Chapter: Ophthalmology: Optic Nerve
Optic Neuritis
Optic Neuritis
Definition
Optic neuritis is an inflammation of the optic
nerve that may occur within the globe (papillitis)
or posterior to it (retrobulbar optic
neuritis).
Epidemiology:
Optic neuritis occurs most frequently in adults between theages of 20 and 45. Women are more frequently affected than men. Twenty to forty per cent of all patients with optic neuritis develop diffuse encephalitis (multiple sclerosis).
Etiology:
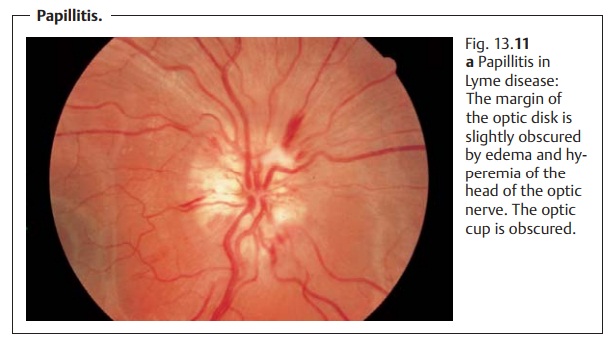
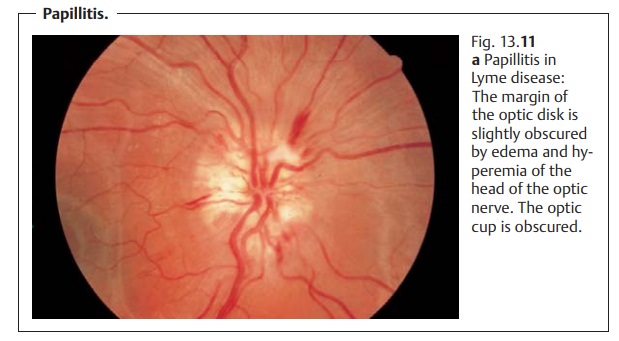
Papillitis.
❖ Inflammatory processes: These include infectious diseases such as Lymedisease, malaria,
and syphilis, and manifestations in the optic nerve of inflammation of the
orbit, paranasal sinuses, or base of the skull.
❖Autoimmune disorders: These include lupus erythematosus, polychon-dritis, regional
enteritis (Crohn’s disease), ulcerative colitis, nodular panarteritis, and
Wegener’s granulomatosis.
❖ Toxic damage due to agents such as methanol, lead, Myambutol (ethambu-tol
hydrochloride), and chloramphenicol. In 70% of these cases, the cause isnot determined.
Retrobulbar optic neuritis.The primary causes of this disorder aredemyeli-nating diseases of the central nervous system such as
diffuse encephalitis. In20% of all cases, retrobulbar optic neuritis is an
isolated early symptom of dif-fuse encephalitis. However, a differential
diagnosis should always also con-sider the other
causes of papillitis mentioned above.
Symptoms:
The cardinal symptomissudden loss of vision, which may
occa-sionally be accompanied by fever (Uhthoff
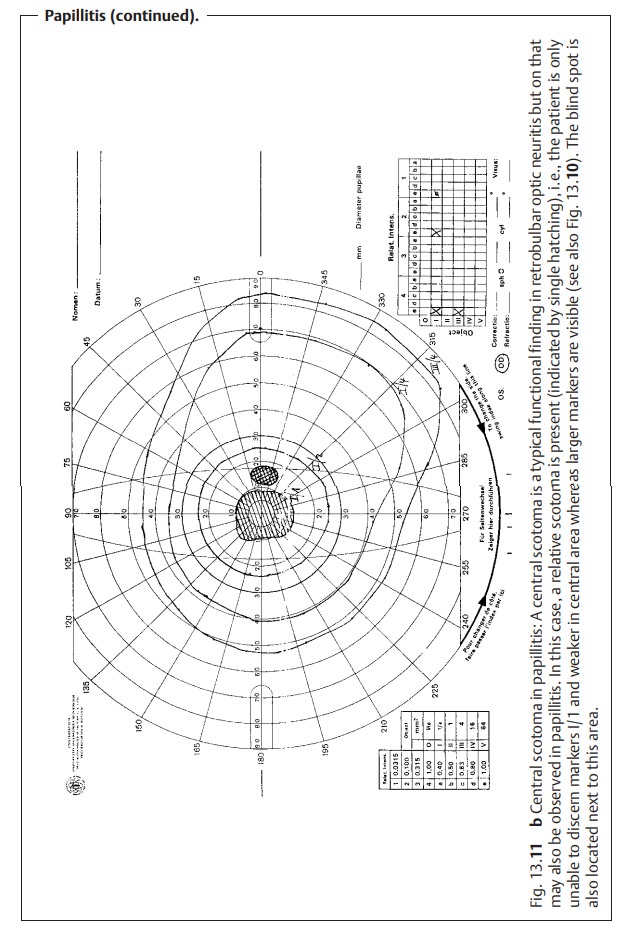
symptom). The field of vision is typically impaired by a central scotoma
(Fig. 13.11b), paracentral scotomas,
acentrocecal scotoma
involving the macula and blind spot, and wedge-shaped visual field defects up
to and including complete blindness.
Other symptoms include pain that increases in extreme positions of gazeand when
pressure is applied to the globe, and reduced perception of color intensity.
Diagnostic considerations:
Ophthalmoscopic findings inpapillitis(Fig.13.11a) include edema and hyperemia of the
head of the optic nerve. This flat-tens the optic cup and obscures the margin
of the optic disk. Bleeding at the margin of the optic disk may or may not be
present. The elevation of the optic disk is considerably less than in
papilledema.
The optic disk will appear normal in retrobulbar optic neuritis.
In retrobulbar optic neuritis, the patient
sees nothing (due to a central scotoma), and the physician sees nothing (the
fundus appears normal).
Other findings upon examination include an afferent pupillary defect (this isregularly
encountered;, red-green color vision defect, and delayed latency in the visual
evoked potential.
Differential diagnosis:
Papilledema: Initially there is no loss of function.
Ischemic optic neuropathy: The central scotoma is lacking, and patients areusually over the
age of 60.
Treatment:
This depends on the underlying disorder. Retrobulbar
opticneuritis with severe loss of vision (less than 0.1) may be treated with
high doses of steroids, i.e., 1000 mg of oral prednisolone daily for three days
and 1 mg of oral prednisolone per kilogram of body weight on days four through
fourteen. However, this treatment only leads to more rapid restoration of
vision. Final visual acuity after one year is identical with or without
high-dose steroid therapy.
Prognosis:
This depends on the underlying disorder. Severe permanentlosses
of visual acuity are possible, as are significant spontaneous improve-ments. Retrobulbar optic neuritis in diffuse
encephalitis usually exhibits a strong tendency toward spontaneous
improvement within four weeks without any treatment. However, discrete functional defects such as
reduced visual contrast and reduced perception of color intensity will always remain. Morphologic findings always include a pale optic disk as a result of complex atrophy of the optic nerve
following papillitis or partial isolated atrophy of the optic nerve following
retrobulbar optic neuritis.
Related Topics