Chapter: Medicine Study Notes : Reproductive and Obstetrics
Sexually Transmitted Diseases (STDs)
Sexually Transmitted Diseases (STDs)
· Types and incubation:
o Chlamydia (7 –21 days) Þ don‟t test till 14 days after contact (unless symptomatic)
o Gonorrhoea (range 1 – 14 days, commonly 2 – 5 days)
o Trichomonas (3 – 21 days)
o Herpes Simplex Virus (2 days onwards – maybe years)
o Human Papilloma Virus (2 – 4 months, up to a year, vertical transmission possible)
o Human Immunodeficiency Virus (HIV) – (seroconversion illness 2 – 6 weeks after exposure, HIV antibodies almost always present after 3 months. Mean time to developing AIDS defining illness 9 – 12 years)
o Hepatitis B (1 – 6 months)
o Syphilis (9 – 90 days)
o Non-specific urethritis
o Pubic Lice (eggs – 2 weeks to mature, larvae – 1 week to mature)
o Scabies (3 – 30 days, 6 weeks for itch to develop)
o Hepatitis C and A may be sexually transmitted
·
Not necessarily sexually
transmitted:
o Normal anatomical variants
o Commensals ® bacterial vaginosis
o Dermatoses
o Candidacies (commensals)
o Molluscum contagiousum (3 weeks – months)
o Urinary tract infections
o Prostatitis
o Vulval disorders
Tests for STD’s
·
Urethral swab or first pass urine
for chlamydia
·
Anal or throat swab for
gonorrhoea if appropriate
·
Female:
o Cervical sample for gonorrhoea, chlamydia (endocervical cells needed)
o Cervical smear
o High vaginal swab for bacterial vaginosis, candida, trichomonas
·
Male: Urethral swab for
gonorrhoea
·
Blood tests:
o Hepatitis B (Ag and Ab) and C (Ab)
o Syphilis: VDRL, TPHA
o HIV Ab if appropriate with counselling and consent. Always attend for results
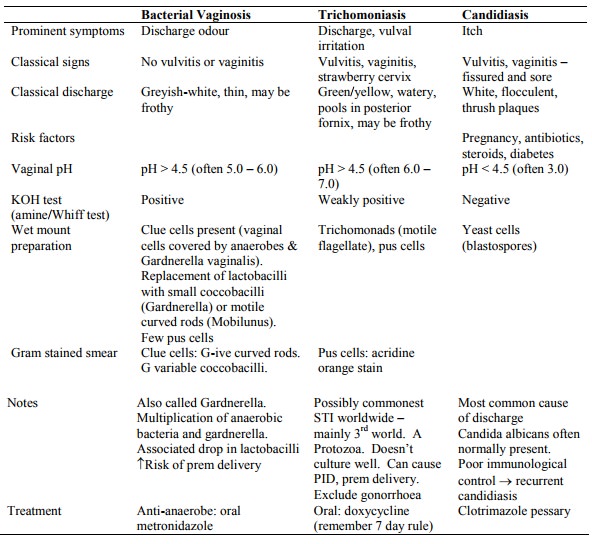
Vaginal Discharge
·
Cervical secretions in women not
on the pill, and which change during the cycle, are part of normal discharge.
Mucus is clear or clear/white. Some inflammatory cells are normal in the latter
half of a cycle
·
Desquamating vaginal cells with
healthy lactobacilli are major part of normal discharge – pH < 4.5
·
Key history questions:
o Colour
o Odour
o Itch
·
Differential:
o Thrush (Candidiasis): white curds, very itchy, not smelly
o Trichomoniasis: grey/green discharge, fishy smell, moderate itch
o Bacterial Vaginosis: green, fishy, itchy
o Chlamydia: asymptomatic or discharge
o Atrophic vaginitis: brown, spotty discharge (from bruising), pain, no
itch. Treatment: oestrogen cream or HRT
Neisseria Gonorrhoeae
·
Description: G –ive diplococci
·
Symptoms:
o Male: 80% symptomatic. Discharge & dysuria (razor blade pain). 30% also have chlamydia
o Female: only 20% symptomatic – can have vaginal discharge or pelvic pain. Pick up with opportunistic/selective screening if under 25, multiple partners, changed partner in last 6 months, IUCD, etc
o Rectal and pharyngeal: often asymptomatic
·
Diagnosis: gram stain microscopy
if symptomatic or contact, or culture on chocolate agar
·
Advice: no sex until minimum of 3
days since treatment completed
· Treatment:
o Amoxycillin 3 gm and Probenecid 1 gm stat (not longer standard due to penicillin resistant), or
o Ciprofloxacin 500 mgs (a quinolone) stat if penicillin allergy or if resistant. Specialist endorsement required. If resistant to that then Ceftriaxone (common in Auckland).
o Azithromycin will cover gonorrhoea if it is being used to treat
concurrent chlamydia
o Resistance possible
·
Contact tracing required. Treat
partners
·
Test for cure at 14 days (legal
requirement)
· Complications: See Topic: Pelvic Inflammatory Disease (PID)
Chlamydia Trachomatis
·
Description: obligate
intracellular bacteria, STIs are types D – K.
Highest in 20 – 24 year age group
·
Symptoms:
o Urethritis, unexplained cystitis, mucopurulent cervicitis, pelvic pain, irregular bleeding
o 80% of females and 50% of males have no symptoms. Suspect and test if
sexual contacts have it, if patients asks for STI tests, patients under 25 with
new/multiple partners
o Up to 30% associated with concurrent N Gonorrhoea infection
· Diagnosis:
o Female: swab from affected area, including from endocervix. Rotate 6 –
10 times. Urine test alone not sufficient. Most common site of single infection
is cervix (ie urine is clear)
o Male: urine test
o New PCR test easier sampling (urine test)
o Opportunistic detection has been shown to reduce rates of PID and
ectopic pregnancy
·
Advice:
o Abstain until treated – if not use condoms
o Contact trace
·
Treatment:
o Without test results: Doxycycline 100mgs bd for 7 days (remember 7 day
rule for patients on OC)
o Known positive and partners: Azithromycin 1 g stat orally – directly observed treatment
o In pregnancy: erythromycin ethylsuccinate 800mg qid for 7 days – must be treated to prevent amnionitis and premature rupture of membranes
o In PID: Doxycycline/erythromycin for 14 days and ornidazole 500 mgs bd for 7 days, plus consider gonorrhoea in which case penicillin/ciprofloxacin in addition
o Test of cure in 3 weeks if non-compliance or re-infection suspected. Urine test is adequate for males and females
o Test high risk patients only for cure
o If reinfection, then ?untreated partner
·
Complications:
o Neonatal: conjunctivitis, pneumonitis 2 – 4 weeks later
o See Topic: Pelvic Inflammatory Disease (PID)
Herpes Simplex Virus (Type 2)
· Manifestations: systemic (fever, sore throat), gingivostomatitis (ulcers with yellow slough – cold sores), meningitis (uncommon, self-limiting), encephalitis (fever, fits, headache, dysphagia, hemiparesis – do PCR on CSF sample – refer urgently)
·
Incubation: 2 – 25 days. Chronic
infection is due to the virus remaining in the sensory nerve ganglia.
Infectious period indeterminate ® contact isolation
·
Symptoms:
o Blisters which become shallow painful ulcers, often preceded by itching
or tingling
o First episode may be accompanied by flu like illness, tender inguinal nodes and dysuria
o Recurrences can be brought on by stress, fatigue, depression, immunosuppression and concurrent illness. Recurrences usually less severe and become less frequent
·
Diagnosis: clinical suspicion.
Swab the base of an unroofed ulcer and refrigerate in viral medium. This will
be painful. Culture negative doesn‟t exclude HSV as timing and collection
technique important.
·
Serology possible, but not
routinely used
· Pathogenesis. There are two antigenic types of Herpes Simplex Virus:
o Type 1 is associated with lesions on the face and fingers, and sometimes genital lesions. Treat with zovirax (topical cream). Prevalence: 70% of population
o Type 2 is associated almost entirely with genital infections, and affects the genitalia, vagina, and cervix and may predispose to cervical dysplasia. 10% of oral lesions caused by type 2. Prevalence: 10 – 15% of population (depends on population – more in high risk)
Pelvic Inflammatory Disease (PID)
·
~ Tubulo-peritoneal Disease
·
Cause: ascending infection of
vagina and cervix to endometrium, fallopian tubes and other structures:
o Chlamydia – often chronic
o Gonorrhoea – often acute
o Can also be anaerobes (e.g. after instrumentation of the uterus or long
standing PID)
·
Symptoms: Acute pain, but 30%
asymptomatic, dyspareunia (pain on sex)
·
Risk factors:
o Young age (< 25)
o Sexual
activity, multiple partners, multiple infections
o Postpartum infections
o IUCDs in first several weeks after insertion
o Decreased rates with condoms, diaphragms, spermicides (bacteria can use sperm as vector), tubal ligation, OC pill
·
Diagnosis:
o Difficult to make clinically: there are multiple causes of abdominal
pain
o Cervical motion tenderness (also occurs with ectopic pregnancy)
o Purulent cervical/vaginal discharge
o Oral temperature > 38 C
o Irregular bleeding and break through bleeding on the OC pill
o Ultrasound of no help. Test for other STIs. May require laproscopy
·
Treatment: Antibiotics must cover
anaerobes, chlamydia and gonorrhoea. E.g. Doxycycline 100 mg bd for 10 – 14
days plus an anti-anaerobe such as metronidazole or ornidazole
·
Sequalae:
o Often repeat episodes due to:
§ Continued at risk behaviour
§ Partner is not treated
§ Past infection compromises cilia of the fallopian tubes making another
infection more likely
o Infertility risk after 1 infection is 11%, but up to 54% after 3
infections
o Other sequalae: ectopic pregnancy, adhesions, chronic pelvic pain
Reiter’s Syndrome*
·
Triad of arthritis (big joints –
hot, red swollen, bilateral), urethritis and conjunctivitis
·
10:1 are males, usually 25 – 35
years
·
Often (not always) caused by
chlamydia (an immunological reaction, HLA B27+ more susceptible)
·
Treatment: treat residual
infection, if any
Genital Warts
·
Can get anal warts without anal
intercourse
·
External warts usually benign
(types 6 & 11 – not oncogenic)
·
Treatment:
o Destructive: Condyline, liquid nitrogen – high recurrence rate
o Imiquimod – topical cream, up-regulates immune system, expensive ($150
per month), 19% recurrence, requires treatment for 8 – 12 weeks
·
A vaccine is at stage 3 trials
Non-Sexually Transmitted Genital Skin Lesions
·
Not all skin lesions on the
genitals and surrounding areas are due to STDs
·
Normal anatomical variants:
o Pearly penile papules: small papillae around the corona of the penis
o Sebaceous cysts of the penis, labia minora and scrotum
o Normal papillae in the vaginal vestibule: can be mistaken for warts
·
Dermatoses:
o Contact dermatitis: soaps, deodorants, etc
o Psoriasis: especially head and corona of the penis. Red, scaly plaques.
Not itchy. Look for it elsewhere
o Reiter‟s Syndrome: urethritis, conjunctivitis, arthritis in addition to
skin lesion
o Lichen Planus: itchy plaques on the penis
·
Infections (not necessarily
sexually acquired):
o Seborrhoeic dermatitis: a fungus, red, sharply defined area covered with
honey coloured scales
o Candidiasis: red, irritating, itchy rash. Treat with Clotrimazole (Canesten)
o Dermatophyte infections (tinea) are common. Characteristic spreading edge, itchy
o Folliculitis: small pustule around a hair follicle
o Scabies: red, itchy nodules – may not resolve despite treatment. Treat with malathion 0.5%
o Erythrasma: scaly, flat, brown, pigmented rash, not itchy. Caused by corynebacterium
o Molluscum contagiosum: may be sexually acquired. Small, pearly
umbiliated lesions on the thigh and buttocks
HIV
· The virus: RNA virus with reverse transcriptase. Has p24 nuclear antigen. Attacks CD4+ T cells.
· Transmission: sex (risk in receptive intercourse – male to male most significant, also in other STDs), blood and maternal transmission (¯ risk with AZT)
·
1 % of Europeans lack CXR-5
receptor: if homozygous then resistant
·
Signs & Symptoms:
o Temperature, wasting (chronic ill health)
o Rashes: eg shingles, HSV (cold sores), candidiasis, may be drug response
(heightened sensitivity to drug responses)
o Lymph nodes
o Signs of high risk behaviour: Injection marks, other STD
o Mouth: infections, Kaposi‟s Sarcoma (re-purple vascular non-tender
tumours – mainly on skin)
o Chronic cough common
o Hepatosplenomegaly (infections, lymphoma)
o Neuropathies: eg due to intracranial lesion (eg lymphoma), peripheral
sensory neuropathies
o Fundi: cotton wool spots, scars (eg due to toxoplasmosis, CMV)
·
Early disease:
o Seroconversion illness: in 50 – 90% of infected people. May include macular rash
o Debate about usefulness of early treatment
o Good evidence of value of prophylactic treatment (e.g. following needle
stick)
·
Screening:
o 3 weeks before positive after infection
o Elisa for HIV-1 and HIV-2 antibodies
o False positive tests: 4/1000
·
Confirmatory diagnosis: Western
Blot
o Can take up to 3 months to get Western Blot Positive
o Can give indeterminate, weak positive or strong positive (3 bands)
·
Course: measure based on viral
load and CD4 count
o Acute illness: 4 – 8 weeks
o Asymptomatic: 2 – 12 years
o Symptomatic: 2+ years. AIDS defining illness:
§ PCP infection (treat with co-trimoxazole): can ®
pneumothorax
§ Cryptococcus infection: mild headaches: lumbar puncture. Indian ink stain positive
§ Kaposi‟s sarcoma: can present anywhere
§ Psychological: HIV related, secondary illness related, or depression
·
Viral Load:
o High T cell turnover: Virus
replicates in 1½ days. Infected cell
lasts 2.2 days
o HIV in sanctuary sites: e.g. brain – hard to treat
o Measure through PCR of viral RNA: good indicator of progression. If viral load high, treat now
·
Immune depletion: Based on CD4+
count:
o > 500
o 200 – 500: Tb, herpes
o <200
·
Subgroups of illness:
o Constitutional: fever, diarrhoea, weight loss
o Neurological: dementia, neuropathy, cognitive
o Opportunistic infections: candida, PCP, toxoplasmosis, CMV, MAC, Tb
o Malignancies: Kaposi‟s sarcoma, non-Hodgkin‟s lymphoma
·
Drug Treatment:
o Combination of drugs that inhibit various points of viral replication
o Can improve CD4+ count from very low (e.g. 50) to e.g. 500-600
o Side-effects: non-specific rashes, „buffalo hump‟ – abnormal fat
distribution
·
Leading cause of death:
Respiratory infection
Testing for HIV
·
Guidelines for HIV pre-test
counselling:
o What the test for HIV antibodies means: not a test for AIDS
o Significance of negative test (Window period)
o Significance of positive test: medical implications (prognosis &
treatment), social implications (coping, support, relationships, who needs to
know, possible discrimination), notification requirements (HIV not notifiable,
patient can use alias), implications for insurance
o Safeguards to preserve confidentiality
o Future preventative aspects: safer sex and IVDU
o How results are obtained
o Any costs
·
Guidelines for post test
counselling:
o Explanation of test results
o If negative: 3-month window period – especially if recent high risk behaviour. Future prevention
o If positive: repeat, confirmatory test organised, arrangement for counselling, support and specialist assessment
Other Causes of Secondary Immunodeficiency
·
Malignancy
·
Drugs e.g. steroids, cyclosporin,
cytotoxics
·
Nutritional Deficiency
·
Post-viral
·
Post-transfusion
·
Alcoholism
·
Chronic renal disease
Related Topics