Chapter: Ophthalmology: Optic Nerve
Papilledema
Papilledema
Definition
Bilateral optic disk edema secondary to
increased intracranial pressure.
Epidemiology:
Epidemiologic data from the 1950s describe papilledema inas many
as 60% of patients with brain tumors. Since then, advances in neu-roradiology
have significantly reduced the incidence of papilledema. The diagnostic
importance of the disorder has decreased accordingly.
Etiology:
An adequate theory to fully explain the pathogenesis of
papil-ledema is lacking. Current thinking centers around a mechanical model in
which increased intracranial pressure and impeded axonal plasma flow through
the narrowed lamina cribrosa cause nerve fiber edema. However, there is no
definite correlation between intracranial pressure and promi-nence of the
papilledema. Nor is there a definite correlation between the times at which the
two processes occur. However, severe papilledema can occur within a few hours
of increased intracranial pressure, such as in acute intracranial hemorrhage.
Therefore, papilledema is a conditional,
unspecificsign of increased intracranial pressure that does not provide
conclusive evi-dence of the cause or location of a process.
In approximately 60% of all cases, the
increased intracranial pressure with papilledema is caused by an intracranial tumor; 40% of all cases are
due to other causes, such as hydrocephalus, meningitis, brain abscess,
encephalitis, malignant hypertension, or intracranial hemorrhages. The patient
should be referred to a neurologist, neurosurgeon, or internist for diagnosis
of the underlying causes.
Every incidence of papilledema requires
immediate diagnosis of the underlying causes as increased intracranial pressure
is a life-threatening situation.
The incidence of papilledema in the presence
of a brain tumor decreases with increasing age; in the first decade of life it
is 80%, whereas in the seventh dec-ade it is only 40%. Papilledema cannot occur
where there is atrophy of the optic nerve, as papilledema requires intact nerve
fibers to develop.
Special forms:
❖ Foster Kennedy syndrome: This refers to isolated atrophy of the optic nervedue to
direct tumor pressure on one side and papilledema due to increased intracranial
pressure on the other side. Possible causes may include a meningioma of the
wing of the sphenoid or frontal lobe tumor.
❖ Hypotension papilledema: This refers to a nerve fiber edema due to ocularhypotension.
Possible causes may include penetrating trauma or fistula secondary to
intraocular surgery.
Symptoms and diagnostic considerations:
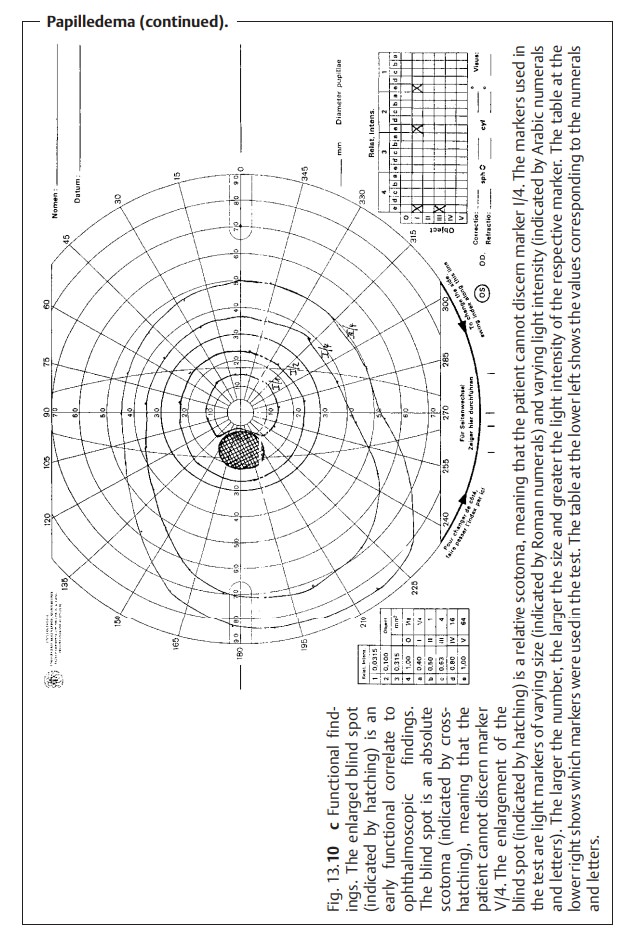
Visual function remains unim-paired for long
time. This significant discrepancy between morphologic and functional findings
is an important characteristic in differential
diagnosis. Early functional
impairments can include reversible obscurations.Perimetrytesting may reveal an increase in the size of the blind
spot (Fig. 13.10c). Cen-tral visual
field defects and concentric narrowing of the visual field are latefunctional impairments that occur
with existing complex atrophy of theoptic nerve.
Papilledema is characterized by significant
morphologic findings and only slight visual impairment.
The following phases may be distinguished by ophthalmoscopy:
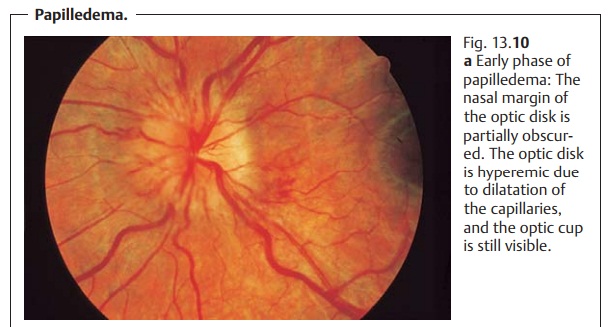
Early phase (Fig. 13.10a): First the nasal margin and then the superior andinferior
margins of the optic disk are obscured because of the difference in the
relative densities of the nerve fibers (see optic disk). The optic cup is initiallypreserved. This is important
in a differential diagnosis to exclude pseudo-papilledema and optic disk
drusen. The optic disk is hyperemic due to dilata-tion of the capillaries, and
there is no pulsation in the central retinal vein. Edema can produce concentric
peripapillary retinal folds known as Paton’s folds.
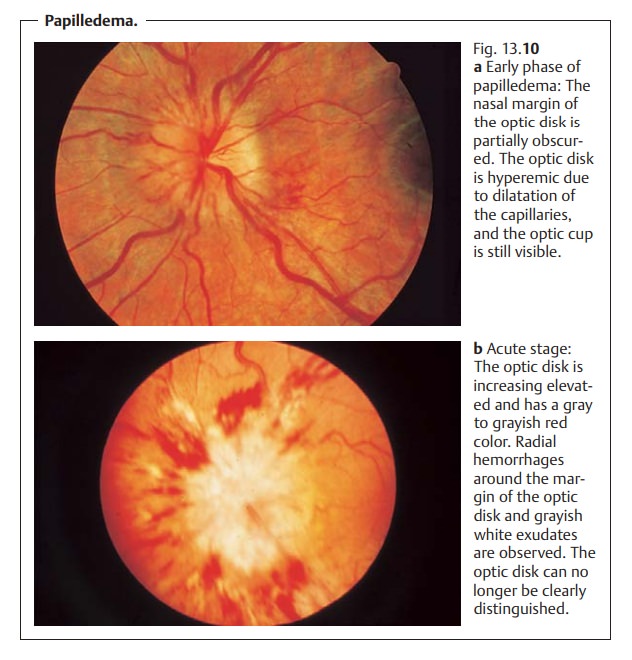
Acute phase (Fig. 13.10b): This is characterized by increasing elevation of theoptic
disk, radial hemorrhages around the margin of the optic disk and gray-ish white
exudates. The optic cup is often no
longer discernible. The color of the optic disk will be red to grayish red.
Chronic phase.Significant optic disk edema is present.The optic cup is oblit-erated, and the hyperemia will be seen to
subside.
Atrophic phase.Proliferation of astrocytes results in complex or secondaryatrophy
of the optic nerve.
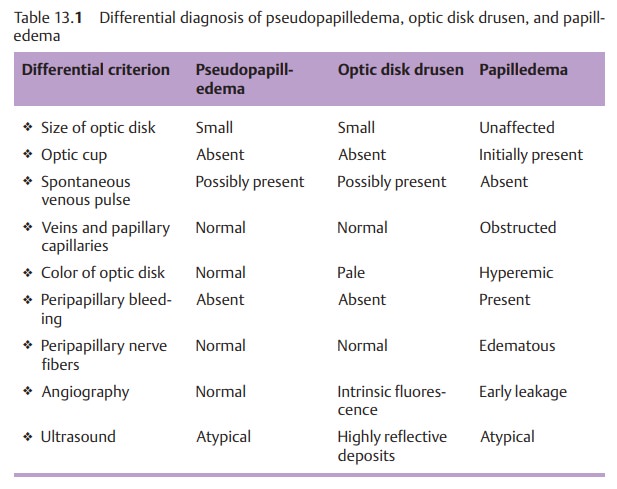
Differential diagnosis:
This includes pseudopapilledema, optic disk drusen(Table 13.1), abnormalities of the optic disk
without functional impairment, optic disk edema with hypertension, and optic
neuritis.
Treatment:
Intracranial pressure should be reduced by treating the
underly-ing disorder (see Etiology). Once intracranial pressure has been
normalized, the papilledema will resolve within a few weeks. Usually complex
atrophy of the optic nerve will remain. The severity will vary according to the
duration of the papilledema.
Related Topics