Chapter: Medicine Study Notes : Reproductive and Obstetrics
Menstrual Disorders
Menstrual Disorders
·
Key distinction:
o Ovulatory cycles: regular
o Anovulatory cycles: irregular
·
Also consider thyroid and PRL
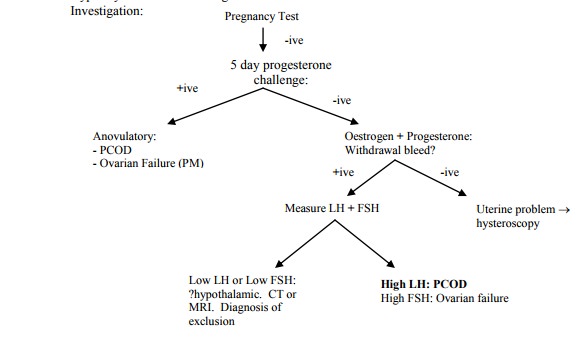
Amenorrhoea
·
Primary amenorrhoea: failure to
start menstruating. Investigate in a 16 year old or a 14 year old with no
breast development. When did her mum start menstruating? Usually normal. Rarely
Turner‟s syndrome or testicular feminisation
·
Secondary amenorrhoea: when
periods stop for > 6 months, except for pregnancy:
o Hypothalamic-pituitary-ovarian causes common. Eg stress, anorexia,
breast feeding, weight loss, PRL, severe disease. Test with a 7-day progesterone challenge. If
withdrawal bleed following, then there is enough oestrogen to produce an
endometrium
o Ovarian causes are uncommon: Polycystic ovarian syndrome, tumours,
premature menopause
o Hyperthyroidism ® oestrogen breakdown
·
Oligomenorrhoea: infrequent
periods: common in the young and the nearly menopausal. Consider polycystic
ovary syndrome, rapid weight change, PRL, hypothyroidism or primary
oligomenorrhoea
Menorrhagia
·
= Excessive blood loss
(technically > 80ml lost/cycle – but hard to measure)
·
Causes:
o ?Hypothyroidism: cold intolerance, weight gain, constipation, goitre, etc
o Younger: pregnancy, dysfunctional uterine bleeding (diagnosis of
exclusion, no pelvic pathology, associated with anovulatory cycles. If young,
may settle)
o Older: IUCD, fibroids, endometriosis, adenomyosis, polyps, pelvic
infection
o Perimenopausal: ?endometrial carcinoma (especially if > 90Kg)
o Haematological: low or dysfunctional platelets (not coagulopathy)
· Investigation:
o bHCG: are
they pregnant
o FBC: anaemic?
o Smear if not up-to-date
o Menstrual calendar
o Abdominal ultrasound
o If age > 45, over 90 kg or infertile with heavy bleeding then transvaginal ultrasound and/or endometrial biopsy (pipelle) to test for endometrial cancer
o Hysteroscopy and curettage for histology if irregular bleeding or
ultrasound indicating polyps or fibroids
·
Treatment if pathology known:
o Anti-PGs (eg NSAIDs) as 1st line treatment
o Progesterone during the follicular phase or CoC
o Intra-uterine devices (eg Mirena)
o Other drugs: Tranexamic acid, norethisterone, Danazol (bad side
effects), etc,
o Surgical options: endometrial ablation (problem with recurrence) or
hysterectomy
Inter-menstrual bleeding
·
May follow mid-cycle ¯ in
oestrogen (ie with ovulation)
·
Also cervical polyps, ectropion,
carcinoma, cervicitis and vaginitis, IUCD, hormonal contraception (spotting)
·
If post-coital, then
suspicion of more serious pathology (eg cervical cancer)
·
Appropriate to do an exam and
smear – but it is NOT appropriate to reply on the smear result (false
negatives, etc). Should act on clinical suspicion
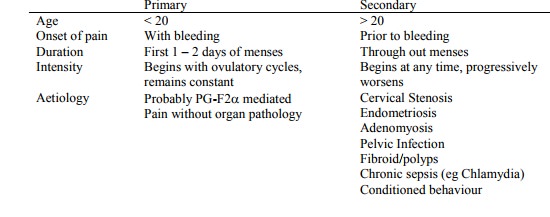
Dysmenorrhoea
·
= Painful periods, may be
associated with sweating, tachycardia, headache:
·
Treatment:
o Reassurance
o CoC: at least 3 month trial, combine with NSAIDs if necessary
o Progestogens: day 5 – 25
o PG inhibitors
o Exercise
o De-conditioning, eliminate secondary gains
Endometriosis
·
= Ectopic endometrial tissue,
histologically confirmed. Most often on ovaries and uterosacral ligaments
·
Chronic and progressive:
inflammation and local haemorrhage ® fibrosis and scarring
·
Incidence:
o 10 – 15% of reproductive age.
Patients usually in mid 30s – early 40s, nulliparous
o Common in infertility and chronic pelvic pain
· Aetiology theories:
o Retrograde menstruation ® homologous grafts
o Genetics: 7 fold risk if +ive family history. Usually earlier and more severe disease
·
Symptoms: classic triad = pelvic
pain, deep dyspareunia, dysmenorrhoea. Also irregular bleeding, infertility
(scars fallopian tubes)
·
On exam: tender, retroverted
uterus
·
Confirmation by laproscopy. Red
brown nodules on surface of ovaries and pelvic structures, and other sites
(appendix, peritoneal scars, etc). Can develop large cysts, lined by endometrial
stroma and glands and containing changed blood (chocolate cysts).
· Treatment:
o Conservative (50% recurrence within 5 years): surgical removal (ablation
or excision) of affected tissue and/or hormonal therapy:
§ Prostaglandin synthetase inhibitors treat pain (NSAIDs)
§ OCPs – promote inactivity of endometrial tissue
§ Progesterones – oral or depot
§ GnRH agonists – short course only due to bone loss
§ Danazol (testosterone derivative)
o Laproscopic resection or ablation of affected peritoneum
o Radical: removal of pelvic organs
Fibroids
·
Benign growths in myometrium (ie
underneath the proliferative layer)
· Very common, especially in overweight and infertility
·
Oestrogen ®
enlargement, so grow in pregnancy and shrink after menopause
·
Aetiology unknown
·
Symptoms: heavy/irregular
bleeding, painful periods, urinary frequency, constipation
·
Diagnosis: abdominal +/- vaginal
ultrasound ® hysteroscopy
·
Treatment:
o Medical:
§ GnRHa can shrink fibroids temporarily. Not for > 6 months, menopausal
symptoms. Also Gestrinone and Danazol.
§ NSAIDs, Progesterone and HRT don‟t shrink fibroids
o Surgical: Hysterectomy, hysteroscopic resection if small and submucosal,
myomectomy (risk of uterine rupture in subsequent pregnancy)
Adenomyosis
·
= Growth of endometrial glands
and stroma into the myometrium. Does not undergo cyclic changes and is not
hormone responsive
·
Symptoms: dysmenorrhoea,
menorrhagia, deep dyspareunia
·
Incidence: age 35 – 50, parous
·
Exam: globular, enlarged uterus,
most tender peri-menses
·
Treatment: NSAIDs, OCPs, GnRH
agonists, Hysterectomy
Premenstrual Syndrome (PMS)
·
= Recurrence of symptoms, whether
emotional or physical, occurring the pre-menstruum but with complete absence of
symptoms in the post-menstruum. Severe symptoms in 5% of women
·
DSM 4 has „Premenstrual Dysphoric
Disorder‟ as a research criteria
·
Main symptoms:
o Depression, irritability, tiredness, headache, bloating, breast
tenderness.
o Plus 150 others!
o Classify as mild, moderate or severe on the basis of interference with
daily function
o Use of a symptom diary over 2 months is very valuable
·
Diagnosis:
o History
o Exam to exclude gynaecological and endocrine disorders
o Tests: rule out thyroid, PRL, secondary dysmenorrhoea (eg endometriosis)
·
Differential:
o Psychiatric: depression or anxiety with premenstrual exacerbation
o Medical: anaemia, hypothyroidism, cancer, SLE, menopause if > 45,
renal causes, polycystic ovary
·
Management:
o Education
o Life-style changes: diet, exercise, ¯smoking
o Psycho-therapy if psych history, for coping skills, or to manage
secondary gains or conditioning
o Drugs:
§ Suppression of ovulation. Eg with CoC – although this can give symptoms
(eg depression, ache, etc)
§ Fluoxetine 20 mg only when symptoms occurring (30% remission, minimal side effects)
§ Debated remedies include evening primrose oil, Vitamin B6 (pyridoxine)
in low dose (neuropathy in high dose)
§ Very high placebo rates
·
Aetiology:
o Multifactorial – includes biological, psychological and societal factors
o Biological hypotheses include abnormal response to ovarian hormones,
mineralocorticoid effects, prostaglandins, etc.
Post menopausal Bleeding (PMB)
·
Bleeding > 1 year after the
last period (check it is vaginal bleeding, not urethra or rectal)
·
Causes:
o Vaginitis (often atrophic): fragile ® trauma, and ¯secretions
®infection
o Foreign bodies (eg pessaries)
o Endometrial or cervical polyps, endometrial fibroids (bleed a lot –
leiomyoma, adenomyosis, hyperplasia)
o Oestrogen withdrawal (HRT or ovarian tumour)
o Carcinoma of the cervix
o Endometrial cancer
·
Distinguish from peri- or
post-menopausal on HRT
·
Investigation: Trans-vaginal US
(looks at thickness of endometrium) and trans-abdominal US (finds other masses)
·
If bleeding on non-cyclical HRT
or intra-cyclical bleeding on cyclical HRT, be a bit more aggressive in
investigation (HRT ® slight risk of endometrial cancer)
Related Topics