Chapter: Medical Surgical Nursing: Respiratory Care Modalities
Oxygen Therapy - Noninvasive Respiratory Therapies
Noninvasive Respiratory Therapies
OXYGEN THERAPY
Oxygen
therapy is the administration of oxygen at a concentra-tion greater than that
found in the environmental atmosphere. At sea level, the concentration of
oxygen in room air is 21%. The goal of oxygen therapy is to provide adequate
transport of oxygen in the blood while decreasing the work of breathing and
reducing stress on the myocardium.
Oxygen
transport to the tissues depends on factors such as car-diac output, arterial
oxygen content, concentration of hemoglo-bin, and metabolic requirements. These
factors must be kept in mind when oxygen therapy is considered.
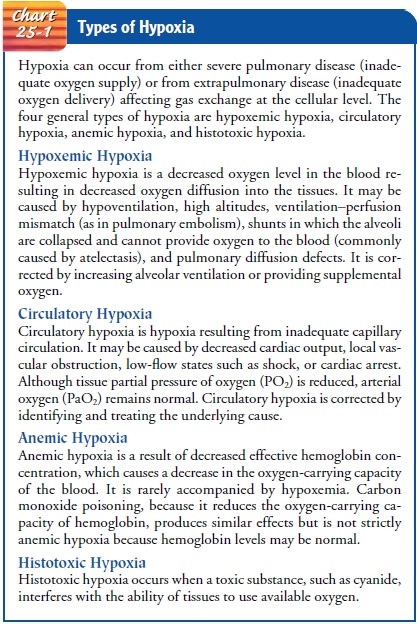
Indications
A
change in the patient’s respiratory rate or pattern may be one of the earliest
indicators of the need for oxygen therapy. The change in respiratory rate or
pattern may result from hypoxemia or hypoxia. Hypoxemia (a decrease in the arterial oxygen tension in the blood)
is manifested by changes in mental status (pro-gressing through impaired
judgment, agitation, disorientation, confusion, lethargy, and coma), dyspnea,
increase in blood pres-sure, changes in heart rate, dysrhythmias, central
cyanosis (late sign), diaphoresis, and cool extremities. Hypoxemia usually
leads to hypoxia, which is a
decrease in oxygen supply to the tissues. Hypoxia, if severe enough, can be
life-threatening.
The
signs and symptoms signaling the need for oxygen may depend on how suddenly
this need develops. With rapidly de-veloping hypoxia, changes occur in the
central nervous system because the higher neurologic centers are very sensitive
to oxy-gen deprivation. The clinical picture may resemble that of alco-hol
intoxication, with the patient exhibiting lack of coordination and impaired
judgment. Longstanding hypoxia (as seen in chronic obstructive pulmonary
disease [COPD] and chronic heart failure) may produce fatigue, drowsiness,
apathy, inatten-tiveness, and delayed reaction time. The need for oxygen is
as-sessed by arterial blood gas analysis and pulse oximetry as well as by
clinical evaluation. For more information about hypoxia, see Chart 25-1.
Cautions in Oxygen Therapy
As
with other medications, the nurse administers oxygen with caution and carefully
assesses its effects on each patient. Oxygen is a medication and except in
emergency situations is adminis-tered only when prescribed by a physician.
In general, patients with respiratory conditions are given oxygen therapy only to raise the arterial oxygen pressure (PaO2) back to the patient’s normal baseline, which may vary from 60 to 95 mm Hg.
In terms of the oxyhemoglobin dissociation curve, the
blood at these levels is 80% to 98% saturated with oxygen; higher inspired
oxygen flow (FiO2) values
add no further significant amounts of oxygen to the red blood cells or plasma.
Instead of help-ing, increased amounts of oxygen may produce toxic effects on
the lungs and central nervous system or may depress ventilation (see discussion
below).
It
is important to observe for subtle indicators of inadequate oxygenation when
oxygen is administered by any method. There-fore, the nurse assesses the
patient frequently for confusion, rest-lessness progressing to lethargy,
diaphoresis, pallor, tachycardia, tachypnea, and hypertension. Intermittent or
continuous pulse oximetry is used to monitor oxygen levels.
OXYGEN TOXICITY
Oxygen
toxicity may occur when too high a concentration of oxy-gen (greater than 50%)
is administered for an extended period (longer than 48 hours). It is caused by
overproduction of oxygen free radicals, which are byproducts of cell
metabolism. If oxygen toxicity is untreated, these radicals can severely damage
or kill cells. Antioxidants such as vitamin E, vitamin C, and beta-carotene may
help defend against oxygen free radicals (Scanlan, Wilkins & Stoller,
1999). The dietitian can adjust the patient’s diet so that it is rich in
antioxidants; supplements are also available for patients who have a decreased
appetite or who are unable to eat.
Signs
and symptoms of oxygen toxicity include substernal dis-comfort, paresthesias,
dyspnea, restlessness, fatigue, malaise, pro-gressive respiratory difficulty,
and alveolar infiltrates evident on chest x-rays.
Prevention
of oxygen toxicity is achieved by using oxygen only as prescribed. If high
concentrations of oxygen are necessary, it is important to minimize the
duration of administration and re-duce its concentration as soon as possible.
Often, positive end-expiratory pressure (PEEP)
or continuous positive airway pressure(CPAP) is used with oxygen therapy to
reverse or prevent micro-atelectasis, thus allowing a lower percentage of
oxygen to be used. The level of PEEP that allows the best oxygenation without
hemo-dynamic compromise is known as “best PEEP.”
SUPPRESSION OF VENTILATION
In
patients with COPD, the stimulus for respiration is a decrease in blood oxygen
rather than an elevation in carbon dioxide levels. Thus, administration of a
high concentration of oxygen removes the respiratory drive that has been
created largely by the patient’s chronic low oxygen tension. The resulting
decrease in alveolar ventilation can cause a progressive increase in arterial
carbon diox-ide pressure (PaCO2),
ultimately leading to the patient’s death from carbon dioxide narcosis and
acidosis. Oxygen-induced hypo-ventilation is prevented by administering oxygen
at low flow rates (1 to 2 L/min).
OTHER COMPLICATIONS
Because
oxygen supports combustion, there is always a danger of fire when it is used.
It is important to post “no smoking” signs when oxygen is in use. Oxygen
therapy equipment is also a po-tential source of bacterial cross-infection;
thus, the nurse changes the tubing according to infection control policy and
the type of oxygen delivery equipment.
Methods of Oxygen Administration
Oxygen
is dispensed from a cylinder or a piped-in system. A re-duction gauge is
necessary to reduce the pressure to a working level, and a flow meter regulates
the flow of oxygen in liters per minute. When oxygen is used at high flow
rates, it should be moistened by passing it through a humidification system to
prevent it from dry-ing the mucous membranes of the respiratory tract.
The
use of oxygen concentrators is another means of provid-ing varying amounts of
oxygen, especially in the home setting. These devices are relatively portable,
easy to operate, and cost-effective. However, they require more maintenance
than tank or liquid systems and probably cannot deliver oxygen flows in excess
of 4 L, which provides an FiO2 of about 36%.
Many
different oxygen devices are used, and all deliver oxy-gen if they are used as
prescribed and maintained correctly (Table 25-1). The amount of oxygen
delivered is expressed as a percentage concentration (eg, 70%). The appropriate
form of oxy-gen therapy is best determined by arterial blood gas levels, which
indicate the patient’s oxygenation status.
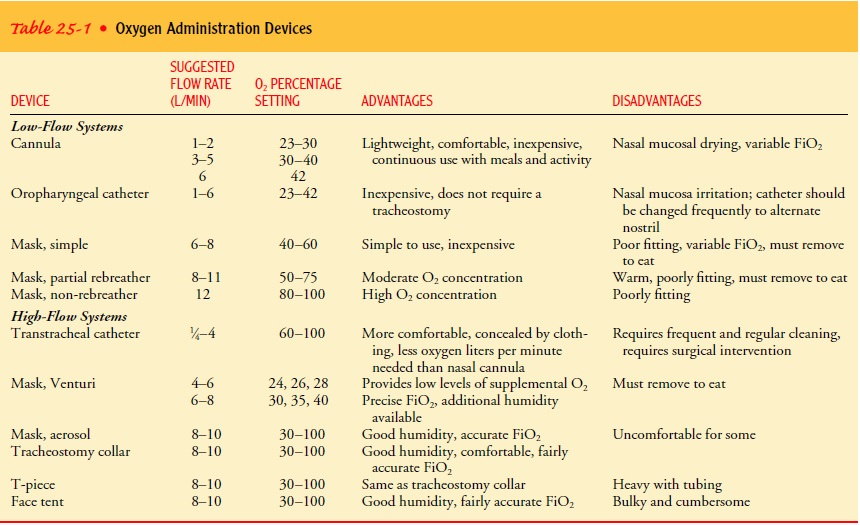
Oxygen delivery systems are classified as low-flow or high-flow delivery systems. Low-flow systems contribute partially to the in-spired gas the patient breathes. This means the patient breathes some room air along with the oxygen. These systems do not pro-vide a constant or known concentration of inspired oxygen. The amount of inspired oxygen changes as the patient’s breathing changes. Examples of low-flow systems include nasal cannula, oropharyngeal catheter, simple mask, and partial-rebreather and non-rebreather masks. High-flow systems provide the total amount of inspired air. A specific percentage of oxygen is delivered inde-pendent of the patient’s breathing. High-flow systems are indicated for patients who require a constant and precise amount of oxygen. Examples of such systems include transtracheal catheters, Venturi masks, aerosol masks, tracheostomy collars, T-piece, and face tents (Cairo & Philbeam, 1999; Scanlan, Wilkins & Stoller, 1999).
A
nasal cannula is used when the patient requires a low to medium concentration
of oxygen for which precise accuracy is not essential. This method is
relatively simple and allows the pa-tient to move about in bed, talk, cough,
and eat without inter-rupting oxygen flow. Flow rates in excess of 6 to 8 L/min
may lead to swallowing of air; this may cause irritation and drying of the
nasal and pharyngeal mucosa.
The
oropharyngeal catheter is rarely used but may be prescribed for short-term
therapy to administer low to moderate concentra-tions of oxygen. The catheter
should be changed every 8 hours, alternating nostrils to prevent infection and
nasal irritation.
When
oxygen is administered via cannula or catheter, the per-centage of oxygen
reaching the lungs varies with the depth and rate of respirations, particularly
if the nasal mucosa is swollen or if the patient is a mouth breather.
Oxygen
masks come in several forms. Each is used for differ-ent purposes (Fig. 25-1). Simple masks are used for low to
mod-erate concentrations of oxygen. The body of the mask itself gathers and
stores oxygen between breaths. The patient exhales directly through openings or
ports in the body of the mask. If oxygen flow ceases, the patient can draw air
in through these openings around the mask edges (Scanlan, Wilkins &
Stoller, 1999). Although widely used, these masks cannot be used for controlled
oxygen concentrations and must be adjusted for proper fit. They should not
press too tightly against the skin, be-cause this may cause a sense of
claustrophobia and skin break-down; adjustable elastic bands are provided to
ensure comfort and security.
Partial-rebreathing masks have
a reservoir bag that must re-main inflated during both inspiration and
expiration. The nurse should adjust the liter flow to ensure that the bag does
not col-lapse during inhalation. A higher concentration of oxygen can be
delivered because both the mask and bag serve as reservoirs for oxygen. Oxygen
enters the mask through small-bore tubing that connects at the junction of the
mask and bag. As the patient in-hales, gas is drawn from the mask, the bag, and
potentially from room air through the exhalation ports. As the patient exhales,
the first third of the exhalation fills the reservoir bag. This is mainly dead
space and does not participate in gas exchange in the lungs. Therefore, it has
a high oxygen concentration. The remainder of the exhaled gas is vented through
the exhalation ports. The actual percentage of oxygen delivered is influenced
by the patient’s ven-tilatory pattern (Cairo & Pilbeam, 1999).
Non-rebreathing masks are similar in design to partial-rebreathing masks except that they have two valves. The first valve is a one-way valve located between the reservoir bag and the base of the mask. The valve allows gas from the reservoir bag to enter the mask on inhalation and prevents gas in the mask from flowing back into the reservoir bag during exhalation. The second valve is a set of valves located at the exhalation ports. These one-way valves prevent room air from entering the mask during inhalation. They also allow the patient’s exhaled gases to exit the mask on exhalation (Cairo & Pilbeam, 1999). As with the partial-rebreathing mask, it is important to adjust the liter flow so that the reservoir bag does not completely collapse on inspiration. In theory, if the non-rebreather mask fits the patient snugly and both side exhalation ports have one-way valves, it is possible for the patient to receive 100% oxygen, making the non-rebreather a high-flow oxygen sys-tem. However, because it is difficult to get an exact fit from the mask on every patient, and some non-rebreather masks have only one one-way exhalation valve, it is nearly impossible to ensure 100% oxygen delivery, making it a low-flow oxygen system.
The
Venturi mask is the most reliable and
accurate method for delivering precise concentrations of oxygen through
noninvasive means. The mask is constructed in a way that allows a constant flow
of room air blended with a fixed flow of oxygen. It is used primarily for
patients with COPD because it can provide low lev-els of supplemental oxygen,
thus avoiding the risk of suppressing the hypoxic drive.
The
Venturi mask employs the Bernoulli principle of air en-trainment (trapping the
air like a vacuum), which provides a high air flow with controlled oxygen
enrichment. For each liter of oxy-gen that passes through a jet orifice, a
fixed proportion of room air will be entrained. A precise volume of oxygen can
be delivered by varying the size of the jet orifice and adjusting the flow of
oxy-gen. Excess gas leaves the mask through the two exhalation ports, carrying
with it the exhaled carbon dioxide. This method allows a constant oxygen
concentration to be inhaled regardless of the depth or rate of respiration.
The
mask should fit snugly enough to prevent oxygen from flowing into the patient’s
eyes. The nurse should check the pa-tient’s skin for irritation. It is
necessary to remove the mask so that the patient can eat, drink, and take
medications.
The
transtracheal oxygen catheter is
inserted directly into the trachea and is indicated for patients with chronic
oxygen therapy needs. These catheters are more comfortable, less dependent on
breathing patterns, and less obvious than other oxygen delivery methods.
Because no oxygen is lost into the surrounding envi-ronment, the patient
achieves adequate oxygenation at lower rates, making this method less expensive
and more efficient.
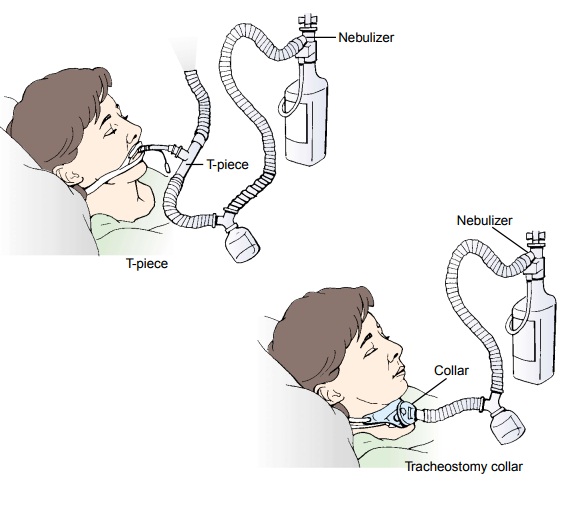
The
T-piece connects to the endotracheal
tube and is useful in weaning patients from mechanical ventilation (Fig. 25-2).
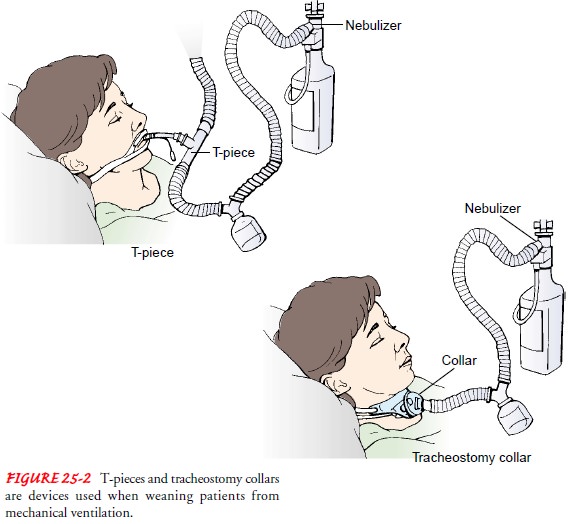
Other
oxygen devices include aerosol masks,
tracheostomy col-lars, and face
tents, all of which are used with aerosol devices (neb-ulizers) that can be
adjusted for oxygen concentrations from 27% to 100% (0.27 to 1.00). If the gas
mixture flow falls below pa-tient demand, room air is pulled in, diluting the
concentration. The aerosol mist must be available for the patient during the
en-tire inspiratory phase.
Although
most oxygen therapy is administered as continuous flow oxygen, new methods of
oxygen conservation are coming into use. Demand
oxygen delivery systems (DODS) interrupt the flow of oxygen during exhalation,
when the oxygen flow is otherwise mostly wasted. Several versions of DODS are
being researched for their effectiveness. Studies show that DODS models
conserve oxygen and maintain oxygen saturations better than continuous-flow
oxygen when the respiratory rate increases (Bliss, McCoy & Adams, 1999).
Hyperbaric
oxygen therapy is the administration of oxygen at pressures greater than one
atmosphere. As a result, the amount of oxygen dissolved in plasma is increased,
which raises oxygen lev-els in the tissues. It is administered through a small
(single patient use) or large (multiple patient use) cylinder chamber. During
therapy, the patient is placed in the chamber. Hyperbaric oxygen therapy is
used to treat conditions such as air embolism, carbon monoxide poisoning,
gangrene, tissue necrosis, and hemorrhage. Other uses for this therapy include
treatment for multiple sclero-sis, diabetic foot ulcers, closed head trauma,
and acute myocar-dial infarction. Research continues in the area of hyperbaric
oxygen use because of potential side effects, including ear trauma, central
nervous system disorders, and oxygen toxicity (Takezawa, 2000; Woodrow &
Roe, 2000).
Gerontologic Considerations
The respiratory system changes throughout the aging process, and it is important for nurses to be aware of these changes when assessing patients who are receiving oxygen therapy. As the respi-ratory muscles weaken and the large bronchi and alveoli become enlarged, the available surface area of the lungs decreases, result-ing in reduced ventilation and respiratory gas exchange. The number of functional cilia is also reduced, decreasing ciliary ac-tion and the cough reflex. As a result of osteoporosis and the cal-cification of the costal cartilages, chest wall compliance is decreased. Patients may display increased chest rigidity and respiratory rate and decreased PaO2 and lung expansion. Nurses should be aware that the older adult is at risk for aspiration and infection related to these changes. In addition, patient education regarding adequate nutrition is essential, because appropriate dietary intake can help to diminish the excess build-up of carbon dioxide and to main-tain optimal respiratory functioning (Abraham, Bottrell, Fulmer & Mezey, 1999; Eliopoulos, 2001).
Nursing Management
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
At times oxygen must be adminis-tered to the patient at home. The
nurse instructs the patient or family in the methods for administering oxygen
and informs the patient and family that oxygen is available in gas, liquid, and
con-centrated forms. The gas and liquid forms come in portable devices
so that the patient can leave home while receiving oxygen therapy. Humidity
must be provided while oxygen is used (except with portable devices) to
counteract the dry, irritating effects of compressed oxygen on the airway
(Chart 25-2).
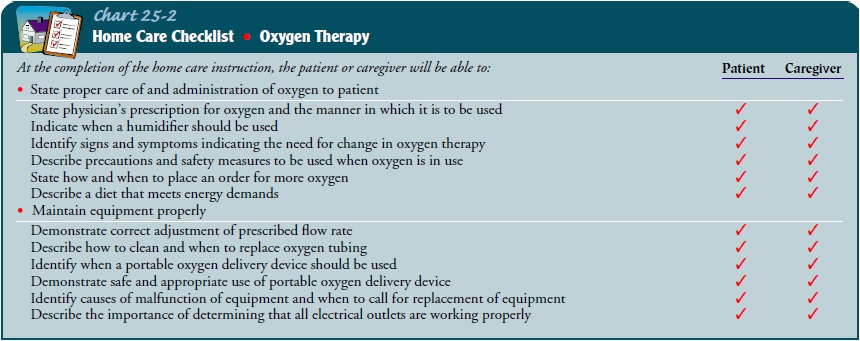
Continuing Care.
Home visits by a home health nurse or respi-ratory therapist may be arranged based on the patient’s status and needs. It is important to assess the patient’s home environment, the patient’s physical and psychological status, and the need for further teaching. The nurse reinforces the teaching points on how to use oxygen safely and effectively, including fire safety tips be-cause oxygen is flammable.
To maintain a consistent quality of care and to maximize the patient’s financial reimbursement for home
oxygen therapy, the nurse ensures that the physician’s pre-scription includes
the diagnosis, the prescribed oxygen flow, and conditions for use (eg,
continuous use, nighttime use only). Be-cause oxygen is a medication, the nurse
reminds the patient re-ceiving long-term oxygen therapy and family about the
importance of keeping follow-up appointments with the physician. The pa-tient
is instructed to see the physician every 6 months or more often, if indicated.
Blood gas measurements and laboratory tests are repeated annually, or more
often if the patient’s condition changes (Smith & Matti, 1999).
Related Topics