Chapter: Medical Surgical Nursing: Fluid and Electrolytes: Balance and Distribution
Laboratory Tests for Evaluating Fluid Status
LABORATORY
TESTS FOR EVALUATING FLUID STATUS
Osmolality reflects the concentration of fluid that affects themovement of water between fluid compartments by osmosis. Osmolality measures the solute concentration per kilogram in blood and urine.
It is also a measure of a solution’s ability to create osmotic pressure and
affect the movement of water. Serum os-molality primarily reflects the
concentration of sodium. Urine osmolality is determined by urea, creatinine,
and uric acid. When measured with serum osmolality, urine osmolality is the
most re-liable indicator of urine concentration. Osmolality is reported as
milliosmoles per kilogram of water (mOsm/kg).
Osmolarity, another term that describes the concentration ofsolutions, is measured
in milliosmoles per liter (mOsm/L). The term “osmolality,” however, is used
more often in clinical practice. Normal serum osmolality is 280 to 300 mOsm/kg,
and normal urine osmolality is 250 to 900 mOsm/kg. Sodium predominates in ECF
osmolality and holds water in this compartment.
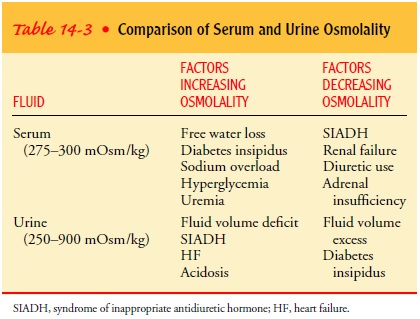
Factors that increase
and decrease serum and urine osmolality are identified in Table 14-3. Serum
osmolality may be measured directly through laboratory tests or estimated at
the bedside by doubling the serum sodium level or by using the following
formula:

The calculated value
usually is within 10 mOsm of the mea-sured osmolality.
Urine specific gravity measures the kidneys’ ability to excrete or conserve water. The specific gravity of urine is compared to the weight of distilled water, which has a specific gravity of 1.000. The normal range of specific gravity is 1.010 to 1.025. Urine spe-cific gravity can be measured at the bedside by placing a calibrated hydrometer or urinometer in a cylinder of approximately 20 mL of urine.
Specific gravity can also be assessed with a refractometer or dipstick with a
reagent for this purpose. Specific gravity varies inversely with urine volume;
normally, the larger the volume of urine, the lower the specific gravity.
Specific gravity is a less reli-able indicator of concentration than urine
osmolality; increased glucose or protein in urine can cause a falsely high
specific grav-ity. Factors that increase or decrease urine osmolality are the
same for urine specific gravity.
Blood urea nitrogen (BUN) is made up of urea, an end prod-uct of
metabolism of protein (from both muscle and dietary in-take) by the liver.
Amino acid breakdown produces large amounts of ammonia molecules, which are absorbed
into the bloodstream. Ammonia molecules are converted to urea and excreted in
the urine. The normal BUN is 10 to 20 mg/dL (3.5–7 mmol/L). The BUN level
varies with urine output. Factors that increase BUN include decreased renal
function, GI bleeding, dehydra-tion, increased protein intake, fever, and
sepsis. Those that de-crease BUN include end-stage liver disease, a low-protein
diet, starvation, and any condition that results in expanded fluid vol-ume (eg,
pregnancy).
Creatinine is the end product of muscle metabolism. It is a bet-ter
indicator of renal function than BUN because it does not vary with protein
intake and metabolic state. The normal serum crea-tinine is approximately 0.7
to 1.5 mg/dL (SI: 60–130 mmol/L); however, its concentration depends on lean
body mass and varies from person to person. Serum creatinine levels increase
when renal function decreases.
Hematocrit measures the volume percentage of red blood cells
(erythrocytes) in whole blood and normally ranges from 44% to 52% for males and
39% to 47% for females. Conditions that in-crease the hematocrit value are
dehydration and polycythemia; those that decrease hematocrit are overhydration
and anemia.
Urine sodium values
change with sodium intake and the status of fluid volume (as sodium intake
increases, excretion increases; as the circulating fluid volume decreases,
sodium is conserved). Normal urine sodium levels range from 50 to 220 mEq/24 h
(50–220 mmol/24 h). A random specimen usually contains more than 40 mEq/L of
sodium. Urine sodium levels are used to assess volume status and are useful in
the diagnosis of hyponatremia and acute renal failure.
Related Topics