Chapter: Medicine Study Notes : Reproductive and Obstetrics
Complications of Early Pregnancy
Complications of Early Pregnancy
Differential of early pain/bleeding
·
20% of women bleed in early
pregnancy – it is never normal Þ investigate
·
Obstetric causes: miscarriage,
ectopic, trophoblastic disease
·
Gynaecological causes: period,
STI, cervical (eg polyps), vaginitis, endometriosis, ovarian cyst (may be
functional ® irregular cycles), PID
·
Non-gynaecological: UTI, GI (eg
haemorrhoids)
·
Exam:
o CV, Resp, temp
o Abdominal: tenderness/guarding/rebound
o Pelvic exam:
§ Speculum: discharge, bleeding, swabs, os
§ Bimanual: mass, endometriosis (® fixed, retroverted uterus and
utero-sacral nodularity on PR), cervical motion tenderness (Þ ?PID)
·
Investigations:
o MSU, FBC
o Blood type + Rhesus
Spontaneous abortion/Miscarriage
·
= Loss of products of conception
before the 20th week.
·
10 – 15% of recognised
pregnancies. >75% in first trimester
and due to fetal causes
·
Threatened abortion: os is closed and fetus is
viable (still has heart beat). Uterus right size for dates. 75% will settle. Associated with preterm delivery
·
Incomplete abortion: cervix is dilating, more pain,
heavier bleeding. Conservative treatment if < 13 weeks. If pain, bleeding or retained tissue on US then suction curettage. Ergometrine
(uterine smooth muscle contractor) for serve bleeding
·
Complete abortion: Products of conception
expelled, bleeding stopped, cervix closed (don‟t confuse with threatened), uterus small for dates
·
Septic Abortion: as for incomplete abortion +
uterine and adnexal tenderness, purulent loss, pyrexia. Can lead to severe sepsis
·
Missed abortion: Fetus dead but not expelled,
uterus small for dates, confirmed by 2 US scans 7 days apart. Usually active management to remove fetus
·
Causes:
o None found – most common
o Chromosomal abnormalities
o Hormonal imbalance: eg failure of corpus luteum to produce enough
progesterone
o Maternal illness, abnormalities of the uterus (eg cervical
incompetence), immunological factors
·
Recurrent miscarriage = loss of
3 or more consecutive pregnancies, occurs in < 1%
Ectopic pregnancy
·
= Any implantation outside the
uterine cavity. > 95% in the
fallopian tube
·
0.5 – 1 % of pregnancies. Fatal if untreated. Most common cause of death in 1st trimester
·
Risk factors – anything slowing
ovum‟s path to the uterus: salpingitis (eg PID), surgery, previous ectopic
(recurrence in 10 – 20%), endometriosis, IUCD
·
Presentation:
o Abdominal pain or bleeding in any sexually active woman
o Usually around 8 weeks amenorrhoea, but may not have missed a period
o Can present with acute rupture – sudden severe abdominal pain and shock
o Shoulder tip pain due to blood in the peritoneum irritating the
diaphragm
o Cervical excitation
· Diagnosis:
o bHCG – low for gestational age and rises slower than normal (normal doubling time is 2 days)
o ?Quantitative bHCG: at 1500-2000 should see sac on trans-vaginal US, at 6000 should see sac on abdominal US
o US can visualise in 2% of cases – key finding is empty uterus
o Laproscopy is gold standard
·
Treatment: surgical or
methotrexate (folate antagonist)
Trophoblastic disease
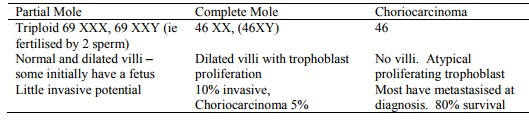
·
Complete or partial hydatiform
mole: abnormal placenta without/with a fetus. Placenta replaced by a mass of
grape-like vesicles
·
Choriocarcinoma: malignant invasion by trophoblastic cells –
can arise years after a pregnancy
·
1 in 2000 pregnancies
·
Risk factors: early or late
maternal age, previous mole, previous multiple pregnancies
·
Presentation:
o Uterus large for dates in 50%
o Vaginal bleeding +/- passage of grape-like villus
o Early pre-eclampsia
o Very high levels of HCG
o Ground glass appearance on US and no fetus or absence of fetal
movements/heart sounds
Hyperemesis gravidarum*
·
Rare (1 in 1000). Risk if young and primip
·
Presents with inability to keep
food or drink down, hypovolaemia, polyneuritis (¯Vit B),
liver and renal failure
·
Admit to hospital. Rehydrate, exclude UTI, twins, and hydatiform
mole
Cardiovascular Problems in Pregnancy
·
Common clinical findings in
pregnancy: pulse volume, JVP pressure waves, heart size (apex beat displaced by approx 1 cm), loud first heart sound,
3rd heart sound, ejection systolic murmur up to grade 3/6 in 90% women,
peripheral oedema
·
Maternal mortality = 1 per 10,000
– most in puerperium (especially mitral problems ® ¯pulmonary
flow ® pulmonary oedema, especially during 3rd stage of labour due to sudden in blood
volume as uterus contracts).
·
Risk of heart failure, especially
due to Rheumatic fever, congenital disease, Marfan‟s, prosthetic valves, given
reduced functional reserve in pregnancy (ie further stresses an already
stressed heart)
·
Fetal mortality: usually little
impact, except mums with cyanotic congenital heart disease
·
History: breathlessness (although
very common in pregnancy), syncope, arrhythmia
·
ECG: T wave inversion in III, S-T
changes and Q waves occur frequently. ECG best for arrhythmias, not structural
problems (use echocardiogram)
·
Management: avoid exacerbating
factors: infection, hypertension, obesity, anaemia, arrhythmias, smoking etc.
Multiple pregnancy ® further 30% increase in CO which compromises function further
·
Drug Treatment: digoxin, diuretic
therapy, b blockers
·
Labour: care not to fluid
overload, monitor BP carefully (don‟t want it either up or down – care with
aorto-caval compression and epidural).
Related Topics