Chapter: Ophthalmology: Optic Nerve
Anterior Ischemic Optic Neuropathy (AION)
Anterior Ischemic Optic Neuropathy (AION)
The following forms of anterior ischemic optic
neuropathy (AION) are distin-guished according to the cause of the disorder:
❖ Arteriosclerotic anterior ischemic optic neuropathy.
❖ Arteritic anterior ischemic optic neuropathy.
Arteriosclerotic Anterior Ischemic Optic Neuropathy
Definition
An acute disruption of the blood supply to the
optic disk, i.e., optic disk infarc-tion, resulting from vascular changes in
arteriosclerosis.
Epidemiology:
Arteriosclerotic AION is a common cause of
sudden loss ofvisual acuity. The greatest incidence of this disorder is between
the ages of 60 and 70. In contrast to arteritic AION, it can also occur in
adults below the age of 60.
Etiology:
The causes of the disorder lie in acute disruption of the blood flowthrough the lateral branches of the short posterior ciliary arteries and the ring of Zinn in the setting of severe arteriosclerosis. A narrow scleral canal, i.e., a small optic disk, is a predisposing factor. The disorder known as diabeticpapillopathy also belongs to this group of disorders, although it has a betterprognosis in terms of vision.
Symptoms:
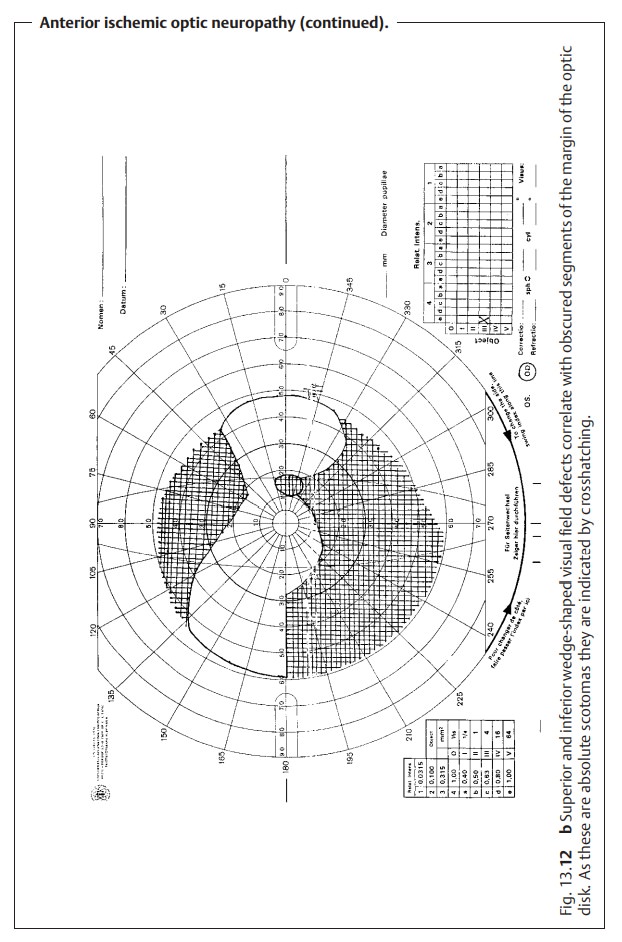
Patients report asudden unilateral loss of visual acuity. This is dueto segmental or
complete infarction of the anterior portion of the optic nerve. Severity is
variable. The patient may present with wedge-shaped visual field defects (Fig.
13.12b) or horizontal visual field
defects that correlate with seg-mental nerve fiber edemas. However, severe
concentric defects progressing to total blindness can also occur. Vision may or
not be impaired. An afferent pupillary defect is always present.
Diagnostic considerations:
The patient will frequently have a history
ofhypertension, diabetes mellitus, or hyperlipidemia.
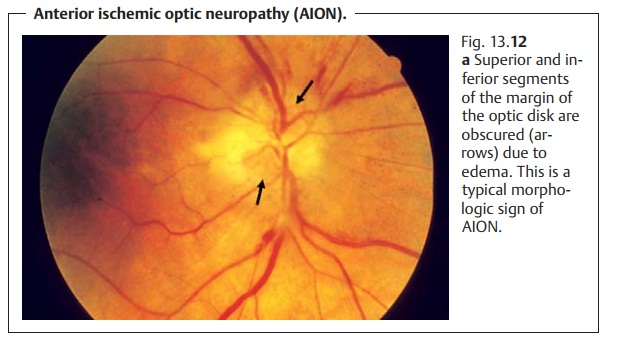
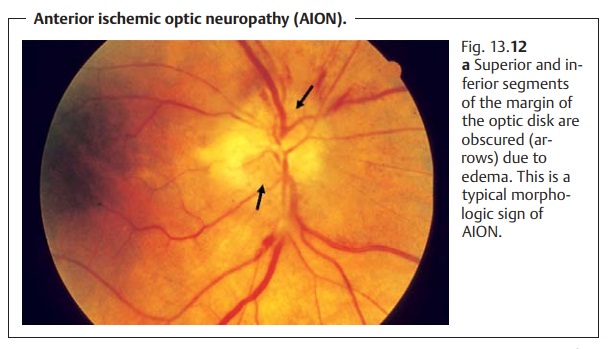
Ophthalmoscopy will reveal edema of the optic disk, whose margin willbe
accordingly obscured. The margin is often obscured in a segmental pat-tern,
which is an important criterion in differential diagnosis (Fig. 13.12a). The head of the optic nerve is
also hyperemic with marginal bleeding.
Obscured segments of the margin of the optic
disk that correlate with visual field defects are a sign of AION.
Treatment:
Anterior ischemic optic neuropathy is nearly impossible to treat.Attempted methods include hemodilution (pentoxifylline infusions, acetyl-salicylic acid, and bloodletting depending on hematocrit levels) and systemic administration of steroids to control the edema. Diagnosis of the underlying cause is important; examination by an internist and Doppler ultrasound stud-ies of the carotid artery may be helpful. Underlying disorders such as diabetes mellitus or arterial hypertension should be treated.
Prognosis:
The prognosis is usually poor even where
therapy is initiatedearly. Isolated atrophy of the optic nerve will appear
within three weeks, complex atrophy of the optic nerve is less frequent but may
also be observed.
Arteritic Anterior Ischemic Optic Neuropathy
Definition
An acute disruption of the blood supply to the
optic disk due to inflammation of medium-sized and small arterial branches.
Epidemiology:
The annual incidence is approximately three
cases per100000. The disorder occurs almost exclusively after the age of 60.
Women are affected slightly more often than men, accounting for 55% of all
cases. Fifty per cent of all patients suffer from ocular involvement within a
few days up to approximately three months of the onset of the disorder.
Etiology:
Giant cell arteritis is a frequently bilateral
granulomatous vasculitisthat primarily affects the medium-sized and small
arteries. Common sites include the temporal arteries, ophthalmic artery, short
posterior ciliary arter-ies, central retinal artery, and the proximal portion
of the vertebral arteries, which may be affected in varying combinations.
Symptoms:
Patients reportsudden unilateral blindness or severe visualimpairment. Other
symptoms include headaches, painful scalp in the regionof the temporal
arteries, tenderness to palpation in the region of the temporal arteries, pain
while chewing (a characteristic sign), weight loss, reduced general health and exercise
tolerance. Patients may have a history of amauro-sis fugax or polymyalgia
rheumatica.
Diagnostic considerations:
The ophthalmoscopic
findings are the same asin arteriosclerotic AION (see Fig. 13.12a). Other findings include a signifi-cantly increased erythrocyte
sedimentation rate (precipitous sedimentation is the most important hematologic
finding), an increased level of C-reactive protein, leukocytosis, and
iron-deficiency anemia.
Erythrocyte sedimentation rate should be
measured in every patient presenting with anterior ischemic optic neuropathy.
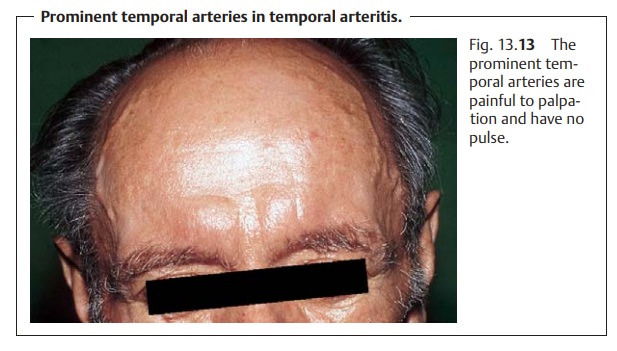
The temporal arteries are prominent (Fig. 13.13), painful to palpation, and have no pulse. The diagnosis is
confirmed by a biopsy of the temporal artery. Because of the segmental pattern
of vascular involvement, negative histologic findings cannot exclude giant cell
arteritis.
Giant cell arteritis should be considered in every patient presenting with anterior ischemic optic neuropathy.
Differential diagnosis:
Arteriosclerotic AION should be considered.
Treatment:
Immediatehigh-dosage systemic steroid therapy (initial doses upto 1000 mg
of intravenous prednisone) is indicated. Steroids are reduced as the
erythrocyte sedimentation rate decreases, C-reactive protein levels drop, and
clinical symptoms abate. However, a maintenance dose will be required for
several months. Vascular treatment such as pentoxifylline infusions may be
attempted.
High-dosage systemic steroid therapy (for
example 250 mg of intravenous prednisone) is indicated to protect the fellow
eye even if a giant cell arteritis is only suspected.
Prognosis:
The prognosis for the affected eye ispooreven where therapy isinitiated
early. Immediate steroid therapy is absolutely indicated because in
approximately 75% of all cases the fellow eye is affected within a few hours
and cerebral arteries may also be at risk.
Related Topics