally, radiologic imaging or magnetic res-onance imaging is used to help
locate the suspected area and guide the placement of the needle. In some
instances, the aspira-tion biopsy does not yield enough tissue to permit
accurate diag-nosis. A needle core biopsy uses a specially designed needle to
obtain a small core of tissue. Most often, this specimen is suffi-cient to
permit accurate diagnosis.
In some situations, it is necessary to biopsy lymph nodes that are near
the suspicious tumor. It is well known that many cancers can spread
(metastasize) from the primary site to other areas of the body through the
lymphatic circulation. Knowing whether adjacent lymph nodes contain tumor cells
helps physicians plan for systemic therapies instead of, or in addition to,
surgery in order to combat tumor cells that have gone beyond the primary tumor
site. The use of injectable dyes and nuclear medicine imag-ing can assist the
surgeon in identifying lymph nodes (sentinel nodes) that process lymphatic
drainage for the involved area. This procedure is used in patients with
melanoma and is being used with increasing frequency in patients with cancers
of the breast, colon, and vulva, although it is still considered
investigational.
The choice of biopsy
method is based on many factors. Of greatest importance is the type of
treatment anticipated if the cancer diagnosis is confirmed. Definitive surgical
approaches in-clude the original biopsy site so that any cells disseminated during the biopsy are excised at the time of surgery. Nutrition and
hematologic, respiratory, renal, and hepatic function are consid-ered in
determining the method of treatment as well. If the biopsy requires general
anesthesia and if subsequent surgery is likely, the effects of prolonged
anesthesia on the patient are considered.
The patient and family are given an opportunity to discuss the options
before definitive plans are made. The nurse, as the patient’s advocate, serves
as a liaison between the patient and the physician to facilitate this process.
Time should be set aside to minimize interruptions. Time should be provided for
the patient to ask ques-tions and for thinking through all that has been
discussed.
Surgery as Primary Treatment
When surgery is the primary approach in treating cancer, the goal is to
remove the entire tumor or as much as is feasible (a proce-dure sometimes
called debulking) and any involved surrounding tissue, including regional lymph
nodes.
Two common surgical approaches used for treating primary tumors are
local and wide excisions. Local excision is warranted when the mass is small.
It includes removal of the mass and a small margin of normal tissue that is
easily accessible. Wide or radical excisions (en bloc dissections) include
removal of the primary tumor, lymph nodes, adjacent involved structures, and
surround-ing tissues that may be at high risk for tumor spread. This surgi-cal
method can result in disfigurement and altered functioning. Wide excisions are
considered, however, if the tumor can be re-moved completely and the chances of
cure or control are good.
In some situations,
video-assisted endoscopic surgery is replac-ing surgeries associated with long
incisions and extended recovery periods. In these procedures, an endoscope with
intense lighting and an attached multichip minicamera is inserted through a
small incision into the body. The surgical instruments are inserted into the
surgical field through one or two additional small incisions, each about 3 cm
long. The camera transmits the image of the involved area to a monitor so the
surgeon can manipulate the instruments to perform the necessary procedure. This
type of procedure is now being used for many thoracic and abdominal surgeries.
Salvage surgery is an
additional treatment option that uses an extensive surgical approach to treat
the local recurrence of the cancer after a less extensive primary approach is
used. A mastec-tomy to treat recurrent breast cancer after primary lumpectomy
and radiation is an example of salvage surgery.
In addition to the use of surgical blades or scalpels to excise the mass
and surrounding tissues, several other types of surgical interventions are
available. Electrosurgery makes use of electrical current to destroy the tumor
cells. Cryosurgery uses liquid nitro-gen to freeze tissue to cause cell
destruction. Chemosurgery uses combined topical chemotherapy and layer-by-layer
surgical re-moval of abnormal tissue. Laser surgery (l ight amplification by stimulated emission of radiation)
makes use of light and energyaimed at an exact tissue location and depth to
vaporize cancer cells. Stereotactic radiosurgery (SRS) is a single and highly
pre-cise administration of high-dose radiation therapy used in some types of
brain and head and neck cancers. This type of radiation has such a dramatic
effect on the target area that the changes are considered to be comparable to
more traditional surgical ap-proaches (International Radiosurgery Support
Association, 2000).
A multidisciplinary approach to patient care is essential during and
after any type of surgery. The effects of surgery on the patient’s body image,
self-esteem, and functional abilities are addressed. Ifnecessary, a plan for
postoperative rehabilitation is made before the surgery is performed.
The growth and
dissemination of cancer cells may have pro-duced distant micrometastases by the
time the patient seeks treat-ment. Therefore, attempting to remove wide margins
of tissue in the hope of “getting all the cancer cells” may not be feasible.
This reality substantiates the need for a coordinated multidisciplinary
approach to cancer therapy. Once the surgery has been com-pleted, one or more
additional (or adjuvant) modalities may be chosen to increase the likelihood of
destroying the cancer cells. However, some cancers that are treated surgically
in the very early stages are considered to be curable (eg, skin cancers,
testicular cancers).
Prophylactic Surgery
Prophylactic surgery involves removing nonvital tissues or organs that
are likely to develop cancer. The following factors are con-sidered when
electing prophylactic surgery:
· Family history and
genetic predisposition
· Presence or absence of
symptoms
· Potential risks and
benefits
· Ability to detect cancer
at an early stage
· Patient’s acceptance of
the postoperative outcome
Colectomy, mastectomy, and oophorectomy are examples of prophylactic
operations. Recent developments in the ability to identify genetic markers
indicative of a predisposition to develop some types of cancer may play a role
in decisions concerning pro-phylactic surgeries. Some controversy, however,
exists about adequate justification for prophylactic surgical procedures. For
example, a strong family history of breast cancer, positive BRCA-1 or BRCA-2
findings, an abnormal physical finding on breast examination such as
progressive nodularity and cystic disease, a proven history of breast cancer in
the opposite breast, abnormal mammography findings, and abnormal biopsy results
may be fac-tors considered in making the decision to proceed with a
prophy-lactic mastectomy (Houshmand, Campbell, Briggs, McFadden &
Al-Tweigeri, 2000; Zimmerman, 2002).
Because the long-term
physiologic and psychological effects are unknown, prophylactic surgery is
offered selectively to patients and discussed thoroughly with the patient and
family. Preopera-tive teaching and counseling, as well as long-term follow-up,
are provided.
Palliative Surgery
When cure is not possible, the goals of treatment are to make the
patient as comfortable as possible and to promote a satisfying and productive
life for as long as possible. Whether the period is ex-tremely brief or
lengthy, the major goal is a high quality of life— with quality defined by the
patient and family. Honest and informative communication with the patient and
family about the goal of surgery is essential to avoid false hope and
disappointment.
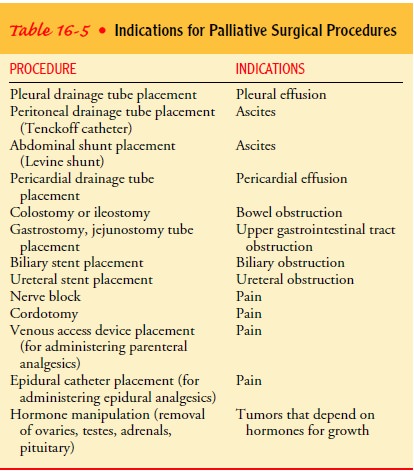
Palliative surgery is
performed in an attempt to relieve com-plications of cancer, such as
ulcerations, obstructions, hemor-rhage, pain, and malignant effusions (Table
16-5).
Reconstructive Surgery
Reconstructive surgery may follow curative or radical surgery and is carried out in an attempt to improve function or obtain a more desirable cosmetic effect. It may be performed in one operation or in stages. Patients are instructed about possible reconstructive surgical options before the primary surgery by the surgeon who will perform the reconstruction. Reconstructive surgery may be indicated for breast, head and neck, and skin cancers.
The nurse must recognize
the patient’s needs and the impact that altered functioning and altered body
image may have on quality of life. Providing the patient and family with
opportuni-ties to discuss these issues is imperative. The needs of the
indi-vidual must be accurately assessed and validated in each situation for any
type of reconstructive surgery.
Nursing Management in Cancer Surgery
The patient undergoing surgery for cancer requires general
peri-operative nursing care, as described in Unit 4, along with specific care
related to the patient’s age, organ impairment, nutritional deficits, disorders
of coagulation, and altered immunity that may increase the risk for
postoperative complications. Combining other treatment methods, such as
radiation and chemotherapy, with surgery also contributes to postoperative
complications, such as infection, impaired wound healing, altered pulmonary or renal
function, and the development of deep vein thrombosis. In these situations, the
nurse completes a thorough preoperative as-sessment for all factors that may
affect patients undergoing sur-gical procedures.
The patient undergoing
surgery for the diagnosis or treatment of cancer is often anxious about the
surgical procedure, possible findings, postoperative limitations, changes in
normal body func-tions, and prognosis. The patient and family require time and
as-sistance to deal with the possible changes and outcomes resulting from the
surgery.
The nurse provides education and emotional support by as-sessing patient
and family needs and exploring with the patient and family their fears and
coping mechanisms, encouraging them to take an active role in decision making
when possible. When the patient or family asks about the results of diagnostic
testingand surgical procedures, the nurse’s response is guided by the
in-formation the physician previously conveyed to them. The pa-tient and family
may also ask the nurse to explain and clarify information that the physician
initially provided but that they did not grasp because they were anxious at the
time. It is important for the nurse to communicate frequently with the
physician and other health care team members to be certain that the
informa-tion provided is consistent.
After surgery, the nurse assesses the patient’s responses to the surgery
and monitors for possible complications, such as infection, bleeding,
thrombophlebitis, wound dehiscence, fluid and elec-trolyte imbalance, and organ
dysfunction. The nurse also provides for patient comfort. Postoperative
teaching addresses wound care, activity, nutrition, and medication information.
Plans for discharge,
follow-up and home care, and treatment are initiated as early as possible to
ensure continuity of care from hospital to home or from a cancer referral
center to the patient’s local hospital and health care provider. Patients and
families are also encouraged to use community resources such as the Amer-ican Cancer
Society or Make Today Count for support and information.
Related Topics