Chapter: Medical Surgical Nursing: Oncology: Nursing Management in Cancer Care
Cancer Rehabilitation
Cancer Rehabilitation
Many cancer patients, including those who receive primary sur-gical
treatment and adjuvant chemotherapy or radiation therapy, return to work and
their usual activities of daily living. These patients may encounter a variety
of problems, including changes in their functional abilities and in the
attitudes of employers, coworkers, and family members who still view cancer as
a termi-nal, debilitating disease. Nurses play an important role in the
rehabilitation of the cancer patient. Both the patient and family are included
as part of any rehabilitation effort because cancer affects not only the
patient but also the family members. In addition, with the shift away from
inpatient care, many families are caring for patients at home. To maximize
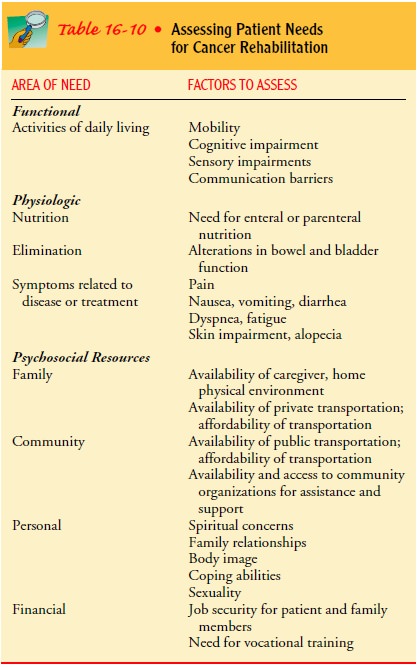
beneficial outcomes, evalua-tion of the patient’s needs related to cancer
rehabilitation begins early in cancer treatment (Table 16-10).
Assessment for body image changes as a result of disfiguring treatments
is necessary to facilitate the patient’s adjustment to changes in appearance or
functional abilities. The nurse can refer the patient and family to a variety
of support groups sponsored by the American Cancer Society, such as those for
people who have had laryngectomies or mastectomies. Nurses also collaborate
with physical, occupational, and enterostomal therapists in im-proving the
patient’s abilities in the use of prosthetic and assistive devices, and in
altering the home environment as needed.
Patients often experience distress (eg, pain, nausea) related to the underlying cancer or treatments. These symptoms may in-terfere with work and quality of life. Nurses assess for these prob-lems and assist the patient in identifying strategies for coping with them. For patients with gastrointestinal disturbances after chemotherapy, altering work hours or receiving treatments in the evenings may prove helpful. Collaboration with physicians and pharmacists is helpful in identifying appropriate interventions.
Nurses collaborate with dietitians to help patients plan meals that will
be acceptable and meet nutritional requirements. Nurses are also involved in
the ongoing assessment of patients to detect any long-term consequences of
cancer treatment.
Although the Americans With Disabilities Act of 1990 was in-tended to
protect patients with disabling disorders against dis-crimination, recovering
cancer patients have reported instances of unfair practices and discrimination
in the workplace. Some employers do not understand that different kinds of cancers
have different prognoses and different effects on functional ability. As a
result, employers may hesitate to hire or continue to employ people with
cancer, especially if ongoing treatment regimens re-quire adjustments in work
schedules. Employers, coworkers, and families may continue to view the person
as “sick” despite on-going recovery or completion of treatment. Attitudes of
coworkers can be a problem when the patient has a communication impair-ment, as
may occur in some head and neck cancers. The patient may benefit from
vocational rehabilitation services of the Amer-ican Cancer Society or other
agencies.
Nurses can participate in efforts to educate employers and the public in
general to ensure that the rights of patients with cancer are maintained.
Whenever possible, nurses assist patients and families to resume preexisting
roles. Psychologists and clergy or spiritual advisors are consulted to assist
with psychosocial and spiritual concerns. Rehabilitation shifts the focus from
what has been lost to what can be done with existing strengths and abili-ties.
In that spirit, nurses encourage patients to regain the high-est level of
function and independence possible.
Gerontologic Considerations
As a result of an increased life expectancy and an increased risk for
cancer with age, nurses are providing cancer-related care for growing numbers
of elderly patients. More than 58% of all can-cers occur in people older than
65 years of age, and about two thirds of all cancer deaths occur in people 65
years of age and older. Nursing care of this population addresses special
needs, in-cluding physical, psychosocial, and financial concerns.
Oncology nurses working with the elderly population need to understand
the normal physiologic changes that occur with aging. These changes include
decreased skin elasticity; decreased skeletal mass, structure, and strength;
decreased organ function and structure; impaired immune system mechanisms;
alterations in neurologic and sensory functions; and altered drug absorption,
distribution, metabolism, and elimination. These changes ulti-mately influence
the elderly patient’s ability to tolerate cancer treatment. In addition, many
elderly patients have other chronic diseases and associated treatments that may
limit tolerance to cancer treatments (Table 16-11).
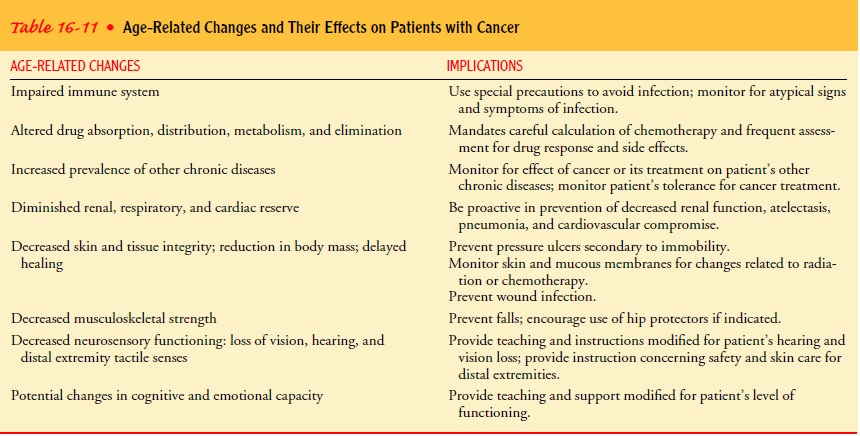
Potential chemotherapy-related toxicities, such as renal im-pairment, myelosuppression, fatigue, and cardiomyopathy, may increase as a result of declining organ function and diminished physiologic reserves. The recovery of normal tissues after radia-tion therapy may be delayed, and the patient may experience more severe adverse effects, such as mucositis, nausea and vomit-ing, and myelosuppression. Because of decreased tissue healing capacity and declining pulmonary and cardiovascular function-ing, the older patient is slower to recover from surgery. Elderly patients are also at increased risk for complications such as at-electasis, pneumonia, and wound infections.
Access to cancer care for elderly patients may be limited by
discriminatory or fatalistic attitudes of health care providers, care-givers,
and patients themselves. Issues such as the gradual loss of supportive
resources, declining health or loss of a spouse, and un-availability of relatives
or friends may result in limited access to care and unmet needs for assistance
with activities of daily living. In addition, the economic impact of health
care may be difficult for those living on fixed incomes.
The nurse must be aware of the special needs of the aging pop-ulation.
Cancer prevention, detection, and screening efforts are directed toward the
elderly as well as the younger population. Nurses carefully monitor elderly
patients receiving cancer treat-ments for signs and symptoms of adverse effects.
In addition, the elderly patient is instructed to report all symptoms to the
physi-cian. It is not uncommon for the elderly patient to delay report-ing
symptoms, attributing them to “old age.” Many elderly people do not want to
report illness for fear of losing their inde-pendence or financial security.
Sensory losses (eg, hearing and vi-sual losses) and memory deficits are
considered when planning patient education because they may affect the
patient’s ability to process and retain information. In such cases, the nurse
needs to act as a patient advocate, encouraging independence and identi-fying
resources for support when indicated.
Related Topics