Chapter: Medicine Study Notes : Reproductive and Obstetrics
Abnormal Labour
Abnormal Labour
·
Risks to foetus in distress:
o Hypoxia +/- ischaemia
o Trauma
o Meconium aspiration (meconium = first stool. Abnormal to find it in amniotic fluid).
·
= Labour does not progress
normally. Due to problems with:
o Power – eg hypoactive uterine contractions, or hyperactive (eg spasm)
o Passage – disproportion between the size of the pelvis and the fetus (eg
scarred cervix)
o Passenger – abnormal lie, presentation, position or structure of the fetus
o Psyche – excessively anxious or sedated mother (but if sedatives can ¯contractions
then probably not true labour), conduction anaesthesia (ie epidural) may weaken
lower uterine contractions and therefore not assist head rotation and flexion
·
Types:
o Protracted labour – takes longer than normal
o Arrested labour – progresses normally then stops. During active stage,
progress = either further dilation or
further descent
o Can happen at any stage
·
Causes of failure to progress:
o Prolonged latent phase
o Primary dysfunctional labour: never enters active phase. Associated with
primagravids, OP or deflexed neck, post maturity and unripe cervix
o Secondary arrest: enters active phase then stops. More likely than
primary dysfunctional labour to be associated with absolute cephalo-pelvic
disproportion
o Cervical dystocia: Primary (rare) or secondary (eg following cone
biopsy)
·
Evaluation:
o Palpate or monitor uterine contractions
o Perform cervical exam (and check history)
o Determine lie/position of fetus
o Review medication
·
Treatment:
o Hypertonic contractions – pain medication, Syntocinon
o Hypotonic contractions – Syntocinon, AROM (artificial rupture of
membranes)
·
Abnormal Presentations:
o Breech. More prone to abnormal labour. C-section if < 1000 gm (body
comes through at 7 – 8 cm dilated and head gets stuck = “entrapment of
after-coming head) or > 3600 or 4000 gm. C-section becoming more routine for
any breech
o Face (rather than occiput first). Occurs with complete extension. Mentum
(chin) anterior can be delivered vaginally. Don‟t use forceps and Syntocinon
o Brow. Incomplete flexion (midway between face and vertex). Converts to
either face or occiput – can‟t deliver as brow
o Occiput transverse: Head can‟t flex and rotate from transverse to
occiput anterior. Gets stuck at iliac spines. Risk factors include pelvis shape
(wide and squashed = platypoid). Rotate manually or with forceps, or C-section
o Occiput posterior (ie face up): 5 – 10 %, prolonged second stage,
painful labour (lots of back pain), bigger tears and episiotomies
·
Abnormal fetal structure:
o Macrosomia
o Hydrocephalus
o Hydrops Fetalis: total body oedema eg due to heart failure secondary to
Rh-isoimmunisation
o Meningocoel (a neural tube
defect)
·
Pelvic abnormalities:
o Inlet: failure to descend/engage (failure to descend prior to labour in
a nullip is a bad sign)
o Mid: smaller capacity than inlet, often associated with OT/OP
o Outlet: rare in the absence of contracted mid-pelvis
Cardiotocography (CTG) in Labour
·
= Fetal heart rate monitoring
·
Look at rate (normal = 110 –
160), variability (> 5 bpm), accelerations (2 of at least 15 bpm in 20
minutes).
·
Don‟t want: Basal rate < 110
or > 160, ¯ variability for longer than 45 – 60 minutes, or spontaneous
decelerations
·
Early decelerations (ie with a
contraction) are probably normal (due to pressure on the head ® ¯HR -
?Cushings type reflex). Last decelerations (following
a contraction) are a sign of fetal hypoxia. “Shouldering” (brief HR either
side of a deceleration) may signal cord compression
·
Early hypoxia is indicated by a
mild tachycardia, reduced variability and consistent late decelerations. 80%
sensitivity (ie 1 in 5 unnecessary interventions). A not normal but not
abnormal trace has a 20 – 50% sensitivity for hypoxia
·
A poor CTG is an indicator only.
May do scalp sample to confirm (pH < 7.2 or base excess > -12 getting bad
Þ deliver now by the safest means). Would act now on a bad trace if not
in labour or prolonged bradycardia < 80
·
Red hearings:
o Check material BP. Hypotensive mother ® poor
trace. Eg following epidural insertion, vena cava compression (change position)
o Hyperstimulation: contractions to long or fast ® turn
down syntocinon
Methods of Induction
·
Prostaglandins on the cervix
·
Artificial rupture of membranes
·
Oxytocin drip
Forceps
·
To provide traction, rotation or
both to the fetal head
·
Indications: delay in second
stage, fetal distress, malposition, poor maternal effort, etc
·
Types: outlet, mid or low –
depends on the station of the fetal head and degree of rotation
·
Should never be used when fetal
head is not at least at 0 station (unengaged) as you don‟t know if the head
will fit through
·
Requirements: cephalic
presentation, known position, contractions present (mum needs to push at same
time), ROM, fully dilated otherwise cervical tear (® bleeding
and possible future cervical incompetence), empty bladder and adequate
anaesthesia
· Complications:
o Maternal: vaginal, cervical or uterine laceration, bleeding, bladder or
bowel injury, often episiotomy
o Fetal: bruising, scalp, skull, eye or brain injury
Ventouse/Vacuum
·
Suction applied over posterior
fontanelle
·
Less space necessary, often leads
to spontaneous flexion/rotation, don‟t need to know exact fetal position, will
pop off if too much pressure ® less risk of trauma to mum or baby
Caesarean section
· Types (refers to uterine not skin incision):
o Lower segment transverse: ¯risk of uterine rupture in subsequent pregnancy (<1%)
o Classical: vertical incision in upper segment of the uterus. 5 – 6 %
risk of rupture in subsequent pregnancy. Bleeding, infection, ileus
o Low vertical: vertical incision in the lower segment – treat as classical
o Indications for classical: preterm breech, fibroids, anterior placenta
praevia, transverse lie with back down
·
Risks to mother:
o 4 – 6 times greater than for vaginal delivery
o Anaesthetic risk for mother. Especially aspiration (slow digestion ® usually something in the stomach). Give antacid and Maxolon (¯acidity if aspirates and ¯ vomiting). Give 02 to mum ® ¯fetal hypoxia. Group and hold. Usually use spinal or epidural anaesthetic (although ® vasodilation ® ¯BP ® fetal distress)
o Infection
o Bleed (placenta gets 500mls of blood a minute at term). May ® hysterectomy.
o DVT (pregnant, surgery and immobile) ® PE (most common cause of
maternal death)
o Future obstetric complications:
§ Risk of
caesarean section next time. Can normally trial labour and 70% will progress
normally. 1% uterine rupture (pain, hypotensive). Can‟t be induced if previous Caesar – strong
contractions against a closed cervix ® risk of rupture
§ Risk of placenta growing in the scar next time. May ® placenta
accreta (abnormal adherence to uterus which ® risk of PPH)
·
Indications:
o Placental: praevia, abruption, vasa praevia
o Fetal: disease (eg hydrops), malpresentation, distress, cord prolapse
o Maternal: eclampsia, severe PET, active HSV, cardiac disease, cervical
cancer, prior uterine surgery, obstruction (eg fibroids, ovarian tumours)
·
Herpes Simplex Virus: Caesarean
indicated if current genital outbreak at delivery. Only approx 1% of babies
infected but approx 50% mortality if infected
Perinatal Asphyxia
·
Asphyxia: cessation of gas
exchange ® hypoxia and hypercarbia. Can occur in utero, intra-partum or
postnatally.
·
Fetal Distress: fetus
demonstrates one or more clinical indicators of hypoxia (eg early passage of
meconium and HR changes on CTG)
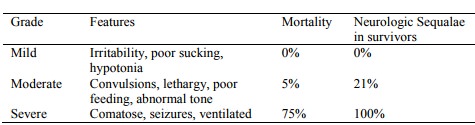
· Hypoxic-ischaemic encephalopathy (HIE): clinical manifestation in the neonate of a previous hypoxic-ischaemic insult. Need for resuscitation (or not) at birth does not necessarily correlate with HIE later on:
·
Systemic effects of hypoxia:
o Brain: hypoxic ischaemic encephalopathy (all are potentially reversible
except for this one)
o Kidney: renal failure
o CV: hypotension
o Liver: coagulopathy
o Respiratory: meconium aspiration, pulmonary hypertension
o Gut: ischaemia
Related Topics