Chapter: Medical Surgical Nursing: Fluid and Electrolytes: Balance and Distribution
Nursing Management of the Patient Receiving IV Therapy
Nursing
Management of the Patient Receiving IV Therapy
Venipuncture, or the ability to gain access to the venous system for
administering fluids and medications, is an expected nursing skill in many
settings. This responsibility includes selecting the appropriate venipuncture
site and type of cannula and being pro-ficient in the technique of vein entry.
PREPARING TO ADMINISTER IV THERAPY
Before performing venipuncture, the nurse carries out hand hy-giene,
applies gloves, and informs the patient about the proce-dure. Next the nurse
selects the most appropriate insertion site and type of cannula for a
particular patient. Factors influencing these choices include the type of
solution to be administered, the expected duration of IV therapy, the patientŌĆÖs
general condition, and the availability of veins. The skill of the person
initiating the infusion is also an important consideration.
CHOOSING AN IV SITE
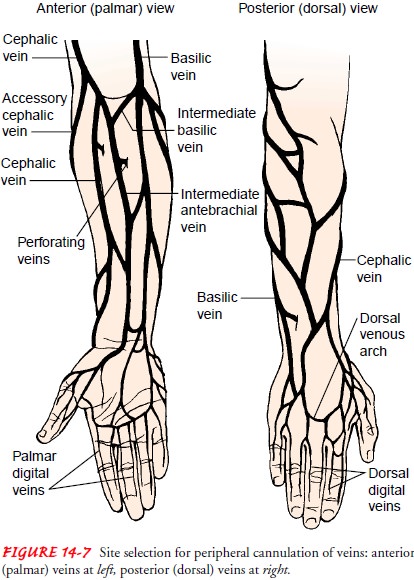
Many sites can be used for IV therapy, but ease of access and po-tential
hazards vary. Veins of the extremities are designated as pe-ripheral locations
and are ordinarily the only sites used by nurses. Because they are relatively
safe and easy to enter, arm veins are most commonly used (Fig. 14-7). The
metacarpal, cephalic, basilic, and median veins as well as their branches are
recommended sites be-cause of their size and ease of access. More distal sites
should be used first, with more proximal sites used subsequently. Leg veins
should rarely, if ever, be used because of the high risk of thromboembolism.
Additional sites to avoid include veins distal to a previous IV infil-tration
or phlebitic area, sclerosed or thrombosed veins, an arm with an arteriovenous
shunt or fistula, or an arm affected by edema, in-fection, blood clot, or skin
breakdown. The arm on the side of a mastectomy is avoided because of impaired
lymphatic flow.
Central veins commonly used by physicians include the sub-clavian and internal jugular veins. It is possible to gain access to (or cannulate) these larger vessels even when peripheral sites have collapsed, and they allow for the administration of hyperosmolar solutions. Hazards are much greater, however, and may include inadvertent entry into an artery or the pleural space.
Ideally, both arms and
hands are carefully inspected before choosing a specific venipuncture site that
does not interfere with mobility. For this reason, the antecubital fossa is
avoided, except as a last resort. The most distal site of the arm or hand is
gener-ally used first so that subsequent IV access sites can be moved
pro-gressively upward. The following are factors to consider when selecting a
site for venipuncture:
┬Ę Condition of the vein
┬Ę Type of fluid or
medication to be infused
┬Ę Duration of therapy
┬Ę PatientŌĆÖs age and size
┬Ę Whether the patient is
right- or left-handed
┬Ę PatientŌĆÖs medical
history and current health status
┬Ę Skill of the person
performing the venipuncture
After applying a
tourniquet, the nurse palpates and inspects the vein. The vein should feel
firm, elastic, engorged, and round, not hard, flat, or bumpy. Because arteries
lie close to veins in the antecubital fossa, the vessel should be palpated for
arterial pulsa-tion (even with a tourniquet on), and cannulation of pulsating vessels
should be avoided. General guidelines for selecting a can-nula include:
┬Ę Length: 3Ōüä4 to 1.25 inches long
┬Ę Diameter: narrow
diameter of the cannula to occupy mini-mal space within the vein
┬Ę Gauge: 20 to 22 gauge
for most IV fluids; a larger gauge for caustic or viscous solutions; 14 to 18
gauge for blood ad-ministration and for trauma patients and those undergoing
surgery
Hand veins are easiest
to cannulate. Cannula tips should not rest in a flexion area (eg, the
antecubital fossa) as this could in-hibit the IV flow.
SELECTING VENIPUNCTURE DEVICES
Equipment used to gain
access to the vasculature includes can-nulas, needleless IV delivery systems,
and peripherally inserted central catheter or midline catheter access lines.
Cannulas.
Most peripheral access devices are
cannulas. Theyhave an obturator inside a tube that is later removed. ŌĆ£CatheterŌĆØ
and ŌĆ£cannulaŌĆØ are terms that are used interchangeably. The main types of
cannula devices available are those referred to as winged infusion sets
(butterfly) with a steel needle or as an over-the-needle catheter with wings,
indwelling plastic cannu-las inserted over a steel needle, and indwelling
plastic cannulas inserted through a steel needle. Scalp vein or butterfly
needles are short steel needles with plastic wing handles. These are easy to
insert, but because they are small and nonpliable, infiltration occurs easily.
The use of these needles should be limited to ob-taining blood specimens or
administering bolus injections or in-fusions lasting only a few hours, as they
increase the risk for vein injury and infiltration. Insertion of an
over-the-needle catheter requires the additional step of advancing the catheter
into the vein after venipuncture. Because these devices are less likely to
cause infiltration, they are frequently preferred over winged in-fusion sets.
Plastic cannulas
inserted through a hollow needle are usually called intracatheters. They are
available in long lengths and are well suited for placement in central
locations. Because insertion requires threading the cannula through the vein
for a relatively long distance, these can be difficult to insert. The most
com-monly used infusion device is the over-the-needle catheter. A hol-low metal
stylet is preinserted into the catheter and extends through the distal tip of
the catheter to allow puncture of the ves-sel, in an effort to guide the
catheter as the venipuncture is per-formed. The vein is punctured and a
flashback of blood appears in the closed chamber behind the catheter hub. The
catheter is threaded through the stylet into the vein and the stylet is then
re-moved. There are many safety over-the-needle catheter designs available with
retracting stylets to protect health care workers from needlestick injuries.
Many types of cannulas are available for IV therapy. Some of the
variations in these cannulas include the thickness of the cannula wall (affects
rate of flow), the sharpness of the insertion needles (determines needle
insertion technique), the softening properties of the cannula (influences the
length of time the can-nula can remain in place), safety features (minimizes
risk of needlestick injuries and blood-borne exposure), and the number of
lumens (determines the number of solutions that can be infused simultaneously).
Cannula systems that help prevent needlesticks and transmission of blood-borne
diseases are discussed below. Most standard peripheral catheters are composed
of some form of plastic. Teflon (polytetrafluoroethylene)ŌĆōcoated catheters have
less thrombogenic properties and are less inflammatory than polyurethane or
PVC. Catheter size for steel needles can range from 3Ōüä8 to 1.5 inches in length and 27 to 13 gauge. Plastic catheters range in
length from 5Ōüä8 to 2 inches or as long as 12 inches. The
size of the catheter ranges from 27 to 12 gauge.
To select the ideal product for use, consideration should be given to
which product provides the greatest patient satisfaction and offers quality,
cost-effective infusion care. All devices should be radiopaque to determine
catheter location by x-ray, if indicated. All catheters are thrombogenic and
differ only in their degree of thrombus occurrence. Biocompatibility, another
characteristic of a catheter, ensures that inflammation and irritation do not
occur. Silicone catheters are the most bioinert catheter available today.
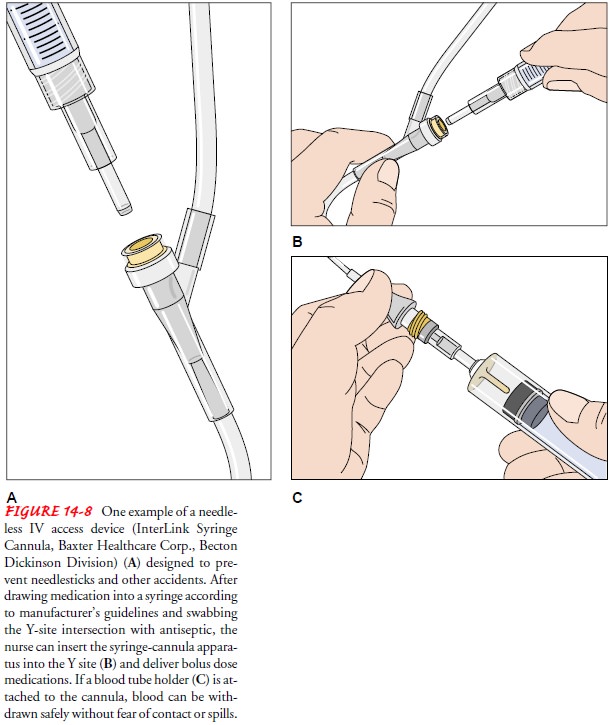
Needleless IV Delivery Systems.
In an effort to decrease needle-stick injuries and exposure to HIV,
hepatitis, and other blood-borne pathogens, agencies have implemented
needleless IV delivery systems. These systems have built-in protection against
needle-stick injuries and provide a safe means of using and disposing of an IV
administration set (which consists of tubing, an area for in-serting the tubing
into the container of IV fluid, and an adapter for connecting the tubing to the
needle). Numerous companies produce needleless components. IV line connectors
allow the si-multaneous infusion of IV medications and other intermittent
medications (known as a piggyback delivery) without the use of needles (Fig.
14-8). Technology is advancing and moving away from use of the traditional
stylet. An example is a self-sheathing stylet that is recessed into a rigid
chamber at the hub of the catheter when its insertion is complete. Other
designs have placed the stylet at the end of a flexible wire to avoid
needlesticks.
Many examples of these devices are on the market. Each insti-tution must
evaluate products to determine its own needs based on OSHA guidelines and the
institutionŌĆÖs policies and procedures.
Peripherally Inserted Central Catheter or Midline Catheter Access Lines.
Patients who need moderate- to long-termparenteral therapy often receive a peripherally inserted central catheter or a midline catheter. These catheters are also used for
patients with limited peripheral access (eg, obese or emaciated patients,
IV/injection drug users) who require IV antibiotics, blood, and parenteral
nutrition. For these devices to be used, the median cephalic, basilic, and
cephalic veins must be pliable (not sclerosed or hardened) and not subject to
repeated puncture. If these veins are damaged, then central venous access via
the sub-clavian or internal jugular vein, or surgical placement of an
im-planted port or a vascular access device, must be considered as an
alternative. Table 14-9 compares peripherally inserted central and midline
catheter lines.
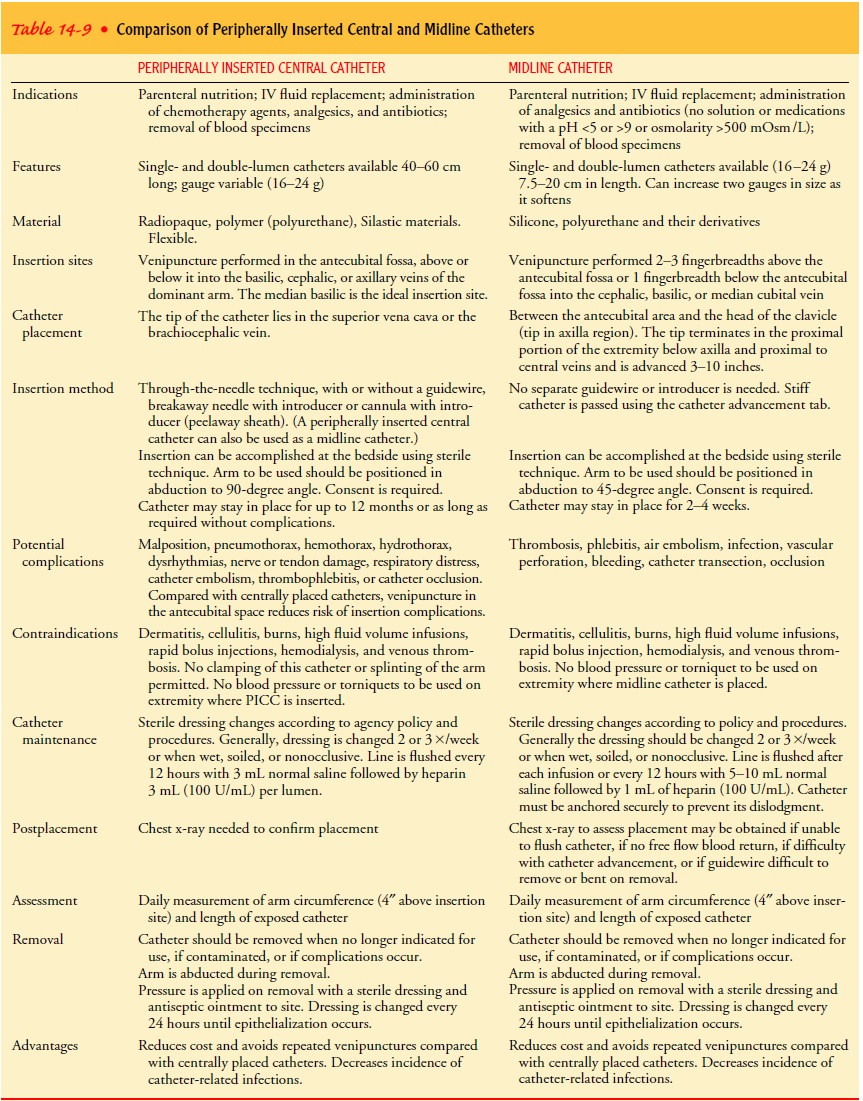
The principles for
inserting these lines are much the same as those for inserting peripheral
catheters; however, their insertion should be undertaken only by those who are
experienced and spe-cially skilled in inserting IV lines.
The physician prescribes
the line and the solution to be in-fused. Insertion of either line requires
sterile technique. The size of the catheter lumen chosen is based on the type
of solution, the size of the patient, and the vein to be used. The patientŌĆÖs
consent is obtained before use of these catheters. Use of the dominant arm is
recommended as the site for inserting the can-nula into the superior vena cava
to ensure adequate arm move-ment, which encourages blood flow and reduces the
risk of dependent edema.
TEACHING THE PATIENT
Except in emergency situations, a patient should be prepared in advance
for an IV infusion. The venipuncture, the expected length of infusion, and
activity restrictions are explained. Then the pa-tient should have an
opportunity to ask questions and voice con-cerns. For example, some patients
believe they will die if small bubbles in the tubing enter their veins. After
acknowledging this fear, the nurse can explain that usually only relatively
large vol-umes of air administered rapidly are dangerous.
PREPARING THE IV SITE
Before preparing the
skin, the nurse should ask the patient if he or she is allergic to latex or
iodine, products commonly used in preparing for IV therapy. Excessive hair at
the selected site may be removed by clipping to increase the visibility of the
veins and to facilitate insertion of the cannula and adherence of dressings to
the IV insertion site. Because infection can be a major com-plication of IV
therapy, the IV device, the fluid, the container, and the tubing must be
sterile. The insertion site is scrubbed with a sterile pad soaked in 10%
povidoneŌĆōiodine (Betadine) or chlorhexidine gluconate solution for 2 to 3
minutes, working from the center of the area to the periphery and allowing the
area to air day. The site should not be wiped with 70% alcohol be-cause the
alcohol negates the effect of the disinfecting solution. (Alcohol pledgets are
used for 30 seconds instead, only if the pa-tient is allergic to iodine.) The
nurse must perform hand hygiene and put on gloves. Nonsterile disposable gloves
must be worn during the venipuncture procedure because of the likelihood of
coming into contact with the patientŌĆÖs blood.
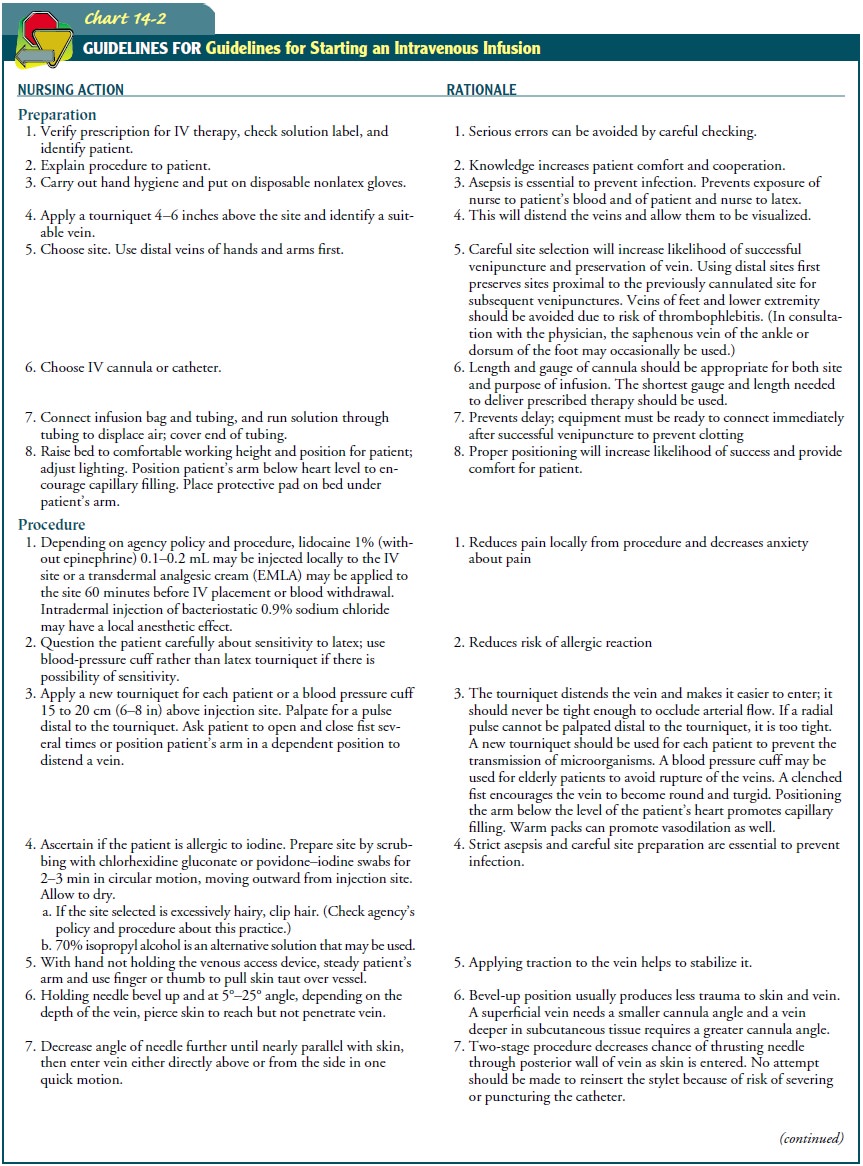
PERFORMING VENIPUNCTURE
Guidelines and a suggested sequence for venipuncture are pre-sented in
Chart 14-2. For veins that are very small or particularly fragile,
modifications in the technique may be necessary. Alter-native methods can be
found in journal articles or in specialized textbooks of IV therapy.
Institutional policies and procedures determine whether all nurses must be certified
to perform venipuncture.
A nurse certified in IV therapy or an IV team can be consulted to assist with
initiating IV therapy.
MAINTAINING THERAPY
Maintaining an existing IV infusion is a nursing responsibility that
demands knowledge of the solutions being administered and the principles of
flow. In addition, patients must be assessed care-fully for both local and
systemic complications.
FACTORS AFFECTING FLOW
The flow of an IV
infusion is governed by the same principles that govern fluid movement in
general.
ŌĆó
Flow is directly proportional to the height of the
liquid col-umn. Raising the height of the infusion container may im-prove a
sluggish flow.
ŌĆó
Flow is directly proportional to the diameter of
the tubing. The clamp on IV tubing regulates the flow by changing the tubing
diameter. In addition, the flow is faster through large-gauge rather than
small-gauge cannulas.
ŌĆó
Flow is inversely proportional to the length of the
tubing. Adding extension tubing to an IV line will decrease the flow.
ŌĆó
Flow is inversely proportional to the viscosity of
a fluid. Vis-cous IV solutions, such as blood, require a larger cannula than do
water or saline solutions.
MONITORING FLOW
Because so many factors influence gravity flow, a solution does not
necessarily continue to run at the speed originally set. There-fore, the nurse
monitors IV infusions frequently to make sure that the fluid is flowing at the
intended rate. The IV container should be marked with tape to indicate at a
glance whether the correct amount has infused. The flow rate is calculated when
the solu-tion is originally started, then monitored at least hourly. To
cal-culate the flow rate, the nurse determines the number of drops delivered
per milliliter; this varies with equipment and is usually printed on the administration
set packaging. A formula that can be used to calculate the drop rate is:
gtt/mL of infusion
set/60 (min in hr) ├Ś total hourly vol = gtt/min
Flushing of a vascular device is performed to ensure patency and prevent
the mixing of incompatible medications or solutions. This procedure should be
carried out at established intervals, ac-cording to hospital policy and
procedure, especially for intermit-tently used catheters. Most manufacturers
and researchers (LeDuc, 1997) suggest the use of saline for flushing. The
volume of the flush solution should be equal to at least twice the volume
capacity of the catheter. The catheter should be clamped before the syringe is
completely empty and withdrawn to prevent reflux of blood into the lumen, which
could cause catheter clotting.
A variety of electronic infusion devices are available to assist in IV
fluid delivery. These devices allow more accurate administration of fluids and
medications than is possible with routine gravity-flow setups. A pump is a
positive-pressure device that uses pressure to infuse fluid at a pressure of 10
psi. Newer models use a pressure of 5 psi. The pressure exerted by the pump
overrides vascular resis-tance (increased tubing length, low height of the IV
container).
Volumetric pumps calculate the volume delivered by measur-ing the volume in a reservoir that is part of the set and calibrated in mL/h. A controller is an infusion assist device that relies on gravity for infusion; the volume is calibrated in drops/min.
A controller uses a drop sensor to monitor the flow. Factors essential for the safe
use of pumps include alarms to signify the presence of air in the IV line and
occlusion. The standard for the accurate delivery of fluid or medication via an
electronic IV infusion pump is plus or minus 5%. The manufacturerŌĆÖs directions
must be read care-fully before using any infusion pump or controller, because
there are many variations in available models. Use of these devices does not
eliminate the need for the nurse to monitor the infusion and the patient
frequently.
DISCONTINUING AN INFUSION
The removal of an IV
catheter is associated with two possible dan-gers: bleeding and catheter
embolism. To prevent excessive bleed-ing, a dry, sterile pressure dressing
should be held over the site as the catheter is removed. Firm pressure is
applied until hemostasis occurs.
If a plastic IV catheter is severed, the loose fragment can travel to
the right ventricle and block blood flow. To detect this complication when the
catheter is removed, the nurse compares the expected length of the catheter
with its actual length. Plastic cathe-ters should be withdrawn carefully and
their length measured to make certain that no fragment has broken off.
Great care must be exercised when using scissors around the dressing
site. If the catheter clearly has been severed, the nurse can attempt to
occlude the vein above the site by applying a tourni-quet to prevent the
catheter from entering the central circulation (until surgical removal is
possible). As always, however, it is better to prevent a potentially fatal
problem than to deal with it after it has occurred. Fortunately, catheter
embolism can be prevented easily by following simple rules:
ŌĆó
Avoid using scissors near the catheter.
ŌĆó
Avoid withdrawing the catheter through the
insertion needle.
ŌĆó
Follow the manufacturerŌĆÖs guidelines carefully (eg,
cover the needle point with the bevel shield to prevent severance of the
catheter).
MANAGING SYSTEMIC COMPLICATIONS
IV therapy predisposes
the patient to numerous hazards, includ-ing both local and systemic
complications. Systemic complica-tions occur less frequently but are usually
more serious than local complications. They include circulatory overload, air
embolism, febrile reaction, and infection.
Fluid Overload.
Overloading
the circulatory system with excessiveIV fluids causes increased blood pressure
and central venous pres-sure. Signs and symptoms of fluid overload include
moist crack-les on auscultation of the lungs, edema, weight gain, dyspnea, and
respirations that are shallow and have an increased rate. Possible causes
include rapid infusion of an IV solution or hepatic, cardiac, or renal disease.
The risk for fluid overload and subsequent pul-monary edema is especially
increased in elderly patients with car-diac disease; this is referred to as
circulatory overload.
The treatment for
circulatory overload is decreasing the IV rate, monitoring vital signs
frequently, assessing breath sounds, and placing the patient in a high FowlerŌĆÖs
position. The physician is contacted immediately. This complication can be
avoided by using an infusion pump for infusions and by carefully monitoring all
infusions. Complications of circulatory overload include heart failure and
pulmonary edema.
Air Embolism.
The
risk of air embolism is rare but ever-present.It is most often associated with
cannulation of central veins. Man-ifestations of air embolism include dyspnea
and cyanosis; hypo-tension; weak, rapid pulse; loss of consciousness; and
chest, shoulder, and low back pain. Treatment calls for immediately clamping
the cannula, placing the patient on the left side in the Trendelenburg
position, assessing vital signs and breath sounds, and administering oxygen.
Air embolism can be prevented by using a Luer-Lok adapter on all lines, filling
all tubing completely with solution, and using an air detection alarm on an IV
pump. Complications of air embolism include shock and death. The amount of air
necessary to induce death in humans is not known; however, the rate of entry is
probably as important as the actual volume of air.
Septicemia and Other Infection.
Pyrogenic substances in eitherthe infusion solution or the IV
administration set can induce a febrile reaction and septicemia. Signs and
symptoms include an abrupt temperature elevation shortly after the infusion is
started, backache, headache, increased pulse and respiratory rate, nausea and
vomiting, diarrhea, chills and shaking, and general malaise. In severe
septicemia, vascular collapse and septic shock may occur. Causes of septicemia
include contamination of the IV product or a break in aseptic technique,
especially in immunocompromised patients. Treatment is symptomatic and includes
culturing of the IV cannula, tubing, or solution if suspect and establishing a
new IV site for medication or fluid administration.
Related Topics