Chapter: Ophthalmology: Optic Nerve
Congenital Disorders that Obscure the Margin of the Optic Disk
Disorders that Obscure the Margin of the Optic Disk
Congenital Disorders that Obscure the Margin of the Optic Disk
There are normal
variants of the optic disk in which the margin appears fully or partially
blurred. Care should be taken to distinguish them from abnormal findings.
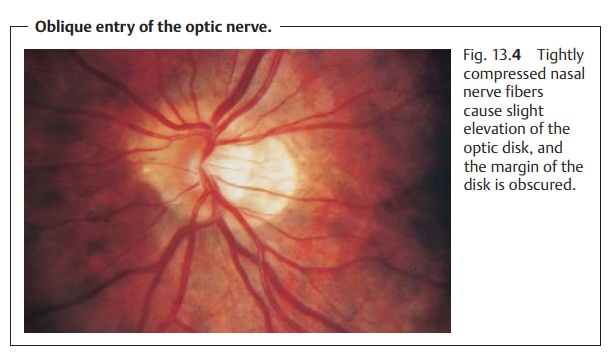
Oblique Entry of the Optic Nerve
Where the optic nerve exits the eye in an oblique and nasal direction (Fig. 13.4), the nerve fibers on the nasal circumference will be elevated. The tightly compressed nasal nerve fibers will obscure the margin of the optic disk.Accordingly, temporal nerve fibers are stretched, and the neuroretinal rim can-not be clearly distinguished. Often an adjacent crescentic whitish area, known as a temporal crescent, will be observed on the temporal side. This crescent is frequently seen in myopia and is referred to as a myopic crescent. It can also be circular.
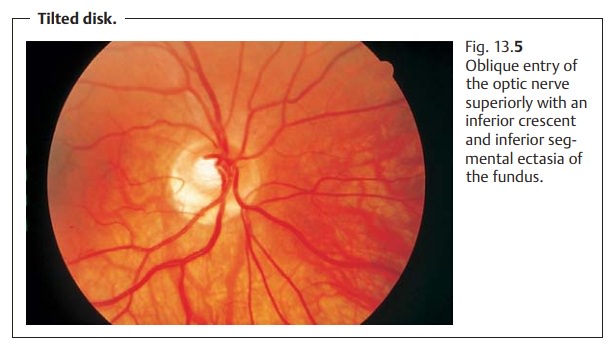
Tilted Disk
An optic nerve that exits the eye superiorly (Fig. 13.5) is referred to as a tilted disk. The superior circumference of the margin of the
optic disk will be obscured in a manner similar to oblique entry of the
optic nerve. A number of other changes may also be observed, including an
inferior crescent, situs inversus of the retinal vessels, ectasia of the
fundus, myopia, and visual field defects. These findings may occur in various
combinations and are referred to collec-tively as tilted-disk syndrome. This is clinically
highly significant as nasal inferior ectasia of the fundus can produce
temporal superior visual field defects. Where these findings are bilateral,
care should be taken to distin-guish them from pituitary tumors. This clinical
picture is regarded as a form of rudimentary
coloboma.
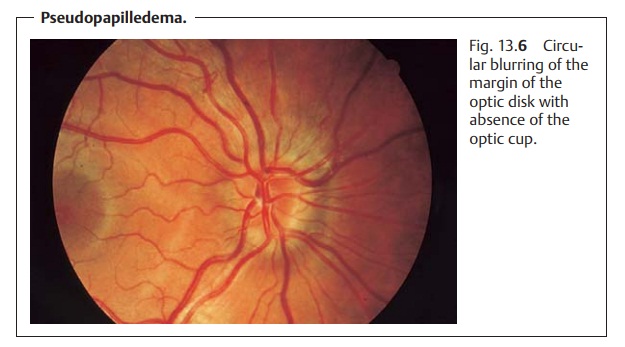
Pseudopapilledema
Pseudopapilledema (Fig. 13.6) is due to a narrow scleral canal. Because of the constriction, the nerve fibers are tightly compressed. The optic disk is ele-vated and the full circle of the margin obscured. The optic cup is absent, andthe retinal vessels appear tortuous. There are no abnormal morphologic changes such as bleeding, nerve fiber edema, and hyperemia; visual acuity and visual field are normal. Pseudopapilledema can occur with hyperopia, although it is encountered equally frequently in emmetropic or slightly myopic eyes.
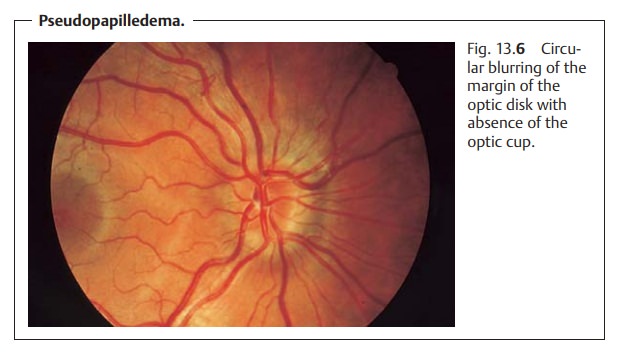
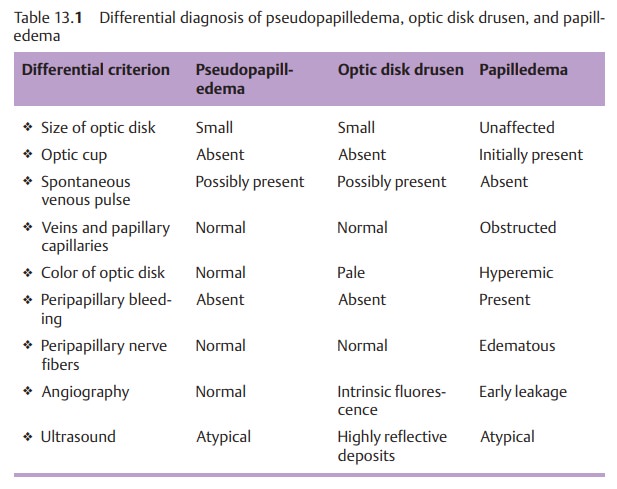
Differential diagnosis: optic disk edema, optic disk drusen (see Table 13.1).
Myelinated Nerve Fibers
Normally retinal nerve fibers are not myelinated. However, myelinated areas occasionally occur in the retina (Fig. 13.7). They occur most frequently at the margin of the optic disk.
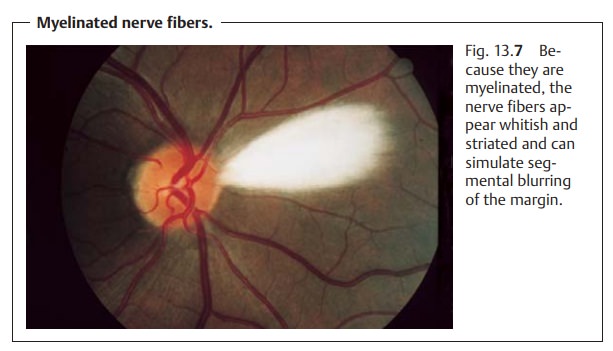
Whitish and striated, they simulate segmental orcircular
blurring of the margin. Myelinated nerve fibers can also occur on theperiphery of the retina. Because of their location
in the innermost layer of theretina, they tend to obscure the retinal vessels.
Myelinated nerve fibers nor-mally cause no loss of function. Only extensive
findings can lead to small sco-tomas.
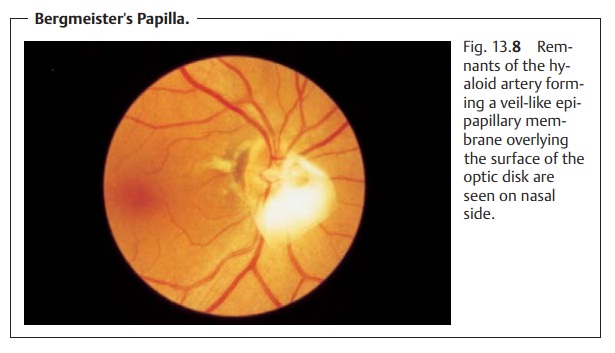
Bergmeister’s Papilla
The fetal hyaloid artery emerges from the
optic disk to supply the vitreous body and lens. Glial and fibrous tissue may
persist if the structure is not fully absorbed. This vestigial tissue, usually
on the nasal side of the optic disk, is known as Bergmeister’s papilla. When this tissue takes the form of veil-like
membrane overlying the surface of the optic disk, it is also referred to as an epipapillary membrane (Fig. 13.8). Usually
this condition isasymptomatic.
Optic Disk Drusen
Drusen are yellowish lobular bodies in the tissue of the optic disk that areusually bilateral (in 70% of all cases). Ophthalmoscopy can reveal superficialdrusen but not drusen located deep in the scleral canal. In the presence of optic disk drusen, the disk appears slightly elevated with blurred margins andwithout an optic cup (Fig. 13.9). Abnormal morphologic signs such as hyper-emia and nerve fiber edema will not be present. However, bleeding in lines along the disk margin or subretinal peripapillary bleeding may occur in rare cases.
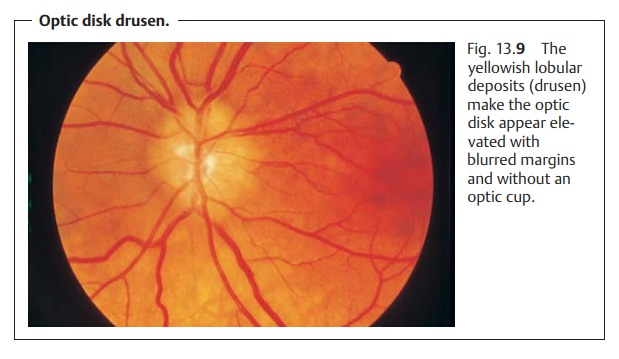
A small lamina cribrosa appears to be a factor
in the etiology of the dis-order.
This impedes axonal plasma flow, which predisposes the patient to axonal
degeneration. This in turn produces calcifications exterior to the axons
(drusen). Retinal drusen are hyaline deposits in Bruch’s membrane and are a
completely unrelated process.
Drusen usually do not cause any loss of
function. Deep drusen can
cause compressive atrophy of nerve fibers with resulting subsequent visual
field defects.
Optic disk drusen may be diagnosed on the
basis of characteristic ultra-sound findings of highly reflective papillary
deposits. Fluorescein angiogra-phy findings of autofluorescence prior to dye
injection are also characteristic.
See Table 13.1 for differential
diagnosis.
Related Topics