Chapter: Medical Surgical Nursing: Respiratory Care Modalities
Chest Physiotherapy - Noninvasive Respiratory Therapies
CHEST PHYSIOTHERAPY
Chest physiotherapy (CPT)
includes postural drainage, chest
percussion and vibration, and
breathing exercises/breathing re-training. In addition, teaching the patient
effective coughing technique is an important part of chest physiotherapy. The
goals of chest physiotherapy are to remove bronchial secretions, im-prove
ventilation, and increase the efficiency of the respiratory muscles.
Postural Drainage (Segmented Bronchial Drainage)
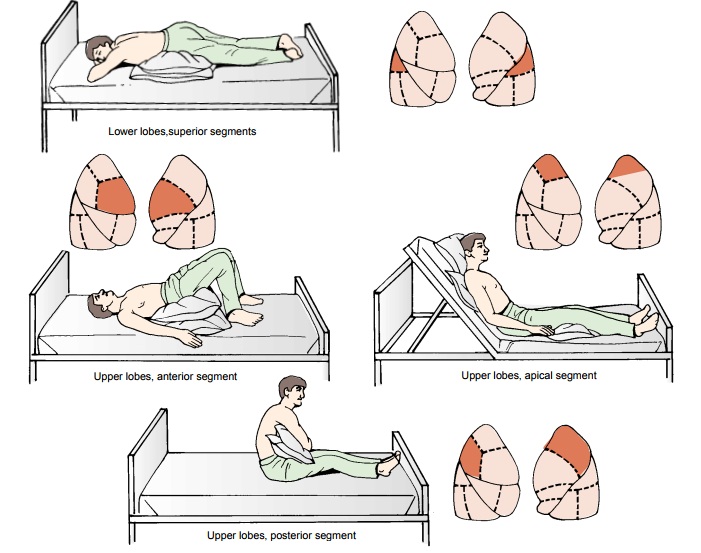
Postural
drainage uses specific positions that allow the force of gravity to assist in
the removal of bronchial secretions. The se-cretions drain from the affected
bronchioles into the bronchi and trachea and are removed by coughing or
suctioning. Postural drainage is used to prevent or relieve bronchial
obstruction caused by accumulation of secretions.
Because
the patient usually sits in an upright position, secre-tions are likely to
accumulate in the lower parts of the lungs. With postural drainage, different
positions (Fig. 25-3) are used so that the force of gravity helps to move secretions
from the smaller bronchial airways to the main bronchi and trachea. The
secre-tions then are removed by coughing. The nurse should instruct the patient
to inhale bronchodilators and mucolytic agents, if pre-scribed, before postural
drainage because these medications im-prove bronchial tree drainage.
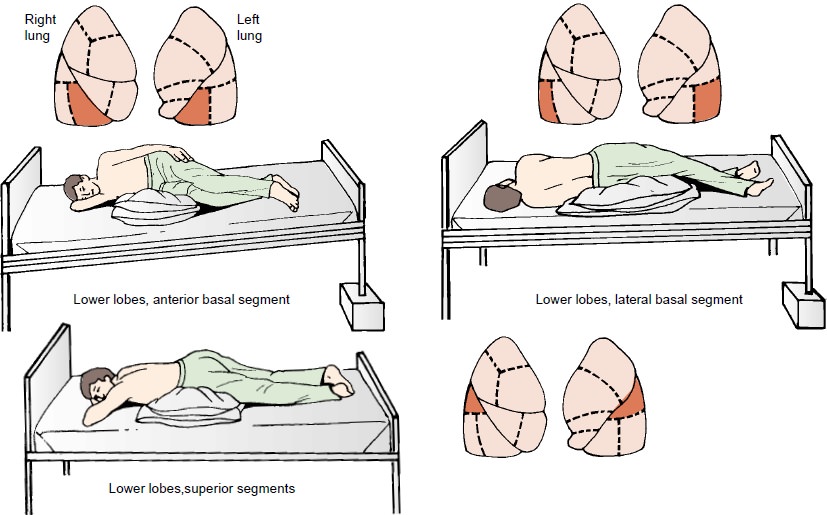
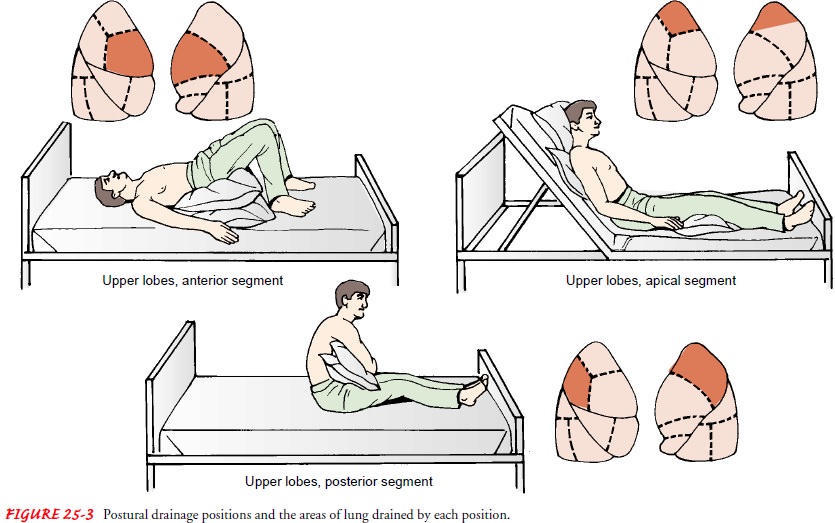
Postural
drainage exercises can be directed at any of the seg-ments of the lungs. The
lower and middle lobe bronchi drain more effectively when the head is down; the
upper lobe bronchi drain more effectively when the head is up. Frequently, five
po-sitions are used, one for drainage of each lobe: head down, prone, right and
left lateral, and sitting upright.
Nursing Management
The
nurse should be aware of the patient’s diagnosis as well as the lung lobes or
segments involved, the cardiac status, and any struc-tural deformities of the
chest wall and spine. Auscultating the chest before and after the procedure
helps to identify the areas needing drainage and to assess the effectiveness of
treatment. The nurse teaches family members who will be assisting the patient
at home to evaluate breath sounds before and after treatment. The nurse
explores strategies that will enable the patient to assume the in-dicated
positions at home. This may require the creative use of objects readily
available at home, such as pillows, cushions, or card-board boxes.
Postural
drainage is usually performed two to four times daily, before meals (to prevent
nausea, vomiting, and aspiration) and at bedtime. Prescribed bronchodilators,
water, or saline may be neb-ulized and inhaled before postural drainage to
dilate the bron-chioles, reduce bronchospasm, decrease the thickness of mucus
and sputum, and combat edema of the bronchial walls. The rec-ommended sequence
of positioning is as follows: positions to drain the lower lobes first, then
positions to drain the upper lobes.
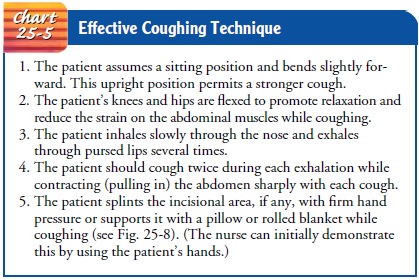
The
nurse makes the patient as comfortable as possible in each position and
provides an emesis basin, sputum cup, and paper tis-sues. The nurse instructs
the patient to remain in each position for 10 to 15 minutes and to breathe in
slowly through the nose and then breathe out slowly through pursed lips to help
keep the air-ways open so that secretions can drain while in each position. If
a position cannot be tolerated, the nurse helps the patient to assume a
modified position. When the patient changes position, the nurse explains how to
cough and remove secretions (Chart 25-5).
If the patient cannot cough, the nurse may need to suction the secretions mechanically. It also may be necessary to use chest per-cussion and vibration to loosen bronchial secretions and mucus plugs that adhere to the bronchioles and bronchi and to propel sputum in the direction of gravity drainage (see “Chest Percus-sion and Vibration,” below). If suctioning is required at home, the nurse instructs caregivers in safe suctioning technique and care of the suctioning equipment.
After
the procedure, the nurse notes the amount, color, vis-cosity, and character of
the expelled sputum. It is important to evaluate the patient’s skin color and
pulse the first few times the procedure is performed. It may be necessary to
administer oxy-gen during postural drainage.
If
the sputum is foul-smelling, it is important to perform pos-tural drainage in a
room away from other patients and/or family members and to use deodorizers
unless contraindicated. Deodor-izers delivered in aerosol sprays can cause
bronchospasm and irri-tation to the patient with a respiratory disorder and
should be used cautiously (Zang & Allender, 1999). After the procedure, the
pa-tient may find it refreshing to brush the teeth and use a mouth-wash before
resting.
Chest Percussion and Vibration
Thick
secretions that are difficult to cough up may be loosened by tapping
(percussing) and vibrating the chest. Chest percussion and vibration help to
dislodge mucus adhering to the bronchioles and bronchi.
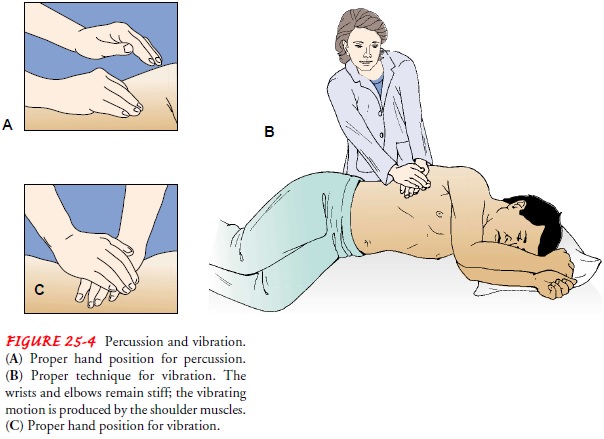
Percussion
is carried out by cupping the hands and lightly strik-ing the chest wall in a
rhythmic fashion over the lung segment to be drained. The wrists are
alternately flexed and extended so that the chest is cupped or clapped in a
painless manner (Fig. 25-4). A soft cloth or towel may be placed over the
segment of the chest that is being cupped to prevent skin irritation and
redness from direct contact. Percussion, alternating with vibration, is
performed for 3 to 5 minutes for each position. The patient uses diaphrag-matic
breathing during this procedure to promote relaxation (see “Breathing
Retraining,” below). As a precaution, percussion over chest drainage tubes, the
sternum, spine, liver, kidneys, spleen, or breasts (in women) is avoided.
Percussion is performed cautiously in the elderly because of their increased
incidence of osteoporo-sis and risk of rib fracture.
Vibration
is the technique of applying manual compression and tremor to the chest wall
during the exhalation phase of res-piration (see Fig. 25-4). This helps to
increase the velocity of the air expired from the small airways, thus freeing
the mucus. After three or four vibrations, the patient is encouraged to cough,
using the abdominal muscles. (Contracting the abdominal muscles in-creases the
effectiveness of the cough.)
A
scheduled program of coughing and clearing sputum, to-gether with hydration,
reduces the amount of sputum in most pa-tients. The number of times the
percussion and vibration cycle is repeated depends on the patient’s tolerance
and clinical response. It is important to evaluate breath sounds before and
after the procedures.
Nursing Management
When
performing chest physiotherapy, the nurse ensures that the patient is
comfortable, is not wearing restrictive clothing, and has not just eaten. The uppermost
areas of the lung are treated first. The nurse gives medication for pain, as
prescribed, before per-cussion and vibration and splints any incision and
provides pil-lows for support as needed. The positions are varied, but focus is
placed on the affected areas. On completion of the treatment, the nurse assists
the patient to assume a comfortable position.
The nurse must stop treatment if any of the following occur: increased pain, increased shortness of breath, weakness, light-headedness, or hemoptysis. Therapy is indicated until the patient has normal respirations, can mobilize secretions, and has normal breath sounds, and when the chest x-ray findings are normal.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Chest physiotherapy is frequentlyindicated at home for patients
with COPD, bronchiectasis, and cystic fibrosis. The techniques are the same as
described above, but gravity drainage is achieved by placing the hips over a
box, a stack of magazines, or pillows (unless a hospital bed is available). The
nurse instructs the patient and family in the positions and techniques of
percussion and vibration so that therapy can be continued in the home. In
addition, the nurse instructs the pa-tient to maintain an adequate fluid intake
and air humidity to prevent secretions from becoming thick and tenacious. It
also is important to teach the patient to recognize early signs of infec-tion,
such as fever and a change in the color or character of spu-tum. Resting 5 to
10 minutes in each postural drainage position before chest physiotherapy
maximizes the amount of secretions obtained.
Continuing Care.
Chest
physical therapy may be carried out dur-ing visits by a home care nurse. The
nurse also assesses the pa-tient’s physical status, understanding of the
treatment plan, and compliance with recommended therapy, as well as the
effective-ness of therapy. It is important to reinforce patient and family
teaching during these visits. The nurse reports to the patient’s physician any
deterioration in the patient’s physical status and in-ability to clear
secretions.
Breathing Retraining
Breathing
retraining consists of exercises and breathing practices designed to achieve
more efficient and controlled ventilation and to decrease the work of
breathing. Breathing retraining is espe-cially indicated in patients with COPD
and dyspnea. These ex-ercises promote maximal alveolar inflation and muscle
relaxation, relieve anxiety, eliminate ineffective, uncoordinated patterns of
respiratory muscle activity, slow the respiratory rate, and decrease the work
of breathing. Slow, relaxed, and rhythmic breathing also helps to control the
anxiety that occurs with dyspnea. Specific breathing exercises include
diaphragmatic and pursed-lip breath-ing (see Chart 25-3).
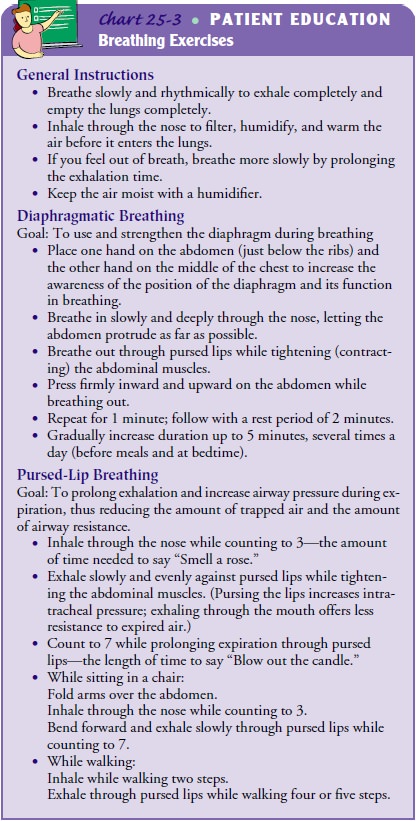
The
goal of diaphragmatic breathing is to use and strengthen the diaphragm during
breathing. Diaphragmatic breathing can become automatic with sufficient
practice and concentration. Pursed-lip breathing, which improves oxygen
transport, helps to induce a slow, deep breathing pattern and assists the
patient to control breathing, even during periods of stress. This type of
breathing helps prevent airway collapse secondary to loss of lung elasticity in
emphysema. The goal of pursed-lip breathing is to train the muscles of
expiration to prolong exhalation and increase airway pressure during
expiration, thus lessening the amount of airway trapping and resistance. The
nurse instructs the patient in diaphragmatic breathing and pursed-lip
breathing, as described earlier in Chart 25-3. Breathing exercises may be
practiced in sev-eral positions because air distribution and pulmonary
circulation vary with the position of the chest. Many patients require
addi-tional oxygen, using a low-flow method, while performing breath-ing
exercises. Emphysema-like changes in the lung occur as part of the natural
aging process of the lung; therefore, breathing ex-ercises are appropriate for
all elderly patients who are hospitalized and elderly patients in any setting
who are sedentary, even with-out primary lung disease.
Nursing Management
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The nurse instructs the patient tobreathe slowly and rhythmically
in a relaxed manner and to ex-hale completely to empty the lungs. The patient
is instructed always to inhale through the nose because this filters,
humidifies, and warms the air. If short of breath, the patient should
concen-trate on breathing slowly and rhythmically. To avoid initiating a cycle
of increasing shortness of breath and panic, it is often help-ful to instruct
the patient to concentrate on prolonging the length of exhalation rather than
merely slowing the rate of breathing. Minimizing the amount of dust or particles
in the air and pro-viding adequate humidification may also make it easier for
the pa-tient to breathe. Strategies to decrease dust or particles in the air
include removing drapes or upholstered furniture, using air fil-ters, and
washing floors and dusting and vacuuming frequently.
The
nurse instructs the patient that an adequate dietary intake promotes gas
exchange and increases energy levels. It is important to provide adequate
nutrition without overfeeding patients. Nurses should teach patients to consume
small, frequent meals and snacks. Having ready-prepared meals and favorite
foods available helps encourage nutrient consumption. Gas-producing foods such
as beans, legumes, broccoli, cabbage, and Brussels sprouts should be avoided to
prevent gastric distress. Because many of these patients
lack
the energy to eat, they should be taught to rest before and after meals to
conserve energy (Lutz & Przytulski, 2001).
Related Topics