Chapter: Medical Surgical Nursing: Oncology: Nursing Management in Cancer Care
Nursing Process: The Patient With Cancer
NURSING
PROCESS: THE PATIENT WITH CANCER
The outlook for patients with cancer has greatly improved be-cause of
scientific and technological advances. As a result of the underlying disease or
various treatment modalities, however, the patient with cancer may experience a
variety of secondary prob-lems, such as infection, reduced WBC counts,
bleeding, skin problems, nutritional problems, pain, fatigue, and psychological
stress.
Assessment
Regardless of the type of cancer treatment or prognosis, many pa-tients
with cancer are susceptible to the following problems and complications. An
important role of the nurse on the oncology team is to assess the patient for
these problems and complications.
INFECTION
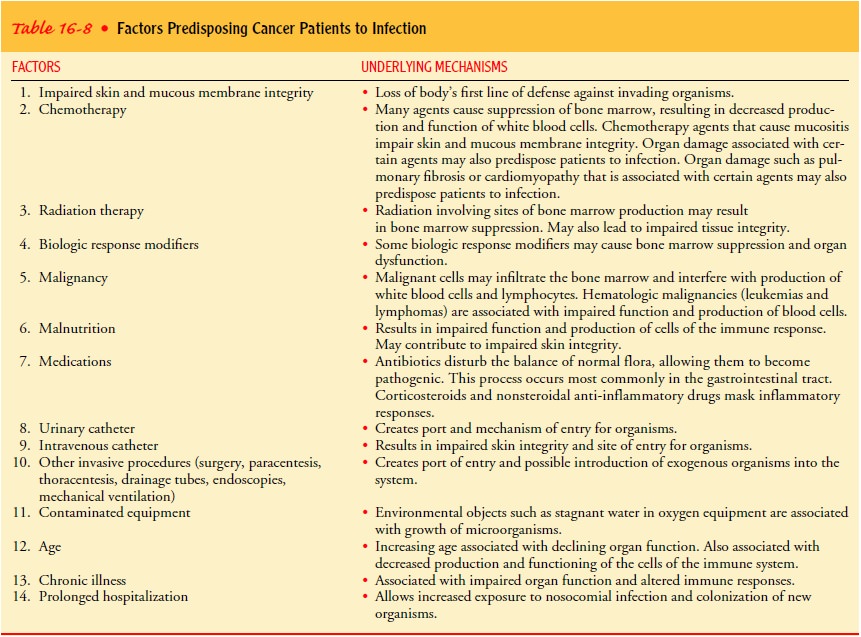
In all stages of cancer, the nurse assesses factors that can promote
infection. Infection is the leading cause of death in cancer patients. Factors
predisposing patients to infection are summarized in Table 16-8. The nurse
monitors laboratory studies to detect early changes in WBC counts. Common sites
of infection, such as the pharynx, skin, perianal area, urinary tract, and
respiratory tract, are assessed frequently. The typical signs of infection
(swelling, redness, drainage, and pain), however, may not occur in the
im-munosuppressed patient due to a diminished local inflammatory response.
Fever may be the only sign of infection that the patient exhibits. The nurse
also monitors the patient for sepsis, particu-larly if invasive catheters or
infusion lines are in place.
WBC function is often impaired in cancer patients. A decrease in
circulating WBCs is referred to as leukopenia or granulocytope-nia. There are
three types of WBCs: neutrophils, basophils, and eosinophils. The neutrophils,
totaling 60% to 70% of all the body’s WBCs, play a major role in combating
infection by engulfing and destroying infective agents in a process called
phagocytosis. Both the total WBC count and the concentration of neutrophils are
im-portant in determining the patient’s ability to fight infection.
A differential WBC count
identifies the relative numbers of WBCs and permits tabulation of
polymorphonuclear neu-trophils (mature neutrophils, reported as “polys,” PMNs,
or “segs”) and immature forms of neutrophils (reported as bands,
metamyelocytes, and “stabs”). These numbers are compiled and reported as the
absolute neutrophil count (ANC). The ANC is calculated by the following
formula:
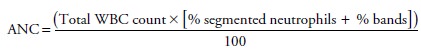
For example, if the
patient’s total WBC count is 6,000, with segmented neutrophils 25% and bands
25%, the ANC would be 3,000.
Neutropenia, an
abnormally low ANC, is associated with an increased risk for infection. The
risk for infection rises as the ANC decreases and persists. An ANC of less than
1,000 cells/mm3 re-flects a severe risk
for infection.Nadir is the lowest
ANC after myelosuppressive chemotherapy or radiation therapy. Therapies that
suppress bone marrow function are called myelosuppressive. Febrile patients who
are neutropenic are assessed for infection through cultures of blood, sputum,
urine, stool, catheter, or wounds, if appropriate. In addition, a chest x-ray
is often included to assess for pulmonary infections.
BLEEDING
The nurse assesses cancer patients for factors that may contribute to
bleeding. These include bone marrow suppression from radi-ation, chemotherapy,
and other medications that interfere with coagulation and platelet functioning,
such as aspirin, dipyri-damole (Persantine), heparin, or warfarin (Coumadin).
Com-mon bleeding sites include skin and mucous membranes; the intestinal,
urinary, and respiratory tracts; and the brain. Gross hem-orrhage, as well as
blood in the stools, urine, sputum, or vomitus (melena, hematuria, hemoptysis,
hematemesis), oozing at injec-tion sites, bruising (ecchymosis), petechiae, and
changes in men-tal status, are monitored and reported.
SKIN PROBLEMS
The integrity of skin and tissue is at risk in cancer patients be-cause of the effects of chemotherapy, radiation therapy, surgery, and invasive procedures carried out for diagnosis and therapy. As part of the assessment, the nurse identifies which of these pre-disposing factors are present and assesses the patient for other risk factors, including nutritional deficits, bowel and bladder incon-tinence, immobility, immunosuppression, multiple skin folds, and changes related to aging. Skin lesions or ulcerations sec-ondary to the tumor are noted. Alterations in tissue integrity throughout the gastrointestinal tract are particularly bothersome to the patient. Any lesions of the oral mucous membranes are noted, as are their effects on the patient’s nutritional status and comfort level.
HAIR LOSS
Alopecia (hair loss) is another form of tissue
disruption commonto cancer patients who receive radiation therapy or
chemother-apy. In addition to noting hair loss, the nurse also assesses the
psy-chological impact of this side effect on the patient and the family.
NUTRITIONAL CONCERNS
Assessing the patient’s nutritional status is an important nursing role.
Impaired nutritional status may contribute to disease pro-gression, immune
incompetence, increased incidence of infec-tion, delayed tissue repair,
diminished functional ability, and decreased capacity to continue
antineoplastic therapy. Altered nutritional status, weight loss, and cachexia
(muscle wasting, emaciation) may be secondary to decreased protein and caloric
intake, metabolic or mechanical effects of the cancer, systemic disease, side
effects of the treatment, or the emotional status of the patient.
The patient’s weight and caloric intake are monitored on a consistent
basis. Other information obtained through assessment includes diet history, any
episodes of anorexia, changes in appetite, situations and foods that aggravate
or relieve anorexia, and med-ication history. Difficulty in chewing or
swallowing is determined and the occurrence of nausea, vomiting, or diarrhea is
noted.
Clinical and laboratory data useful in assessing the patient’s
nutritional status include anthropometric measurements (triceps skin fold and
middle-upper arm circumference), serum protein levels (albumin and
transferrin), serum electrolytes, lymphocyte count, skin response to
intradermal injection of antigens, hemo-globin levels, hematocrit, urinary
creatinine levels, and serum iron levels.
PAIN
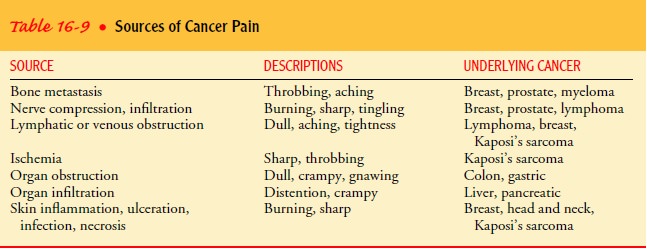
Pain and discomfort in
cancer may be related to the underlying disease, pressure exerted by the tumor,
diagnostic procedures, or the cancer treatment itself. As in any other
situation involving pain, cancer pain is affected by both physical and
psychosocial in-fluences.
In addition to assessing the source and site of pain, the nurse also
assesses those factors that increase the patient’s perception of pain, such as
fear and apprehension, fatigue, anger, and social iso-lation. Pain assessment
scales are useful in assess ing the
patient’s pain level before pain-relieving interventions are instituted and in
evaluating their effectiveness.
FATIGUE
Acute fatigue, which occurs after an energy-demanding experi-ence,
serves a protective function; chronic fatigue, however, does not. It is often
overwhelming, excessive, and not respon-sive to rest, and it seriously affects
quality of life. Fatigue is the most commonly reported side effect in patients
who receive chemotherapy and radiation therapy. The nurse assesses for
feel-ings of weariness, weakness, lack of energy, inability to carry out
necessary and valued daily functions, lack of motivation, and in-ability to
concentrate. Patients may become less verbal and ap-pear pallid, with relaxed
facial musculature. The nurse assesses physiologic and psychological stressors
that can contribute to fa-tigue, including pain, nausea, dyspnea, constipation,
fear, and anxiety. (See Nursing Research Profile 16-2.)
PSYCHOSOCIAL STATUS
Nursing assessment also
focuses on the patient’s psychological and mental status as the patient and the
family face this life-threatening experience, unpleasant diagnostic tests and
treatment modalities, and progression of disease. The patient’s mood and
emotional reaction to the results of diagnostic testing and prog-nosis are
assessed, along with evidence that the patient is pro-gressing through the
stages of grief and can talk about the diagnosis and prognosis with the family.
BODY IMAGE
Cancer patients are
forced to cope with many assaults to body image throughout the course of
disease and treatment. Entry into the health care system is often accompanied
by deperson-alization. Threats to self-concept are enormous as patients face
the realization of illness, possible disability, and death. To ac-commodate
treatments or because of the disease, many cancer patients are forced to alter
their lifestyles. Priorities and values change when body image is threatened.
Disfiguring surgery, hair loss, cachexia, skin changes, altered communication
pat-terns, and sexual dysfunction are some of the devastating results of cancer
and its treatment that threaten the patient’s self-esteem and body image. The nurse
identifies these potential threats and assesses the patient’s ability to cope
with these changes.
Diagnosis
NURSING DIAGNOSES
Based on the assessment
data, nursing diagnoses of the patient with cancer may include the following:
·
Impaired oral mucous membrane
·
Impaired tissue integrity
·
Impaired tissue integrity: alopecia
·
Impaired tissue integrity: malignant skin lesions
·
Imbalanced nutrition, less than body requirements
·
Anorexia
·
Malabsorption
·
Cachexia
·
Chronic pain
·
Fatigue
·
Disturbed body image
· Anticipatory grieving
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment
data, potential complications that may develop include the following:
•
Infection and sepsis
•
Hemorrhage
•
Superior vena cava syndrome
•
Spinal cord compression
•
Hypercalcemia
•
Pericardial effusion
•
Disseminated intravascular coagulation
•
Syndrome of inappropriate secretion of antidiuretic
hor-mone
•
Tumor lysis syndrome
See the later section,
Oncologic Emergencies, for more information.
Planning and Goals
The major goals for the
patient may include management of stomatitis, maintenance of tissue integrity,
maintenance of nu-trition, relief of pain, relief of fatigue, improved body
image, effective progression through the grieving process, and absence of
complications.
Nursing Interventions
The patient with cancer
is at risk for various adverse effects of therapy and complications. The nurse
in all health care settings, including the home, assists the patient and family
in managing these problems.
MANAGING STOMATITIS
Stomatitis, an inflammatory response of the oral tissues, commonlydevelops within
5 to 14 days after the patient receives certain chemotherapeutic agents, such
as doxorubicin and 5-fluorouracil, and BRMs, such as IL-2 and IFN. As many as
40% of patients receiving chemotherapy experience some degree of stomatitis
during treatment. Patients receiving dose-intensive chemother-apy (considerably
higher doses than conventional dosing), such as those undergoing BMT, are at
increased risk for stomatitis. Stomatitis may also occur with radiation to the
head and neck. Stomatitis is characterized by mild redness (erythema) and edema
or, if severe, by painful ulcerations, bleeding, and secondary in-fection. In
severe cases of stomatitis, cancer therapy may be tem-porarily halted until the
inflammation decreases.
As a result of normal
everyday wear and tear, the epithelial cells that line the oral cavity undergo
rapid turnover and slough off routinely. Chemotherapy and radiation interfere
with the body’s ability to replace those cells. An inflammatory response
develops as denuded areas appear in the oral cavity. Poor oral hygiene,
existing dental disease, use of other medications that dry mucous membranes,
and impaired nutritional status contribute to morbidity associated with
stomatitis. Radiation-induced xe-rostomia (dry mouth) associated with decreased
function of the salivary glands may contribute to stomatitis in patients who
have received radiation to the head and neck.
Myelosuppression (bone marrow depression) resulting from underlying
disease or its treatment predisposes the patient to oral bleeding and
infection. Pain associated with ulcerated oral tissues can significantly
interfere with nutritional intake, speech, and a willingness to maintain oral
hygiene.
Although multiple studies on stomatitis have been published, the optimal
prevention and treatment approaches have not been identified. However, most
clinicians agree that good oral hygiene that includes brushing, flossing, and
rinsing is necessary to minimize the risk for oral complications associated
with cancer therapies. Soft-bristled toothbrushes and nonabrasive toothpaste
prevent or reduce trauma to the oral mucosa. Oral swabs with spongelike
applicators may be used in place of a toothbrush for painful oral tissues.
Flossing may be performed unless it causes pain or unless platelet levels are
below 40,000/mm3
(0.04 × 1012/L). Oral rinses with saline solution or tap
water may be necessary for patients who cannot tolerate a toothbrush. Products
that irritate oral tissues or impair healing, such as alcohol-based mouth
rinses, are avoided. Foods that are difficult to chew or are hot or spicy are
avoided to minimize further trauma. The pa-tient’s lips are lubricated to keep
them from becoming dry and cracked. Topical anti-inflammatory and anesthetic
agents may be prescribed to promote healing and minimize discomfort. Products
that coat or protect oral mucosa are used to promote comfort and prevent
further trauma. The patient who experiences severe pain and discomfort with
stomatitis requires systemic analgesics.
Adequate fluid and food intake is encouraged. In some in-stances,
parenteral hydration and nutrition are needed. Topical or systemic antifungal
and antibiotic medications are prescribed to treat local or systemic
infections.
MAINTAINING TISSUE INTEGRITY
Some of the most frequently encountered disturbances of tissue
integrity, in addition to stomatitis, include skin and tissue reac-tions to
radiation therapy, alopecia, and metastatic skin lesions.
The patient who is experiencing skin and tissue reactions to radiation
therapy requires careful skin care to prevent further skin irritation, drying,
and damage. The skin over the affected area is handled gently; rubbing and use
of hot or cold water, soaps, pow-ders, lotions, and cosmetics are avoided. The
patient may avoid tissue injury by wearing loose-fitting clothes and avoiding
clothes that constrict, irritate, or rub the affected area. If blistering
oc-curs, care is taken not to disrupt the blisters, thus reducing the risk of
introducing bacteria. Moisture- and vapor-permeable dressings, such as
hydrocolloids and hydrogels, are helpful in pro-moting healing and reducing
pain. Aseptic wound care is indi-cated to minimize the risk for infection and
sepsis. Topical antibiotics, such as 1% silver sulfadiazine cream (Silvadene),
may be prescribed for use on areas of moist desquamation (painful, red, moist
skin).
ASSISTING PATIENTS TO COPE WITH ALOPECIA
The temporary or permanent thinning or complete loss of hair is a
potential adverse effect of various radiation therapies and chemotherapeutic
agents. The extent of alopecia depends on the dose and duration of therapy.
These treatments cause alope-cia by damaging stem cells and hair follicles. As
a result, the hair is brittle and may fall out or break off at the surface of
the scalp. Loss of other body hair is less frequent. Hair loss usually begins
within 2 to 3 weeks after the initiation of treatment; regrowth begins within 8
weeks after the last treatment. Some patients who undergo radiation to the head
may sustain permanent hair loss. Many health care providers view hair loss as a
minor prob-lem when compared with the potentially life-threatening
con-sequences of cancer. For many patients, however, hair loss is a major
assault on body image, resulting in depression, anxiety, anger, rejection, and
isolation. To patients and families, hair loss can serve as a constant reminder
of the challenges cancer places on their coping abilities, interpersonal
relationships, and sexuality.
The nurse’s role is to provide information about alopecia and to support
the patient and family in coping with disturbing ef-fects of therapy, such as
hair loss and changes in body image. Pa-tients are encouraged to acquire a wig
or hairpiece before hair loss occurs so that the replacement matches their own
hair. Use of at-tractive scarves and hats may make the patient feel less
conspicu-ous. Nurses can refer patients to supportive programs, such as “Look
Good, Feel Better,” offered by the American Cancer Society. Knowledge that hair usually begins to
regrow after complet-ing therapy may comfort some patients, although the color
and texture of the new hair may be different.
MANAGING MALIGNANT SKIN LESIONS
Skin lesions may occur with local extension of the tumor or
em-bolization of the tumor into the epithelium and its surrounding lymph and
blood vessels. Secondary growth of cancer cells into the skin may result in
redness (erythematous areas) or can progress to wounds involving tissue
necrosis and infection. The most extensive lesions tend to disintegrate and are
purulent and malodorous. In addition, these lesions are a source of
consider-able pain and discomfort. Although this type of lesion is most often
associated with breast cancer and head and neck cancers, it can also occur with
lymphoma, leukemia, melanoma, and can-cers of the lung, uterus, kidney, colon,
and bladder. The devel-opment of severe skin lesions is usually associated with
a poor prognosis for extended survival.
Ulcerating skin lesions usually indicate widely disseminated disease
unlikely to be eradicated. Managing these lesions becomes a nursing priority.
Nursing care includes carefully assessing and cleansing the skin, reducing
superficial bacteria, controlling bleeding, reducing odor, and protecting the
skin from pain and further trauma. The patient and family require assistance
and guidance to care for these skin lesions at home. Referral for home care is
indicated.
PROMOTING NUTRITION
Most cancer patients experience some weight loss during their ill-ness.
Anorexia, malabsorption, and cachexia are examples of nu-tritional problems
that commonly occur in cancer patients; special attention is needed to prevent
weight loss and promote nutrition.
Anorexia
Among the many causes of anorexia in the cancer patient are alterations
in taste, manifested by increased salty, sour, and metal-lic taste sensations,
and altered responses to sweet and bitter flavors, leading to decreased
appetite, decreased nutritional in-take, and protein-calorie malnutrition.
Taste alterations may re-sult from mineral (eg, zinc) deficiencies, increases
in circulating amino acids and cellular metabolites, or the administration of
chemotherapeutic agents. Patients undergoing radiation therapy to the head and
neck may experience “mouth blindness,” which is a severe impairment of taste.
Alterations in the sense of smell also alter taste; this is a com-mon
experience of patients with head and neck cancers. Anorexia may occur because
the person feels full after eating only a small amount of food. This sense of
fullness occurs secondary to a de-crease in digestive enzymes, abnormalities in
the metabolism of glucose and triglycerides, and prolonged stimulation of
gastric volume receptors, which convey the feeling of being full.
Psy-chological distress, such as fear, pain, depression, and isolation,
throughout illness may also have a negative impact on appetite. The person may
develop an aversion to food because of nausea and vomiting after treatment.
Malabsorption
Many cancer patients are unable to absorb nutrients from the
gas-trointestinal system as a result of tumor activity and cancer treat-ment.
Tumors can affect the gastrointestinal activity in several ways. They may
impair enzyme production or produce fistulas. They secrete hormones and
enzymes, such as gastrin; this leads toincreased gastrointestinal irritation, peptic
ulcer disease, and de-creased fat digestion. They also interfere with protein
digestion.
Chemotherapy and radiation can irritate and damage mu-cosal cells of the
bowel, inhibiting absorption. Radiation ther-apy can cause sclerosis of the
blood vessels in the bowel and fibrotic changes in the gastrointestinal tissue.
Surgical interven-tion may change peristaltic patterns, alter gastrointestinal
secre-tions, and reduce the absorptive surfaces of the gastrointestinal mucosa,
all leading to malabsorption.
Cachexia
Cachexia is common in patients with cancer, especially in ad-vanced
disease. Cancer cachexia is related to inadequate nutri-tional intake along
with increasing metabolic demand, increased energy expenditure due to anaerobic
metabolism of the tumor, impaired glucose metabolism, competition of the tumor
cells for nutrients, altered lipid metabolism, and a suppressed appetite. It is
characterized by loss of body weight, adipose tissue, visceral protein, and
skeletal muscle. Patients who are cachectic complain of loss of appetite, early
satiety, and fatigue. As a result of protein losses they are often anemic and
have peripheral edema.
General Nutritional Considerations
Whenever possible, every effort is used to maintain adequate nu-trition
through the oral route. Food should be prepared in ways that make it appealing.
Unpleasant smells and unappetizing-looking foods are avoided. Family members
are included in the plan of care to encourage adequate food intake. The
patient’s preferences, as well as physiologic and metabolic requirements, are
considered when selecting foods. Small, frequent meals are provided, with
supplements between meals. Patients often toler-ate larger amounts of food
earlier in the day rather than later, so meals can be planned accordingly.
Patients should avoid drink-ing fluids while eating, to avoid early satiety.
Oral hygiene before mealtime often makes meals more pleasant. Pain, nausea, and
other symptoms that may interfere with nutrition are assessed and managed.
Medications such as corticosteroids or progestational agents such as megestrol
acetate have been used successfully as appetite stimulants.
If adequate nutrition cannot be maintained by oral intake, nu-tritional
support via the enteral route may be necessary. Short-term nutritional
supplementation may be provided through a nasogastric tube. However, if
nutritional support is needed be-yond several weeks, a gastrostomy or
jejunostomy tube may be inserted. Patients and families are taught to
administer enteral nutrition in the home setting.
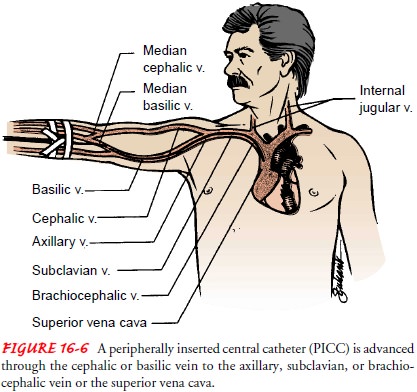
If malabsorption is a
problem, enzyme and vitamin replace-ment may be instituted. Additional
strategies include changing the feeding schedule, using simple diets, and
relieving diarrhea. If malabsorption is severe, parenteral nutrition (PN) may
be nec-essary. PN can be administered in several ways: by a long-term venous
access device, such as a right atrial catheter, an implanted venous port, or a
peripherally inserted central catheter (Fig. 16-6). The nurse teaches the
patient and family to care for venous access devices and to administer PN. Home
care nurses may assist with or supervise PN in the home.
Interventions to reduce cachexia usually do not prolong sur-vival but may improve the patient’s quality of life. Before inva-sive nutritional strategies are instituted, the nurse should assess the patient carefully and discuss the options with the patient and family. Creative dietary therapies, enteral (tube) feedings, or PN may be necessary to ensure adequate nutrition. Nursing care is also directed toward preventing trauma, infection, and other complications that increase metabolic demands.
RELIEVING PAIN
Of all patients with
progressive cancer, more than 75% experi-ence pain (Yarbro, Hansen-Frogge &
Goodman, 1999). Although patients with cancer may have acute pain, their pain
is more frequently characterized as chronic. As in other situations in-volving
pain, the experience of cancer pain is influenced by both physical and
psychosocial factors.
Cancer can cause pain in various ways (Table 16-9). Pain is also
associated with various cancer treatments. Acute pain is linked with trauma from
surgery. Occasionally, chronic pain syn-dromes, such as postsurgical
neuropathies (pain related to nerve tissue injury), occur. Some
chemotherapeutic agents cause tissue necrosis, peripheral neuropathies, and
stomatitis—all potential sources of pain—whereas radiation therapy can cause
pain sec-ondary to skin or organ inflammation. Cancer patients may have other
sources of pain, such as arthritis or migraine headaches, that are unrelated to
the underlying cancer or its treatment.
In today’s society, most people expect pain to disappear or re-solve
quickly, and in fact it usually does. Although controllable, cancer pain is
commonly irreversible and not quickly resolved.For many patients, pain is a
signal that the tumor is growing and that death is approaching. As the patient
anticipates the pain and anxiety increases, pain perception heightens,
producing fear and further pain. Chronic cancer pain, then, can be best
de-scribed as a cycle progressing from pain to anxiety to fear and back to pain
again.
Pain tolerance, the point past which pain can no longer be tol-erated,
varies among people. Pain tolerance is decreased by fa-tigue, anxiety, fear of
death, anger, powerlessness, social isolation, changes in role identity, loss
of independence, and past experi-ences. Adequate rest and sleep, diversion,
mood elevation, empa-thy, and medications such as antidepressants, antianxiety
agents, and analgesics enhance tolerance to pain.
Inadequate pain management is most often the result of mis-conceptions
and insufficient knowledge about pain assessment and pharmacologic
interventions on the part of patients, fami-lies, and health care providers.
Successful management of cancer pain is based on thorough and objective pain
assessment that ex-amines physical, psychosocial, environmental, and spiritual
fac-tors. A multidisciplinary team approach is essential to determine optimal
management of the patient’s pain. Unlike instances of chronic nonmalignant
pain, systemic analgesics play a central role in managing cancer pain.
The World Health Organization (Dalton & Youngblood, 2000) advocates
a three-step approach to treating cancer pain. Analgesics are administered
based on the pa-tient’s level of pain. Nonopioid analgesics (eg, acetaminophen)
are used for mild pain; weak opioid analgesics (eg, codeine) are used for
moderate pain; and strong opioid analgesics (eg, mor-phine) are used for severe
pain. If the patient’s pain escalates, the strength of the analgesic medication
is increased until the pain is controlled. Adjuvant medications are also
administered to en-hance the effectiveness of analgesics and to manage other
symp-toms that may contribute to the pain experience. Examples of adjuvant
medications include antiemetics, antidepressants, anx-iolytics, antiseizure
agents, stimulants, local anesthetics, radio-pharmaceuticals (radioactive
agents that may be used to treat painful bone tumors), and corticosteroids.
Preventing and reducing
pain help to decrease anxiety and break the pain cycle. This can be
accomplished best by admin-istering analgesics on a regularly scheduled basis
as prescribed (the preventive approach to pain management), with additional
analgesics administered for breakthrough pain as needed and as prescribed.
Various pharmacologic and nonpharmacologic approaches offer the best methods of managing cancer pain. No reasonable approaches, even those that may be invasive, should be over looked because of a poor or terminal prognosis.
Nurses help pa-tients and families to take an active
role in managing pain. Nurses provide education and support to correct fears
and misconcep-tions about opioid use. Inadequate pain control leads to
suffer-ing, anxiety, fear, immobility, isolation, and depression. Improving a
patient’s quality of life is as important as preventing a painful death.
DECREASING FATIGUE
In recent years, fatigue has been recognized as one of the most
sig-nificant and frequent symptoms experienced by patients receiving cancer
therapy. Nurses help the patient and family to understand that fatigue is
usually an expected and temporary side effect of the cancer process and of many
treatments used. Fatigue also stems from the stress of coping with cancer. It
does not always signify that the cancer is advancing or that the treatment is
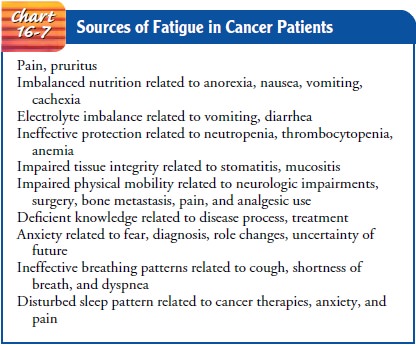
failing. Po-tential sources of fatigue are summarized in Chart 16-7.
Nursing strategies are
implemented to minimize fatigue or as-sist the patient to cope with existing
fatigue. Helping the patient to identify sources of fatigue aids in selecting
appropriate and in-dividualized interventions. Ways to conserve energy are
developed to help the patient plan daily activities. Alternating periods of
rest and activity are beneficial. Regular, light exercise may decrease fa-tigue
and facilitate coping, whereas lack of physical activity and “too much rest”
can actually contribute to deconditioning and as-sociated fatigue.
Patients are encouraged
to maintain as normal a lifestyle as possible by continuing with those
activities they value and enjoy. Prioritizing necessary and valued activities
can assist patients in planning for each day. Both patients and families are
encouraged to plan to reallocate responsibilities, such as attending to child
care, cleaning, and preparing meals. Patients who are employed full-time may
need to reduce the number of hours worked each week. The nurse assists the
patient and family in coping with these changing roles and responsibilities.
Nurses also address factors that contribute to fatigue and implement pharmacologic and nonpharmacologic strategies to manage pain. Nutrition counseling is provided to patients who are not eating enough calories or protein. Small, frequent meals require less energy for digestion. Serum hemoglobin and hemat-ocrit levels are monitored for deficiencies, and blood products or EPO are administered as prescribed. Patients are monitored for alterations in oxygenation and electrolyte balances. Physical therapy and assistive devices are beneficial for patients with impaired mobility.
IMPROVING BODY IMAGE AND SELF-ESTEEM
A positive approach is essential when caring for the patient with an
altered body image. To help the patient retain control and positive
self-esteem, it is important to encourage independence and con-tinued
participation in self-care and decision making. The patient should be assisted
to assume those tasks and participate in those ac-tivities that are personally
of most value. Any negative feelings that the patient has or threats to body
image should be identified and discussed. The nurse serves as a listener and
counselor to both the patient and the family. Referral to a support group can
provide the patient with additional assistance in coping with the changes
re-sulting from cancer or its treatment. In many cases, a cosmetolo-gist can
provide ideas about hair or wig styling, make-up, and the use of scarves and
turbans to help with body image concerns.
Patients who experience alterations in sexuality and sexual function are
encouraged to discuss concerns openly with their partner. Alternative forms of
sexual expression are explored with the patient and partner to promote positive
self-worth and ac-ceptance. The nurse who identifies serious physiologic,
psycho-logical, or communication difficulties related to sexuality or sexual
function is in a key position to assist the patient and part-ner to seek
further counseling if necessary.
ASSISTING IN THE GRIEVING PROCESS
A cancer diagnosis need not indicate a fatal outcome. Many forms of
cancer are curable; others may be cured if treated early. Despite these facts,
many patients and their families view cancer as a fatal disease that is
inevitably accompanied by pain, suffering, debil-ity, and emaciation. Grieving
is a normal response to these fears and to the losses anticipated or
experienced by the patient with cancer. These may include loss of health,
normal sensations, body image, social interaction, sexuality, and intimacy. The
patient, family, and friends may grieve for the loss of quality time to spend
with others, the loss of future and unfulfilled plans, and the loss of control
over one’s own body and emotional reactions.
The patient and family
just informed of the cancer diagnosis frequently respond with shock, numbness,
and disbelief. It is often during this stage that the patient and family are
called on to make important initial decisions about treatment. They re-quire
the support of the physician, nurse, and other health care team members to make
these decisions. An important role of the nurse is to answer any questions the
patient and family have and clarify information provided by the physician.
In addition to assessing
the response of the patient and family to the diagnosis and planned treatment,
the nurse assists them in framing their questions and concerns, identifying
resources and support people (eg, spiritual advisor, counselor), and
communi-cating their concerns with each other. Support groups for patients and
families are available through hospitals and various commu-nity organizations.
These groups provide direct assistance, advice, and emotional support.
As the patient and family progress through the grieving process, they
may express anger, frustration, and depression. Dur-ing this time, the nurse
encourages the patient and family to ver-balize their feelings in an atmosphere
of trust and support. The nurse continues to assess their reactions and
provides assistance and support as they confront and learn to deal with new
problems.
If the patient enters the terminal phase of disease, the nurse may
realize that the patient and family members are at different stages of grief.
In such cases, the nurse assists the patient and family to acknowledge and cope
with their reactions and feelings. Nurses also assist patients and families to
explore preferences for issues related to end-of-life care such as withdrawal
of active disease treatment, desire for the use of life support measures, and
symptom manage-ment. Support, which can be as simple as holding the patient’s
hand or just being with the patient at home or at the bedside, often
contributes to peace of mind. Maintaining contact with the sur-viving family
members after the death of the cancer patient may help them to work through
their feelings of loss and grief.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Despite advances in cancer care, infection remains the leading cause of
death. In the cancer patient, defense against infection is compromised in many
different ways. The integrity of the skin and mucous membrane, the body’s first
line of defense, is chal-lenged by multiple invasive diagnostic and therapeutic
proce-dures, by adverse effects of radiation and chemotherapy, and by the
detrimental effects of immobility.
Impaired nutrition resulting from anorexia, nausea, vomiting, diarrhea,
and the underlying disease alters the body’s ability to combat invading
organisms. Medications such as antibiotics dis-turb the balance of normal
flora, allowing the overgrowth of path-ogenic organisms. Other medications can
also alter the immune response. Cancer itself may be immunosuppres-sive.
Cancers such as leukemia and lymphoma are often associ-ated with defects in
cellular and humoral immunity. Advanced cancer can lead to obstruction by the
tumor of the hollow viscera (such as the intestines), blood vessels, and lymphatic
vessels, cre-ating a favorable environment for proliferation of pathogenic
organisms. In some patients, tumor cells infiltrate bone marrow and prevent
normal production of WBCs. Most often, however, a decrease in WBCs is a result
of bone marrow suppression after chemotherapy or radiation therapy.
The use of the
hematopoietic growth factors, also called colony-stimulating factors (see the
previous discussion of BRM therapy), has reduced the severity and duration of
neutropenia associated with myelosuppressive chemotherapy and radiation
therapy. The administration of these factors assists in reducing the risk for
infection and, possibly, in maintaining treatment schedules, drug dosages,
treatment effectiveness, and the quality of life.
Infection
Gram-positive organisms, such as Streptococcus
and Staphylococcus species, are the
most frequently isolated causes of infection. Gram-negative organisms, such as Escherichia coli and Pseudomonasaeruginosa, and fungal
organisms, such as Candida albicans, alsocontribute
to the incidence of serious infection.
Fever is probably the
most important sign of infection in the immunocompromised patient. Although
fever may be related to a variety of noninfectious conditions, including the
underlying cancer, any temperature of 38.3°C (101°F) or
higher is reported and dealt with promptly.
Antibiotics may be prescribed to treat infections after cultures of
wound drainage, exudate, sputum, urine, stool, or blood are obtained. Patients
with neutropenia are treated with broad-spectrum antibiotics before the
infecting organism is identified because of the high incidence of mortality
associated with un-treated infection. Broad-spectrum antibiotic coverage or
empiric therapy most often includes a combination of medications todefend the body against
the major pathogenic organisms. An important component of the nurse’s role is
to administer these medications promptly according to the prescribed schedule
to achieve adequate blood levels of the medications.
Strict asepsis is essential when handling intravenous lines, catheters,
and other invasive equipment. Exposure of the patient to others with an active
infection and to crowds is avoided. Pa-tients with profound immunosuppression,
such as BMT recipi-ents, may need to be placed in a protective environment
where the room and its contents are sterilized and the air is filtered. These
patients may also receive low-bacteria diets, avoiding fresh fruits and
vegetables. Hand hygiene and appropriate general hygiene are necessary to
reduce exposure to potentially harmful bacteria and to eliminate environmental
contaminants. Invasive procedures, such as injections, vaginal or rectal
examinations, rectal temperatures, and surgery, are avoided. The patient is
encouraged to cough and perform deep-breathing exercises fre-quently to prevent
atelectasis and other respiratory problems. Prophylactic antimicrobial therapy
may be used for patients who are expected to be profoundly immunosuppressed and
at risk for certain infections. The nurse teaches the patient and family to
recognize signs and symptoms of infection to report, perform effective hand
hygiene, use antipyretics, maintain skin integrity, and administer
hematopoietic growth factors when indicated.
Septic Shock
The nurse assesses the patient frequently for infection and
in-flammation throughout the course of the disease. Septicemia and septic shock
are life-threatening complications that must be pre-vented or detected and
treated promptly. Patients with signs and symptoms of impending sepsis and septic
shock require immedi-ate hospitalization and aggressive treatment.
Signs and symptoms of
septic shock include al-tered mental
status, either subnormal or elevated temperature, cool and clammy skin,
decreased urine output, hypotension, dys-rhythmias, electrolyte imbalances, and
abnormal arterial blood gas values. The patient and family members are
instructed about signs of septicemia, methods for preventing infection, and
actions to take if infection or septicemia occurs.
Septic shock is most often associated with overwhelming gram-negative
bacterial infections. The nurse monitors the blood pressure, pulse rate,
respirations, and temperature of the patient with shock every 15 to 30 minutes.
Neurologic assess-ments are carried out to detect changes in orientation and
re-sponsiveness. Fluid and electrolyte status is monitored by measuring fluid
intake and output and serum electrolytes. Arte-rial blood gas values and pulse
oximetry are monitored to deter-mine tissue oxygenation. The nurse administers
intravenous fluids, blood products, and vasopressors as prescribed to main-tain
the patient’s blood pressure and tissue perfusion. Supple-mental oxygen is
often necessary. Broad-spectrum antibiotics are administered as prescribed to
combat the underlying infection.
Bleeding and Hemorrhage
Thrombocytopenia, a
decrease in the circulating platelet count, is the most common cause of
bleeding in cancer patients and is usually defined as a count of less than
100,000/mm3 (0.1 × 1012/L). When the count falls
between 20,000 and 50,000/mm3 (0.02 to 0.05 × 1012/L), the
risk for bleeding increases. Counts under 20,000/mm3 (0.02 × 1012/L) are
associated with an in-creased risk for spontaneous bleeding, for which the
patient re-quires a platelet transfusion. Platelets are essential for normal
blood clotting and coagulation (hemostasis). Thrombocytopenia often results
from bone marrow depres-sion after certain types of chemotherapy and radiation
therapy. Tumor infiltration of the bone marrow can also impair the nor-mal
production of platelets. In some cases, platelet destruction is associated with
an enlarged spleen (hypersplenism) and abnormal antibody function that occur
with leukemia and lymphoma.
In addition to monitoring laboratory values, the
nurse con-tinues to assess the patient for bleeding. The nurse also takes steps
to prevent trauma and minimize the risk for bleeding by encour-aging the
patient to use a soft, not stiff, toothbrush and an elec-tric, not
straight-edged, razor. Additionally, the nurse avoids unnecessary invasive
procedures (eg, rectal temperatures, intra-muscular injections, and
catheterization) and assists the patient and family to identify and remove
environmental hazards that may lead to falls or other trauma. Soft foods,
increased fluid in-take, and stool softeners, if prescribed, may be indicated
to reduce trauma to the gastrointestinal tract. The joints and extremities are
handled and moved gently to minimize the risk for spontaneous bleeding. The
nurse may administer IL-11, which has been ap-proved by the FDA (Rust, Wood
& Battiato, 1999) to prevent severe thrombocytopenia and to reduce the need
for platelet transfusions following myelosuppressive chemotherapy in pa-tients
with nonmyeloid malignancies. In some instances, the nurse teaches the patient
or family member to administer IL-11 in the home.
Hemorrhage may be related to various underlying
abnormal-ities, such as thrombocytopenia and coagulation disorders. These
clinical situations are often associated with the cancer itself or the adverse
effects of cancer treatments. Sites of hemorrhage may in-clude the
gastrointestinal, respiratory, and genitourinary tracts and the brain. Blood
pressure and pulse and respiratory rates are monitored every 15 to 30 minutes
when hospitalized patients ex-perience bleeding.
Serum hemoglobin and hematocrit are monitored
carefully for changes indicating blood loss. The nurse tests all urine, stool,
and emesis for occult blood. Neurologic assessments are per-formed to detect
changes in orientation and behavior. The nurse administers fluids and blood
products as prescribed to replace any losses. Vasopressor agents are
administered as prescribed to main-tain blood pressure and ensure tissue
oxygenation. Supplemental oxygen is used as necessary.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patients with cancer usually return home from acute care facili-ties or
receive treatment in the home or outpatient area rather than acute care
facilities. The shift from the acute care setting also shifts the responsibility
for care to the patient and family. As a re-sult, families and friends must
assume increased involvement in patient care, which requires teaching that
enables them to pro-vide care. Teaching initially focuses on providing
information needed by the patient and family to address the most immediate care
needs likely to be encountered at home.
Side effects of treatments and changes in the patient’s status that
should be reported are reviewed verbally and reinforced with writ-ten
information. Strategies to deal with side effects of treatment are discussed
with the patient and family. Other learning needs are identified based on the
priorities conveyed by the patient and family as well as on the complexity of
care provided in the home.
Technological advances allow home administration of chemo-therapy, PN,
blood products, parenteral antibiotics, and parenteral analgesics; management
of symptoms; and care of vascu-lar access devices. Although home care nurses
provide care and support for patients receiving this advanced technical care,
the patient and family need instruction and ongoing support that allow them to
feel comfortable and proficient in managing these treatments at home. Follow-up
visits and telephone calls from the nurse are often reassuring to the patient
and family and increase their comfort in dealing with complex and new aspects
of care. Continued contact facilitates evaluation of the patient’s progress and
ongoing needs.
Continuing Care
Referral for home care
is often indicated for the patient with can-cer. The responsibilities of the
home care nurse include assessing the home environment, suggesting
modifications in the home or in care to assist the patient and family in
addressing the patient’s physical needs, providing physical care, and assessing
the psy-chological and emotional impact of the illness on the patient and
family.
Assessing changes in the
patient’s physical status and report-ing relevant changes to the physician help
to ensure that appro-priate and timely modifications in therapy are made. The
home care nurse also assesses the adequacy of pain management and the
effectiveness of other strategies to prevent or manage the side ef-fects of
treatment modalities.
The patient’s and
family’s understanding of the treatment plan and management strategies is
assessed, and previous teach-ing is reinforced. The nurse often facilitates the
coordination of patient care by maintaining close communication with all health
care providers involved in the patient’s care. The nurse may make referrals and
coordinate available community resources (eg, local office of the American
Cancer Society, home aides, church groups, parish nurses, and support groups)
to assist patients and caregivers.
Evaluation
EXPECTED PATIENT OUTCOMES
For specific patient
outcomes, see the Plan of Nursing Care. Ex-pected patient outcomes may include:
·
Maintains integrity of oral mucous membranes
·
Maintains adequate tissue integrity
·
Maintains adequate nutritional status
·
Achieves relief of pain and discomfort
·
Demonstrates increased activity tolerance and
decreased fatigue
·
Exhibits improved body image and self-esteem
·
Progresses through the grieving process
·
Experiences no complications, such as infection, or
sepsis, and no episodes of bleeding or hemorrhage
Related Topics