Chapter: Medical Surgical Nursing: Fluid and Electrolytes: Balance and Distribution
Fluid Volume Deficit (Hypovolemia)
Fluid Volume Disturbances
FLUID
VOLUME DEFICIT (HYPOVOLEMIA)
Fluid volume deficit (FVD) occurs when loss of extracellular fluid
volume exceeds the intake of fluid. It occurs when water and elec-trolytes are
lost in the same proportion as they exist in normal body fluids, so that the
ratio of serum electrolytes to water re-mains the same. Fluid volume deficit
(hypovolemia) should not be confused with the term dehydration, which refers to loss of water alone with increased
serum sodium levels. FVD may occur alone or in combination with other
imbalances. Unless other im-balances are present concurrently, serum
electrolyte concentra-tions remain essentially unchanged.
Pathophysiology
FVD results from loss of body fluids and occurs more rapidly when
coupled with decreased fluid intake. FVD can develop from inadequate intake
alone if the decreased intake is prolonged. Causes of FVD include abnormal
fluid losses, such as those re-sulting from vomiting, diarrhea, GI suctioning,
and sweating, and decreased intake, as in nausea or inability to gain access to
fluids (Beck, 2000).
Additional risk factors
include diabetes insipidus, adrenal in-sufficiency, osmotic diuresis,
hemorrhage, and coma. Third-space fluid shifts, or the movement of fluid from
the vascular system to other body spaces (eg, with edema formation in burns or
ascites with liver dysfunction), also produce FVD.
Clinical Manifestations
FVD can develop rapidly
and can be mild, moderate, or severe, depending on the degree of fluid loss.
Important characteristics of FVD include acute weight loss; decreased skin
turgor; oliguria; concentrated urine; postural hypotension; a weak, rapid heart
rate; flattened neck veins; increased temperature; decreased cen-tral venous
pressure; cool, clammy skin related to peripheral vaso-constriction; thirst;
anorexia; nausea; lassitude; muscle weakness; and cramps.
Assessment and Diagnostic Findings
Laboratory data useful in evaluating fluid volume status include BUN and
its relation to the serum creatinine concentration. A volume-depleted patient
has a BUN elevated out of proportion to the serum creatinine level (a ratio
greater than 20:1). The cause of hypovolemia may be determined through the
health history and physical examination. The BUN can be elevated due to
de-hydration or decreased renal perfusion and function. Also, thehematocrit
level is greater than normal because the red blood cells become suspended in a
decreased plasma volume.
Serum electrolyte changes
may also exist. Potassium and sodium levels can be reduced (hypokalemia,
hyponatremia) or elevated (hyperkalemia, hypernatremia).
•
Hypokalemia occurs with GI and renal losses.
•
Hyperkalemia occurs with adrenal insufficiency.
•
Hyponatremia occurs with increased thirst and ADH
release.
•
Hypernatremia results from increased insensible
losses and diabetes insipidus.
Urine specific gravity is increased in relation to the kidneys’ attempt
to conserve water and decreased with diabetes insipidus. Urine osmolality is
greater than 450 mOsm/Kg, since the kidneys try to compensate by conserving
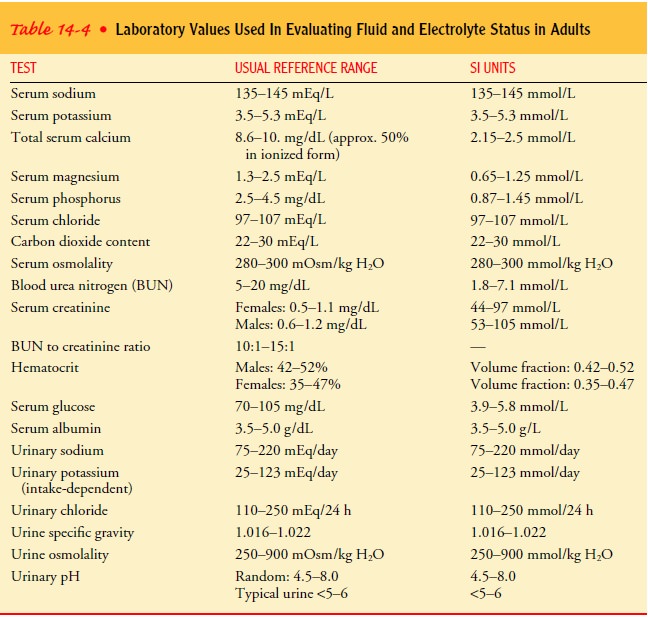
water. Normal values for these tests are listed in Table 14-4.
Gerontologic Considerations
Elderly patients have special nursing care needs because of their
propensity for developing fluid and electrolyte imbalances (Beck, 2000; Kugler
& Hustead, 2000). Fluid balance in the elderly patient is often marginal at
best because of certain physiologic changes associated with the aging process.
Some of these changes include reduction in total body water (associated with
increased body fat content and decreased muscle mass); reduction in renal
function, resulting in decreased ability to concentrate urine; decreased
cardiovascular and respiratory function; and disturbances in hormonal
regulatory functions. Although these changes are viewed as normal in the aging
process, they must be considered when the elderly person becomes ill because
age-related changes predispose the person to fluid and electrolyte imbalances.
These physiologic changes must be considered during assessment of the elderly
patient as well as before initiating treatment for fluid and electrolyte
imbalances.
Assessment of the
elderly patient should be modified some-what from that of younger adults. For
example, skin turgor is less valid in the assessment of elderly patients
because their skin has lost some of its elasticity; therefore, other assessment
measures (eg, slowness in filling of veins of the hands and feet) become more
important in detecting FVD. In the elderly patient, skin turgor is best tested
over the forehead or the sternum, because al-terations in skin elasticity are
less marked in these areas. As in any patient, skin turgor should be monitored
serially to detect subtle changes.
The nurse should perform a functional assessment of the aged person’s ability to determine fluid and food needs and to obtain adequate intake. For example, is the patient mentally clear? Is the patient able to ambulate and use both arms and hands to reach fluids and foods? Is the patient able to swallow? All of these ques-tions have a direct bearing on how patients will be able to meet their own need for fluids and foods. During an elderly patient’s hospital stay, the nurse must provide fluids for any patient who is unable to carry out self-care activities.
Another concern is that
some elderly patients deliberately re-strict their fluid intake to avoid
embarrassing episodes of incon-tinence. In this situation, the nurse also
identifies interventions to deal with the incontinence, such as encouraging the
patient to wear protective clothing or devices, carry a urinal in the car, or
pace fluid intake to allow access to toilet facilities during the day. Elderly
people without cardiovascular or renal dysfunction should be reminded to drink
adequate fluids.
Medical Management
When planning the correction of fluid loss for the patient with FVD, the
health care provider considers the usual maintenance requirements of the
patient and other factors (such as fever) that can influence fluid needs. When
the deficit is not severe, the oral route is preferred, provided the patient
can drink. When fluid losses are acute or severe, however, the IV route is
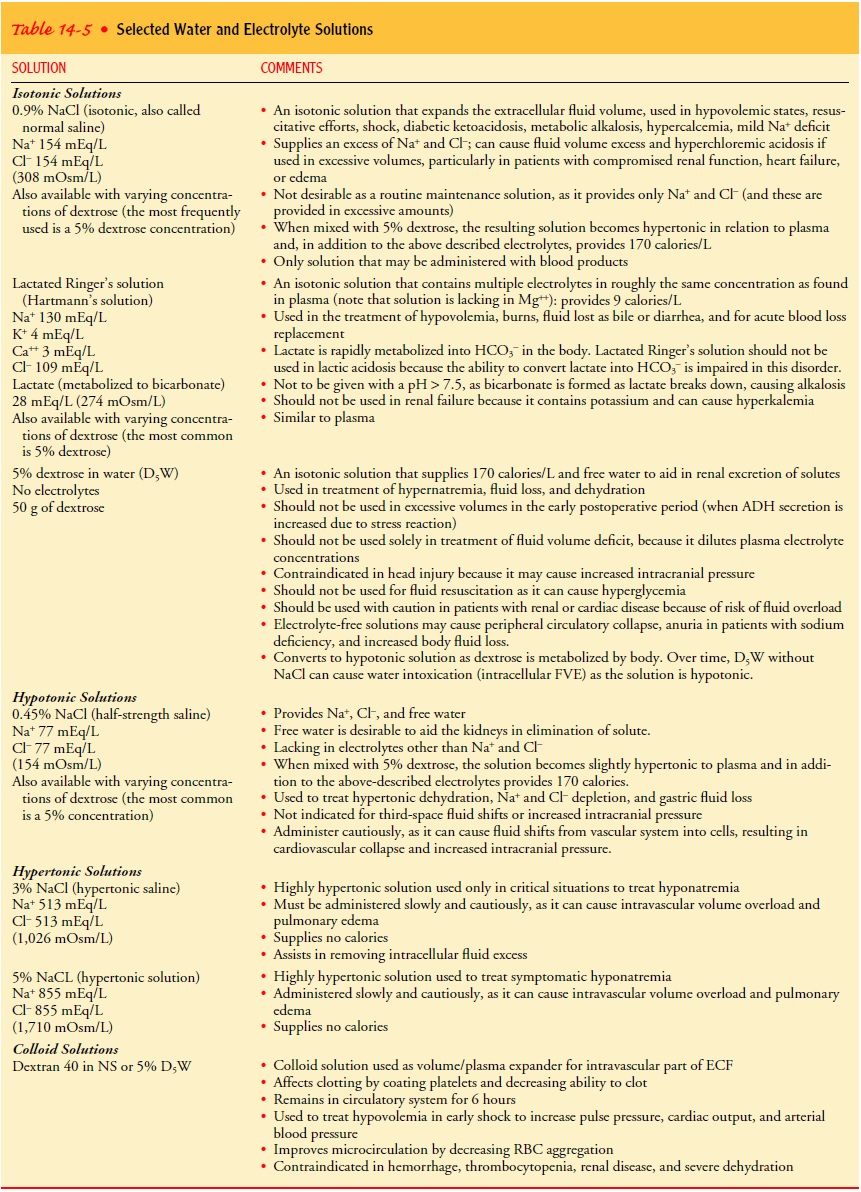
required. Iso-tonic electrolyte solutions (eg, lactated Ringer’s or 0.9% sodium
chloride) are frequently used to treat the hypotensive patient with FVD because
they expand plasma volume. As soon as the patient becomes normotensive, a
hypotonic electrolyte solution (eg, 0.45% sodium chloride) is often used to
provide both electrolytes and water for renal excretion of metabolic wastes.
These and additio-nal fluids are listed in Table 14-5.
Accurate and frequent assessments of intake and output, weight, vital
signs, central venous pressure, level of consciousness, breath sounds, and skin
color should be performed to determine when therapy should be slowed to avoid
volume overload. The rate of fluid administration is based on the severity of
loss and the pa-tient’s hemodynamic response to volume replacement.
If the patient with severe FVD is not excreting enough urine and is
therefore oliguric, the health care provider needs to deter-mine whether the
depressed renal function is the result of reduced renal blood flow secondary to
FVD (prerenal azotemia) or, more seriously, to acute tubular necrosis from
prolonged FVD. The test used in this situation is referred to as a fluid
challenge test. During a fluid challenge test, volumes of fluid are
administered at specific rates and intervals while the patient’s hemodynamic
response to this treatment is monitored (ie, vital signs, breath sounds,
sensorium, central venous pressure, urine output).
A typical example of a
fluid challenge involves administering 100 to 200 mL of normal saline solution
over 15 minutes. The goal is to provide fluids rapidly enough to attain
adequate tissue perfu-sion without compromising the cardiovascular system. The
re-sponse by a patient with FVD but normal renal function will be increased
urine output and an increase in blood pressure and cen-tral venous pressure.
Shock can occur when the volume of fluid lost exceeds 25% of the
intravascular volume, or when fluid loss is rapid.
Nursing Management
To assess for FVD, the nurse monitors and measures fluid intake and
output at least every 8 hours, and sometimes hourly. As FVD develops, body
fluid losses exceed fluid intake. This loss may be in the form of excessive
urination (polyuria), diarrhea, vomiting, and so on. Later, after FVD fully
develops, the kidneys attempt to con-serve needed body fluids, leading to a urine
output of less than 30 mL/h in an adult. Urine in this instance is concentrated
and rep-resents a healthy renal response. Daily body weights are monitored; an
acute loss of 0.5 kg (1 lb) represents a fluid loss of approximately 500 mL. (One liter of fluid
weighs approximately 1 kg, or 2.2 lb.)
Vital signs are closely monitored. The nurse observes for a weak, rapid
pulse and postural hypotension (ie, a drop in systolic pressure exceeding 15 mm
Hg when the patient moves from a lying to a sitting position). A decrease in
body temperature often accompanies FVD, unless there is a concurrent infection.
Skin and tongue turgor
is monitored on a regular basis. In a healthy person, pinched skin immediately
returns to its normal position when released. This elastic property, referred
to as tur-gor, is partially dependent on interstitial fluid volume. In a
per-son with FVD, the skin flattens more slowly after the pinch is released.
When FVD is severe, the skin may remain elevated for many seconds. Tissue
turgor is best measured by pinching the skin over the sternum, inner aspects of
the thighs, or forehead.
Evaluating tongue
turgor, which is not affected by age, may be more valid than evaluating skin
turgor. In a normal person, the tongue has one longitudinal furrow. In the
person with FVD, there are additional longitudinal furrows and the tongue is
smaller, because of fluid loss. The degree of oral mucous membrane moisture is
also assessed; a dry mouth may indicate either FVD or mouth breathing.
Urinary concentration is
monitored by measuring the urine specific gravity. In a volume-depleted
patient, the urinary specific gravity should be above 1.020, indicating healthy
renal conser-vation of fluid.
Mental function is
eventually affected in severe FVD as a re-sult of decreasing cerebral
perfusion. Decreased peripheral perfu-sion can result in cold extremities. In
patients with relatively normal cardiopulmonary function, a low central venous
pressure is indicative of hypovolemia. Patients with acute cardiopulmonary decompensation
require more extensive hemodynamic monitor-ing of pressures in both sides of
the heart to determine if hypo-volemia exists.
PREVENTING FVD
To prevent FVD, the
nurse identifies patients at risk and takes measures to minimize fluid losses.
For example, if the patient has diarrhea, diarrhea control measures should be
implemented and replacement fluids administered. These measures may include
ad-ministering antidiarrheal medications and small volumes of oral fluids at
frequent intervals.
CORRECTING FVD
When possible, oral
fluids are administered to help correct FVD, with consideration given to the
patient’s likes and dislikes. Also, the type of fluid the patient has lost is
considered, and attempts are made to select fluids most likely to replace the
lost electrolytes. If the patient is reluctant to drink because of oral
discomfort, the nurse assists with frequent mouth care and provides
nonirritating fluids. The patient may be offered small volumes of fluids at
fre-quent intervals rather than a large volume all at once. If nausea is
present, antiemetics may be needed before oral fluid replacement can be
tolerated.
If the patient cannot eat and drink, the nurse may need to ad-minister fluid by an alternative route (enteral or parenteral) pre-scribed to prevent renal damage related to prolonged FVD.
Related Topics