Chapter: Medical Surgical Nursing: Fluid and Electrolytes: Balance and Distribution
Sodium Excess (Hypernatremia)
SODIUM
EXCESS (HYPERNATREMIA)
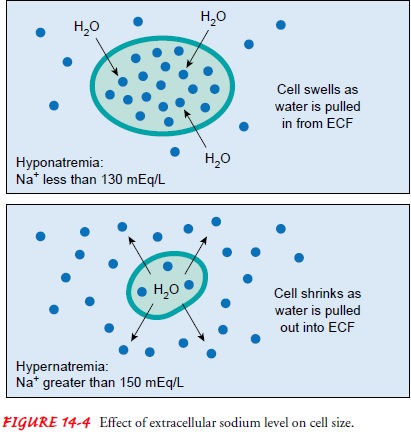
Hypernatremia is a higher-than-normal serum sodium level (ex-ceeding 145
mEq/L [145 mmol/L]) (Adrogue & Madias, 2000a). It can be caused by a gain
of sodium in excess of water or by a loss of water in excess of sodium. It can
occur in patients with normal fluid volume or in those with FVD or FVE. With a
water loss, the patient loses more water than sodium; as a result, the serumsodium concentration
increases and the increased concentration pulls fluid out of the cell. This is
both an extracellular and intra-cellular FVD. In sodium excess, the patient
ingests or retains more sodium than water.
Pathophysiology
A common cause of hypernatremia is fluid deprivation in uncon-scious
patients who cannot perceive, respond to, or communicate their thirst (Adrogue
& Madias, 2000a). Most often affected in this regard are very old, very
young, and cognitively impaired patients. Administration of hypertonic enteral
feedings without adequate water supplements leads to hypernatremia, as does
wa-tery diarrhea and greatly increased insensible water loss (eg,
hyper-ventilation, denuding effects of burns).
Diabetes insipidus, a
deficiency of ADH from the posterior pituitary gland, leads to hypernatremia if
the patient does not ex-perience, or cannot respond to, thirst or if fluids are
excessively restricted. Less common causes are heat stroke, near-drowning in
sea water (which contains a sodium concentration of approxi-mately 500 mEq/L),
and malfunction of either hemodialysis or peritoneal dialysis proportioning
systems. IV administration of hypertonic saline or excessive use of sodium
bicarbonate also causes hypernatremia.
Clinical Manifestations
The clinical manifestations of hypernatremia are primarily neuro-logic
and are presumably the consequence of cellular dehydration (Adrogue &
Madias, 2000a). Hypernatremia results in a rela-tively concentrated ECF,
causing water to be pulled from the cells (see Fig. 14-4). Clinically, these
changes may be manifested by restlessness and weakness in moderate
hypernatremia and by dis-orientation, delusions, and hallucinations in severe
hypernatremia. Dehydration (resulting in hypernatremia) is often overlooked as
the primary reason for behavioral changes in the elderly patient. If
hypernatremia is severe, permanent brain damage can occur (especially in
children). Brain damage is apparently due to sub-arachnoid hemorrhages that
result from brain contraction.
A primary characteristic of hypernatremia is thirst. Thirst is so strong
a defender of serum sodium levels in healthy people that hypernatremia never
occurs unless the person is unconscious or is denied access to water.
Unfortunately, ill people may have an impaired thirst mechanism. Other signs
include a dry, swollen tongue and sticky mucous membranes. Flushed skin,
peripheral and pulmonary edema, postural hypotension, and increased mus-cle
tone and deep tendon reflexes are additional signs and symp-toms of
hypernatremia. Body temperature may rise mildly but returns to normal when the
hypernatremia is corrected.
Assessment and Diagnostic Findings
In hypernatremia, the serum sodium level exceeds 145 mEq/L (145 mmol/L)
and the serum osmolality exceeds 295 mOsm/kg (295 mmol/L). The urine specific
gravity and urine osmolality are increased as the kidneys attempt to conserve
water (provided the water loss is from a route other than the kidneys) (Fall,
2000).
Medical Management
Hypernatremia treatment consists of a gradual lowering of the serum
sodium level by the infusion of a hypotonic electrolyte so-lution (eg, 0.3%
sodium chloride) or an isotonic nonsaline solution(eg, dextrose 5% in water [D5W]). D5W is indicated when water needs to be replaced without sodium. Many
clinicians consider a hypotonic sodium solution to be safer than D5W because it al-lows a gradual reduction in
the serum sodium level and thereby decreases the risk of cerebral edema. It is
the solution of choice in severe hyperglycemia with hypernatremia. A rapid
reduction in the serum sodium level temporarily decreases the plasma
osmo-lality below that of the fluid in the brain tissue, causing danger-ous
cerebral edema. Diuretics also may be prescribed to treat the sodium gain.
There is no consensus
about the exact rate at which serum sodium levels should be reduced. As a
general rule, the serum sodium level is reduced at a rate no faster than 0.5 to
1 mEq/L to allow sufficient time for readjustment through diffusion across
fluid compartments. Desmopressin acetate (DDAVP) may be prescribed to treat
diabetes insipidus if it is the cause of hypernatremia.
Nursing Management
As in hyponatremia, fluid losses and gains are carefully monitored in
patients at risk for hypernatremia. The nurse should assess for abnormal losses
of water or low water intake and for large gains of sodium, as might occur with
ingestion of over-the-counter medications with a high sodium content (such as
Alka-Seltzer). Also, it is important to obtain a medication history because
some prescription medications have a high sodium content. In addi-tion, the
nurse notes the patient’s thirst or elevated body tem-perature and evaluates it
in relation to other clinical signs. The nurse monitors for changes in
behavior, such as restlessness, dis-orientation, and lethargy.
PREVENTING HYPERNATREMIA
The nurse attempts to
prevent hypernatremia by offering fluids at regular intervals, particularly in
debilitated patients unable to perceive or respond to thirst. If fluid intake
remains inadequate, the nurse consults with the physician to plan an alternate
route for intake, either by enteral feedings or by the parenteral route. If
enteral feedings are used, sufficient water should be administered to keep the
serum sodium and BUN within normal limits. As a rule, the higher the osmolality
of the enteral feeding, the greater the need for water supplementation.
For patients with
diabetes insipidus, adequate water intake must be ensured. If the patient is
alert and has an intact thirst mechanism, merely providing access to water may
be sufficient. If the patient has a decreased level of consciousness or other
dis-ability interfering with adequate fluid intake, parenteral fluid
re-placement may be prescribed. This therapy can be anticipated in patients
with neurologic disorders, particularly in the early post-operative period.
CORRECTING HYPERNATREMIA
When parenteral fluids are necessary for managing hyperna-tremia, the
nurse monitors the patient’s response to the fluids by reviewing serial serum
sodium levels and by observing for changes in neurologic signs. With a gradual
decrease in the serum sodium level, the neurologic signs should improve. As
stated in the dis-cussion on management, too-rapid reduction in the serum
sodium level renders the plasma temporarily hypo-osmotic to the fluid in the
brain tissue, causing movement of fluid into brain cells and dangerous cerebral
edema (Adrogue & Madias, 2000a).
Related Topics