Chapter: Medicine Study Notes : Reproductive and Obstetrics
Cervical Cancer
Cervical Cancer
·
Reference: Cervical Screening,
Information for Health Professionals, National Cervical Screening Programme,
Health Funding Authority, October 1998
Epidemiology
·
In NZ, about 200 new cases per
year, 70 – 80 deaths (Þ relatively rare compared with other cancers)
· One in 97 women can expect to get it before 75
·
75% of cases and 80% deaths are
over 35, but CIN lesions can develop young (ie many woman coming for colposcopy
after abnormal smears are 25 – 30).
Aetiology
·
Human Papilloma Virus (HPV):
o HPV 6, 11: condyloma accuminatum
o HPV 16 or 18: Genital dysplasia.
Is a necessary but not sufficient condition for cervical cancer
o Koilocytes: HPV infected keratinocytes with a perinuclear halo. Episomal viral DNA
o Dysplasia: pleomorphic, hyperchromatic mitotically active, high
nuclear/cytoplasmic ratio. Integrated DNA (Kettle fry nuclei)
o HPV Carcinogenesis:
§ Not typical mechanisms
§ E6 binds to p53 (tumour suppressor and accelerates its degradation)
§ E7 binds to RB displacing transcription factors usually sequestered by
RB
·
Other risk factors:
o Early age at first intercourse
o Multiple sexual partners
o High risk male partners
o Smoking
o Herpes
o Immunosuppression
·
Occurs in the transformation
zone: junction in the endocervix between squamous cells of the vagina and
columnar cells of the uterus. Completes development at age 18 – 20, shifting
into the endocervix. Previously in the exocervix and more vulnerable to
damage/infection Þ significance of age at first intercourse
Classification
·
3 grading systems:
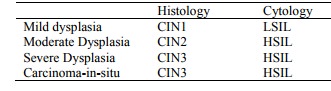
§ Histology Cytology
§ Mild
dysplasia CIN1 LSIL
§ Moderate
Dysplasia CIN2 HSIL
§ Severe
Dysplasia CIN3 HSIL
§ Carcinoma-in-situ CIN3 HSIL
·
Low grade changes: Low Grade
Squamous Intraepithelial Lesion (LSIL) (=CIN1 – Cervical intraepithelial
neoplasia. More likely to be HPV types 6 & 11). Nucleus is slightly
enlarged and irregular. In bottom third of cells on top of base membrane in
transformation zone. If found on screening ® more regular smears. 50 – 60%
return to normal
·
High Grade Changes: HSIL (covers
CIN 2 and 3/CIN – carcinoma-in-situ. More likely to be HPV 16 & 18).
Nucleus of every cell is very enlarged and irregular in shape. High
nuclear:cytoplasmic ratio.
·
Affected cells right to surface.
If found on screening ® refer for colposcopy. Treated the same but CIN3 more likely to progress
than CIN2
·
Invasive cancer: basement
membrane has been breached. Can get glandular extension in CIN3 – metaplasia
down glands – but still not invasive as the BM is not breached
Progression
·
Cervical Dysplasia: grade depends
on the proportion of the epithelium occupied by malignant cells
·
Cervical Carcinoma:
o Micro: islands of infiltrating neoplastic squamous cells that may show
keratinisation
o Outcome: depends on stage
§ Size and depth of invasion. >
10 mm invasion ® poorer outcome
§ Lymph node involvement ® poor outcome
§ Stage 1: confined to cervix. 90 –
95% 5 year survival
§ Stage 3: lymph node positive: 30% 5 year survival
· Cervical glandular neoplasia:
o Also HPV related, but much less common than cervical squamous carcinoma (which has a higher rate of replication)
o Invasive adenocarcinoma has infiltrating neoplastic glands
o Comprises 20% of tumours in a screened population vs 5% in unscreened
Cervical Screening
·
Pap smears collect exfoliated
cells from the cervix
·
Currently reported on the
Bethesda system which divides dysplasia into LGSIL, HGSIL and ASCUS (Atypical
squamous cells of unknown significance – not sure whether they‟re dysplastic or
reactive. Some will be CIN3 so still need follow-up)
· Procedure:
o Best done mid-cycle (¯blood and ¯bacteria which are a causes of cytolysis)
o Explain first. Ask about LMP, abnormal bleeding, post-coital bleeding, abnormal discharge, if pregnant, and previous smear history and experiences
o Patient Education: discuss feelings about having a smear, emphasise
preventative nature, explain what cervix is, show equipment
o Ensure screen/curtain for patient and sheet
o Label slides first
o Either:
§ Spatula first, one full turn, and if poor endocervical sample follow with brush (only turn one turn otherwise bleeding ® obscures
sample) and use a second slide for the brush.
§ Broom does both well (sample of choice for all age groups) – turn 5 times and wipe
both sides once down slide. Thin
prep: cells mixed up and rubbish removed ® better reading. Can‟t use wooden
spatula.
·
Putting on slide: wipe spatula
once, roll brush (scrubbing it around lyses cells). Fix quickly – within one
second – as drying causes distortion of cells. Fix either in 95% ethyl alcohol
for 20 - 30 minutes or cytofix sprayed from 20 – 30 cms.
·
Data on lab form includes LMP and
clinical details.
·
Biggest cause of ¯
sensitivity is poor sampling. Smears can be unsatisfactory if blood,
inflammatory cells or lubricant present. Smears taken 4 – 5 days prior to the
next period may show cytolysis (cellular degeneration due to bacilli)
Relationship between screening results and lesions
·
From OHCS, p 34:
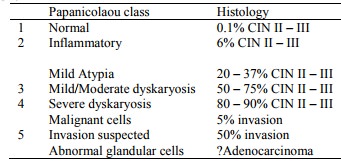
Papanicolaou class Histology
§ 1 Normal 0.1%
CIN II – III
§ 2 Inflammatory 6%
CIN II – III
·
Mild Atypia 20
– 37% CIN II – III
§ 3 Mild/Moderate dyskaryosis 50 – 75% CIN II – III
§ 4 Severe dyskaryosis 80 – 90% CIN II – III
·
Malignant cells 5%
invasion
§ 5 Invasion suspected 50% invasion
·
Abnormal glandular cells ?Adenocarcinoma
·
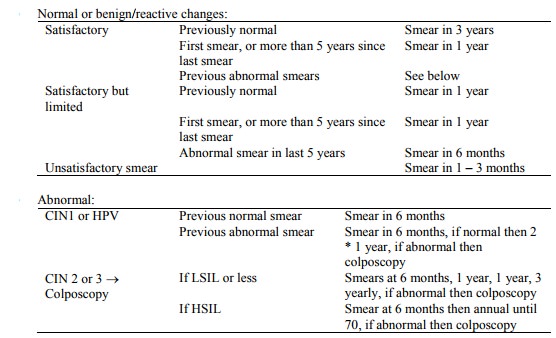
NZ Protocol:
o 3 yearly screening should be offered to all women aged 20 – 69 years who
have been sexually active. Can stop if > 5 years with no sex (this bit not
in the guideline)
o Screening should be yearly for 2 years from 20 (some advocate starting earlier if > 2 years since commencing regular sex – but as cancer in this age group is very uncommon, it‟s not good screening practice. If you think cancer is a possibility, you shouldn‟t use a screening test to diagnose it)
· Sensitivity of a single smear is 80% for low and high grade lesions (ie not sufficient for diagnosis, only for screening)
Effectiveness of Screening
· PPV of HGSIL cytology report: 30 – 40%
·
NPV of a normal smear is 80% Þ if
abnormal appearing cervix (lesion with raised edge, nodular feel, hard, bleeds
when touched) or persistent abnormal bleeding they need a colposcopy not a
smear:
·
DON‟T RELY ON THE SMEAR
·
Maximum prevention: 91-92 % of
squamous cancers with 3 yearly screening. to 92 – 93% with annual
screening. ¯ to 87% with 5 yearly screening
·
Less than 100% because of:
o Less than 100% enrolment
o False negatives in sampling (eg a lesion is more likely to bleed and
compromise the sample)
o False negatives in laboratory diagnosis
o Interval cancers: minimum time from infection to invasive is ~ 18 months. Normal is ~ 10 to 15 years
·
Success rate for adequate
treatment of pre-cancers is 98 – 100%
·
Women most likely to get cervical
cancer are those not regularly screened
·
Much less effective at glandular
lesions: clinical suspicion should overrule a „normal‟ smear
Related Topics