Chapter: Medical Surgical Nursing: Respiratory Care Modalities
Airway Management
Airway Management
Adequate
ventilation is dependent on free movement of air through the upper and lower
airways. In many disorders, the air-way becomes narrowed or blocked as a result
of disease, bron-choconstriction (narrowing of airway by contraction of muscle
fibers), a foreign body, or secretions. Maintaining a patent (open) airway is
achieved through meticulous airway management, whether in an emergency
situation such as airway obstruction or in long-term management, as in caring
for a patient with an endotracheal or a tracheostomy tube.
EMERGENCY MANAGEMENT OF UPPER AIRWAY OBSTRUCTION
Upper
airway obstruction has a variety of causes. Acute upper air-way obstruction may
be caused by food particles, vomitus, blood clots, or any other particle that
enters and obstructs the larynx or trachea. It also may occur from enlargement
of tissue in the wall of the airway, as in epiglottitis, laryngeal edema,
laryngeal carci-noma, or peritonsillar abscess, or from thick secretions.
Pressure on the walls of the airway, as occurs in retrosternal goiter,
en-larged mediastinal lymph nodes, hematoma around the upper airway, and
thoracic aneurysm, also may result in upper airway obstruction.
The
patient with an altered level of consciousness from any cause is at risk for
upper airway obstruction because of loss of the protective reflexes (cough and
swallowing) and the tone of the pharyngeal muscles, causing the tongue to fall
back and block the airway.
The
nurse makes the following rapid observations to assess for signs and symptoms
of upper airway obstruction:
1.
Inspection—Is the patient conscious?
Is there any inspira-tory effort? Does the chest rise symmetrically? Is there
use or retraction of accessory muscles? What is the skin color? Are there any
obvious signs of deformity or obstruction (trauma, food, teeth, vomitus)? Is
the trachea midline?
2.
Palpation—Do both sides of the chest
rise equally with in-spiration? Are there any specific areas of tenderness,
frac-ture, or subcutaneous emphysema (crepitus)?
3.
Auscultation—Is there any audible
air movement, stridor (inspiratory sound), or wheezing (expiratory sound)? Are
breath sounds present bilaterally in all lobes?
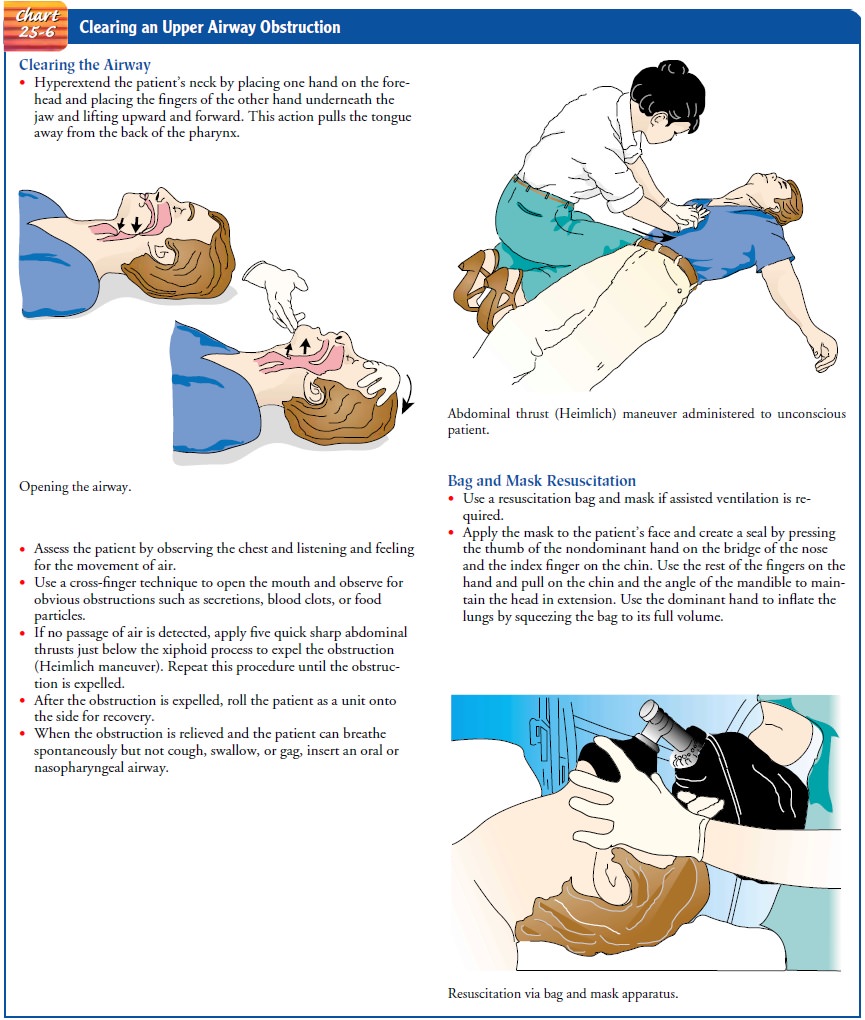
As
soon as an upper airway obstruction is identified, the nurse takes emergency
measures (Chart 25-6).
ENDOTRACHEAL INTUBATION
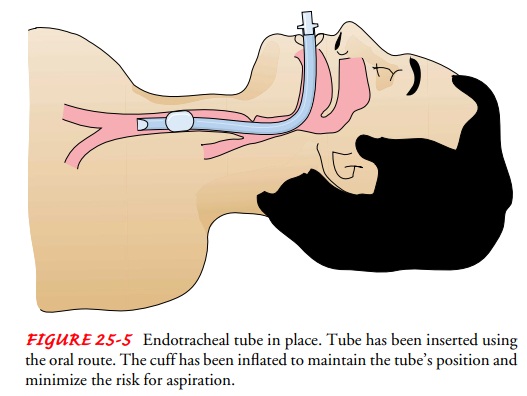
Endotracheal intubation involves
passing an endotracheal tubethrough the mouth or nose into the trachea (Fig.
25-5). Intuba-tion provides a patent airway when the patient is having
respira-tory distress that cannot be treated with simpler methods. It is the
method of choice in emergency care. Endotracheal intubation is a means of
providing an airway for patients who cannot maintain an adequate airway on
their own (eg, comatose patients or patients with upper airway obstruction),
for mechanical ventilation, and for suctioning secretions from the pulmonary
tree.
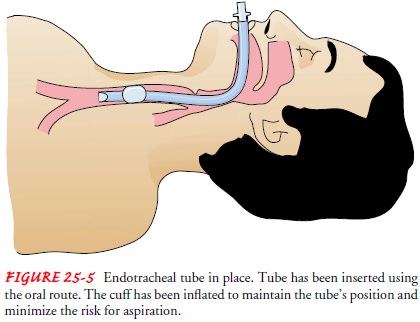
An
endotracheal tube usually is passed with the aid of a laryn-goscope by
specifically trained medical, nursing, or respiratory therapy personnel. Once
the tube is in-serted, a cuff around the tube is inflated to prevent air from
leaking around the outer part of the tube, to minimize the possibility of
subsequent aspiration, and to prevent movement of the tube.
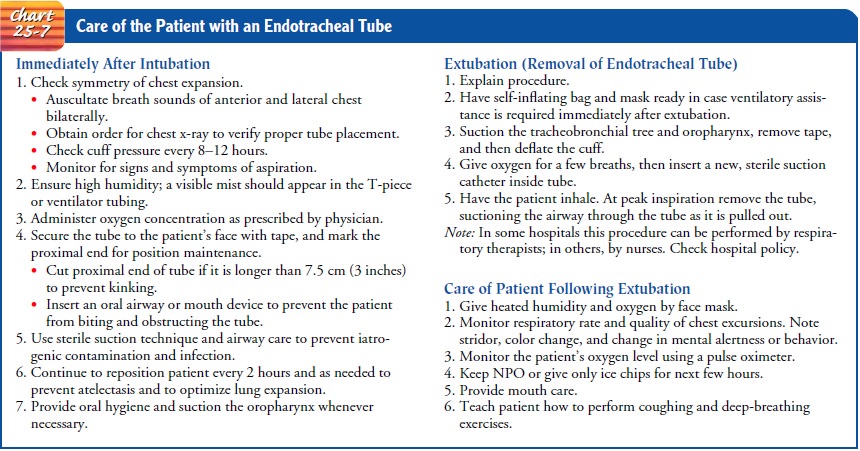
Nurses
should be aware that complications could occur from pressure in the cuff on the
tracheal wall. Cuff pressures should be checked with a calibrated aneroid manometer
device every 8 to 12 hours to maintain cuff pressure between 20 and 25 mm Hg.
High cuff pressure can cause tracheal bleeding, ischemia, and pressure
necrosis, while low cuff pressure can increase the risk of aspiration
pneumonia. Routine deflation of the cuff is not recommended due to the
increased risk of aspiration and hypoxia. The cuff is de-flated prior to
removing the endotracheal tube (St. John, 1999b).
Tracheobronchial
secretions are suctioned through the tube. Warmed, humidified oxygen should
always be introduced through the tube, whether the patient is breathing
spontaneously or is re-ceiving ventilatory support. Endotracheal intubation may
be used for no more than 3 weeks, by which time a tracheostomy must be
considered to decrease irritation of and trauma to the tracheal lin-ing, to
reduce the incidence of vocal cord paralysis (secondary to laryngeal nerve
damage), and to decrease the work of breathing. Chart 25-7 discusses the
nursing care of the patient with an en-dotracheal tube.
There
are several disadvantages of endotracheal and trache-ostomy tubes. First, the
tube causes discomfort. In addition, the cough reflex is depressed because
closure of the glottis is hindered. Secretions tend to become thicker because
the warming and hu-midifying effect of the upper respiratory tract has been
bypassed. The swallowing reflexes, composed of the glottic, pharyngeal, and
laryngeal reflexes, are depressed because of prolonged disuse and the
mechanical trauma of the endotracheal or tracheostomy tube, which puts the
patient at increased risk for aspiration. In addi-tion, ulceration and
stricture of the larynx or trachea may de-velop. Of great concern to the
patient is the inability to talk and to communicate needs.
Unintentional
or premature removal of the tube is a potentially life-threatening complication
of endotracheal intubation. Removal of the tube is a frequent problem in
intensive care units and occurs mainly during nursing care or by the patient.
It is important for nurses to instruct patients and family members about the
purpose of the tube and the dangers of removing it. Baseline and ongoing
assessment of the patient and equipment ensures effective care. Providing
comfort measures, including opioid analgesia and seda-tion, can improve the patient’s
tolerance of the endotracheal tube.
To prevent tube removal by the patient, the nurse can use the following strategies: explain to the patient and family the purpose of the tube, distract the patient through one-to-one interaction with the nurse and family or with television, and maintain com-fort measures. As a last resort, soft wrist restraints may be used, according to agency policy.
Studies have shown that the most effective way to prevent tube removal by the patient is through the use of soft wrist restraints (Happ, 2000). However, discretion and caution must always be used before applying any restraint. If the patient cannot move the arms and hands to the endotracheal tube, restraints would not be needed. If the patient is alert, oriented, able to follow directions, and cooperative to the point that it is highly unlikely that he or she will remove the endotracheal tube, restraints are not needed. On the other hand, if the nurse determines there is a risk that the patient may try to remove the tube, soft wrist restraints are appropriate with a physician’s order (check agency policy). Close monitoring of the patient remains essential to ensure safety and prevent harm.
TRACHEOSTOMY
A
tracheotomy is a surgical procedure
in which an opening is made into the trachea. The indwelling tube inserted into
the tra-chea is called a tracheostomy
tube. A tracheostomy may be either temporary or permanent.
A
tracheostomy is used to bypass an upper airway obstruction, to allow removal of
tracheobronchial secretions, to permit the long-term use of mechanical
ventilation, to prevent aspiration of oral or gastric secretions in the
unconscious or paralyzed patient (by closing off the trachea from the
esophagus), and to replace an endotracheal tube. There are many disease
processes and emer-gency conditions that make a tracheostomy necessary.
Procedure
The
surgical procedure is usually performed in the operating room or in an
intensive care unit, where the patient’s ventilation can be well controlled and
optimal aseptic technique can be maintained.A surgical opening is made in the
second and third tracheal rings. After the trachea is exposed, a cuffed
tracheostomy tube of an ap-propriate size is inserted. The cuff is an
inflatable attachment to the tracheostomy tube that is designed to occlude the
space be-tween the trachea walls and the tube to permit effective me-chanical
ventilation and to minimize the risk of aspiration.
The
tracheostomy tube is held in place by tapes fastened around the patient’s neck.
Usually a square of sterile gauze is placed between the tube and the skin to
absorb drainage and pre-vent infection.
Complications
Complications
may occur early or late in the course of tra-cheostomy tube management. They
may even occur years after the tube has been removed. Early complications
include bleed-ing, pneumothorax, air embolism, aspiration, subcutaneous or
mediastinal emphysema, recurrent laryngeal nerve damage, and posterior tracheal
wall penetration. Long-term complications in-clude airway obstruction from
accumulation of secretions or pro-trusion of the cuff over the opening of the
tube, infection, rupture of the innominate artery, dysphagia, tracheoesophageal
fistula, tracheal dilation, and tracheal ischemia and necrosis. Tracheal
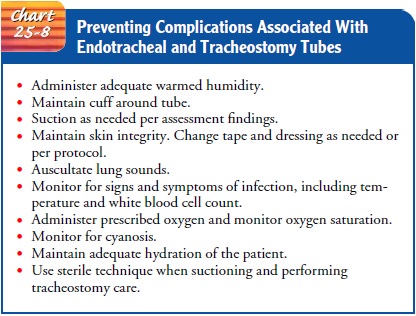
stenosis may develop after the tube is removed. Chart 25-8 out-lines measures
nurses can take to prevent complications.
Postoperative Nursing Management
The
patient requires continuous monitoring and assessment. The newly made opening
must be kept patent by proper suctioning of secretions. After the vital signs
are stable, the patient is placed in a semi-Fowler’s position to facilitate
ventilation, promote drainage, minimize edema, and prevent strain on the suture
lines. Analgesia and sedative agents must be administered with caution because
of the risk of suppressing the cough reflex.
Major objectives of nursing care are to alleviate the patient’s apprehension and to provide an effective means of communication.
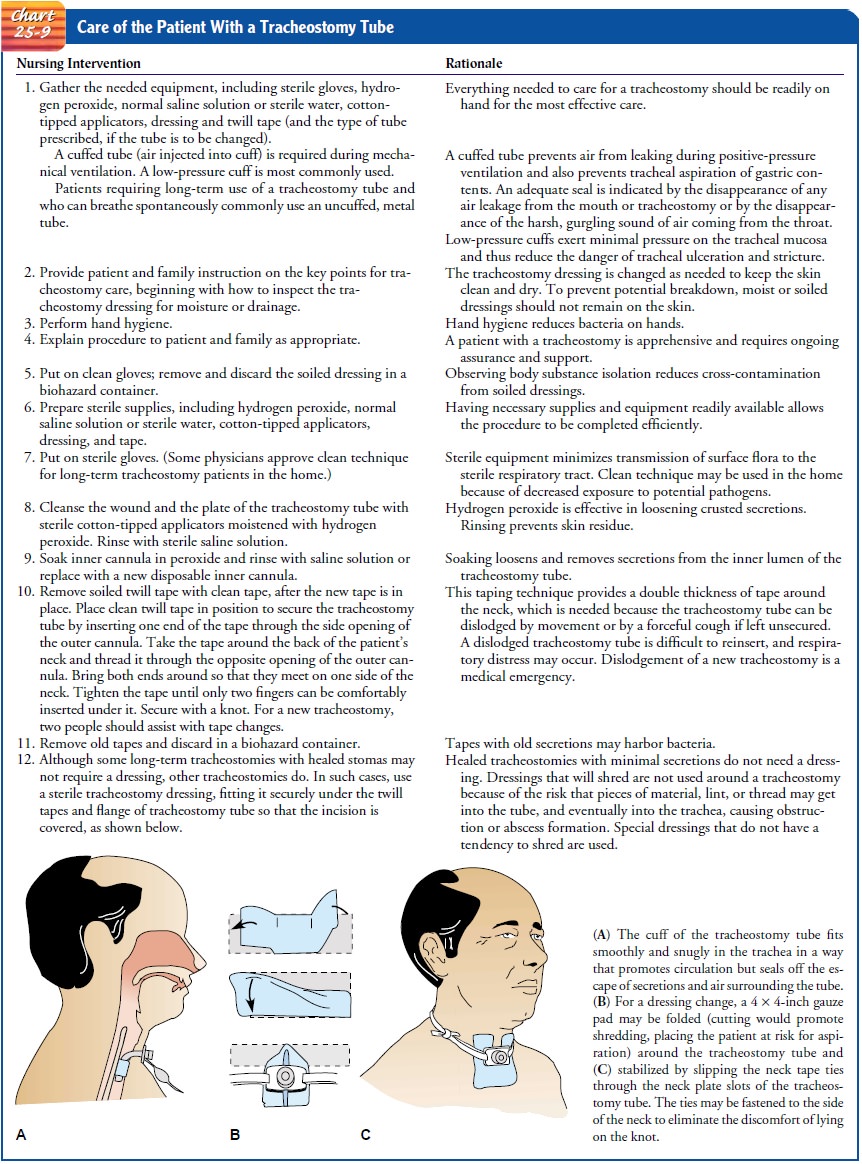
The nurse keeps paper and pencil or a Magic Slate and the call light within the
patient’s reach to ensure a means of commu-nication. The care of the patient
with a tracheostomy tube is summarized in Chart 25-9.
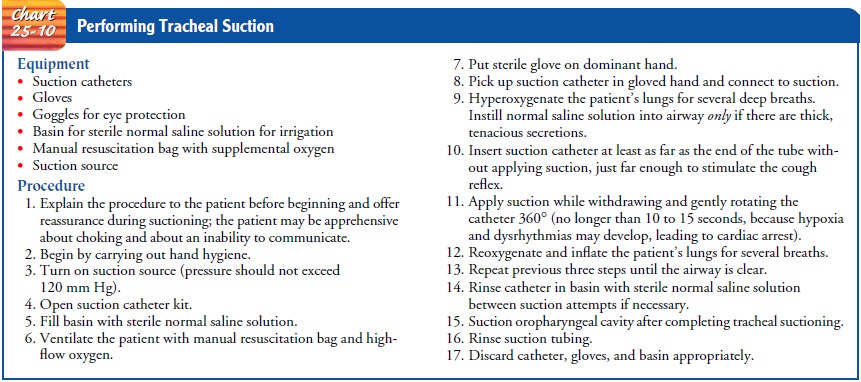
SUCTIONING THE TRACHEAL TUBE (TRACHEOSTOMY OR ENDOTRACHEAL TUBE)
When
a tracheostomy or endotracheal tube is in place, it is usu-ally necessary to
suction the patient’s secretions because of the de-creased effectiveness of the
cough mechanism. Tracheal suctioning is performed when adventitious breath
sounds are detected or whenever secretions are obviously present. Unnecessary
suction-ing can initiate bronchospasm and cause mechanical trauma to the
tracheal mucosa.
All
equipment that comes into direct contact with the pa-tient’s lower airway must
be sterile to prevent overwhelming pul-monary and systemic infections. The
procedure for suctioning a tracheostomy is presented in Chart 25-10. In
mechanically ven-tilated patients, an in-line suction catheter may be used to
allow rapid suction when needed and to minimize cross-contamination of airborne
pathogens. An in-line suction device allows the pa-tient to be suctioned
without being disconnected from the venti-lator circuit.
MANAGING THE CUFF
As
a general rule, the cuff on an endotracheal or tracheostomy tube should be
inflated. The pressure within the cuff should be the lowest possible that
allows delivery of adequate tidal volumes and prevents pulmonary aspiration.
Usually the pressure is main-tained at less than 25 cm H2O
to prevent injury and at more than 20 cm H2O
to prevent aspiration. Cuff pressure must be moni-tored at least every 8 hours
by attaching a hand-held pressure gauge to the pilot balloon of the tube or by
using the minimal leak volume or minimal occlusion volume technique. With
long-term intubation, higher pressures may be needed to maintain an adequate
seal.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care. If the patient is at home with a tra-cheostomy, the nurse
instructs the patient and family about its daily care as well as measures to
take in an emergency. The nurse also makes sure the patient and family are
aware of community contacts for education and support needs. It is important
for the nurse to teach the patient and family strategies to prevent
infec-tion when performing tracheostomy care (McConnell, 2000).
Related Topics