Chapter: Medical Surgical Nursing: Respiratory Care Modalities
Nursing Process: The Patient Undergoing Thoracic Surgery
NURSING PROCESS: THE PATIENT UNDERGOING THORACIC SURGERY
Postoperative Assessment
The
nurse monitors the heart rate and rhythm by auscultation and electrocardiography
because episodes of major dysrhythmias are common after thoracic and cardiac
surgery. In the immediate postoperative period, an arterial line may be
maintained to allow frequent monitoring of arterial blood gases, serum
electrolytes, hemoglobin and hematocrit values, and arterial pressure. Central
venous pressure may be monitored to detect early signs of fluid volume
disturbances. Central venous pressure monitoring devices are being used less
frequently and for shorter periods of time than in the past. Early extubation
from mechanical ventilation can also lead to earlier removal of arterial lines
(Zevola & Maier, 1999). Another important component of postoperative
assessment is to note the results of the preoperative evaluation of the
patient’s lung reserve by pulmonary function testing. A preoperative FEV1
of more than 2 L or more than 70% of predicted value indicates a good lung
reserve. Patients who have a postoperative predicted FEV1
of less than 40% of predicted value have a higher incidence of morbidity and
mortality (Scanlan, Wilkins & Stoller, 1999). This results in decreased
tidal volumes, placing the patient at risk for respiratory failure.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data, the patient’s major postoperative nursing diagnoses may
include:
·
Impaired gas exchange related to
lung impairment and surgery
·
Ineffective airway clearance related
to lung impairment, anesthesia, and pain
·
Acute pain related to incision,
drainage tubes, and the sur-gical procedure
·
Impaired physical mobility of the
upper extremities related to thoracic surgery
·
Risk for imbalanced fluid volume
related to the surgical pro-cedure
·
Imbalanced nutrition, less than body
requirements related to dyspnea and anorexia
·
Deficient knowledge about self-care
procedures at home
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on assessment data, potential complications may include:
·
Respiratory distress
·
Dysrhythmias
·
Atelectasis, pneumothorax, and
bronchopleural fistula
·
Blood loss and hemorrhage
·
Pulmonary edema
Planning and Goals
The
major goals for the patient may include improvement of gas exchange and
breathing, improvement of airway clearance, relief of pain and discomfort,
increased arm and shoulder mobility, main-tenance of adequate fluid volume and
nutritional status, under-standing of self-care procedures, and absence of
complications.
Nursing Interventions
IMPROVING GAS EXCHANGE AND BREATHING
Gas
exchange is determined by evaluating oxygenation and ven-tilation. In the
immediate postoperative period, this is achieved by measuring vital signs
(blood pressure, pulse, and respirations) at least every 15 minutes for the
first 1 to 2 hours, then less fre-quently as the patient’s condition
stabilizes.
Pulse
oximetry is used for continuous monitoring of the ade-quacy of oxygenation. It
is important to draw blood for arterial blood gas measurements early in the
postoperative period to es-tablish a baseline to assess the adequacy of
oxygenation and ven-tilation and the possible retention of CO2.
The frequency with which postoperative arterial blood gases are measured
depends on whether the patient is mechanically ventilated or exhibits signs of
respiratory distress; these measurements can help determine ap-propriate
therapy. It also is common practice for patients to have an arterial line in
place to obtain blood for blood gas measure-ments and to monitor blood pressure
closely. Hemodynamic monitoring may be used to assess hemodynamic stability.
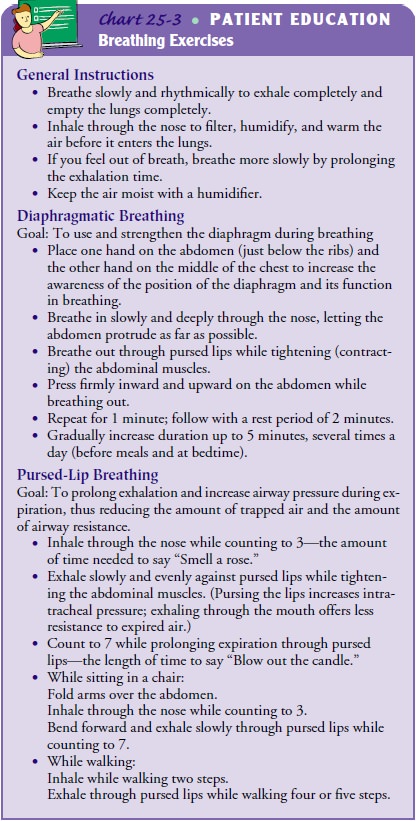
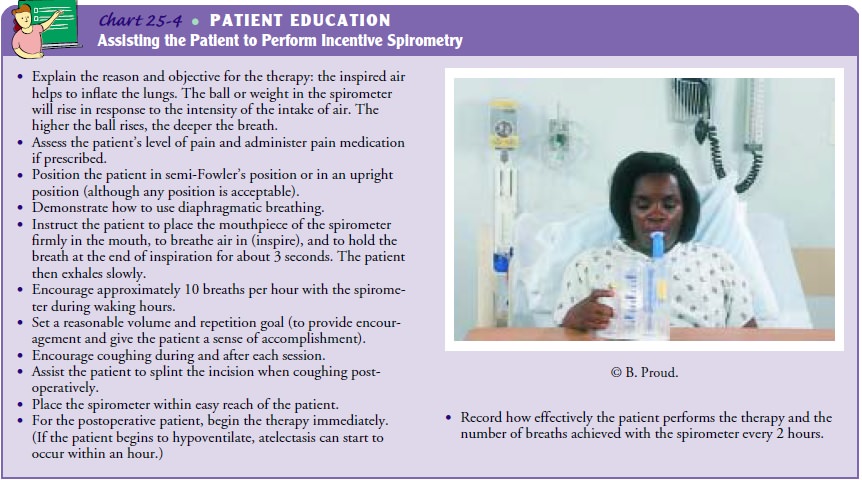
Breathing
techniques, such as diaphragmatic and pursed-lip breathing, that were taught
before surgery should be performed by the patient every 2 hours to expand the
alveoli and prevent at-electasis. Another technique to improve ventilation is
sustained maximal inspiration therapy or incentive spirometry. This tech-nique
promotes lung inflation, improves the cough mechanism, and allows early
assessment of acute pulmonary changes. (See Charts 25-3 and 25-4 for more
information.)
Positioning
also improves breathing. When the patient is ori-ented and blood pressure is
stabilized, the head of the bed is elevated 30 to 40 degrees during the
immediate postoperative period. This facilitates ventilation, promotes chest
drainage from the lower chest tube, and helps residual air to rise in the upper
portion of the pleural space, where it can be removed through the upper chest
tube.
The
nurse should consult with the surgeon about patient po-sitioning. There is
controversy regarding the best side-lying posi-tion. In general, the patient
should be positioned from back to side frequently and moved from horizontal to
semi-upright posi-tion as soon as tolerated. Most commonly, the patient is
in-structed to lie on the operative side. However, the patient with unilateral
lung pathology may not be able to turn well onto that side because of pain. In
addition, positioning the patient with the “good lung” (the nonoperated lung)
down allows a better match of ventilation and perfusion and therefore may
actually improve oxygenation. The patient’s position is changed from horizontal
to semi-upright as soon as possible, because remaining in one po-sition tends
to promote the retention of secretions in the depen-dent portion of the lungs.
After a pneumonectomy, the operated side should be dependent so that fluid in
the pleural space re-mains below the level of the bronchial stump, and the
other lung can fully expand.
The
procedure for turning the patient is as follows:
·
Instruct the patient to bend the
knees and use the feet to push.
·
Have the patient shift hips and
shoulders to the opposite side of the bed while pushing with the feet.
·
Bring the patient’s arm over the
chest, pointing it in the di-rection toward which the patient is being turned.
Have the patient grasp the side rail with the hand.
·
Turn the patient in log-roll fashion
to prevent twisting at the waist and pain from possible pulling on the
incision.
IMPROVING AIRWAY CLEARANCE
Retained
secretions are a threat to the thoracotomy patient after surgery. Trauma to the
tracheobronchial tree during surgery, di-minished lung ventilation, and
diminished cough reflex all result in the accumulation of excessive secretions.
If the secretions are retained, airway obstruction occurs. This, in turn,
causes the air in the alveoli distal to the obstruction to become absorbed and
the affected portion of the lung to collapse. Atelectasis, pneumo-nia, and
respiratory failure may result.
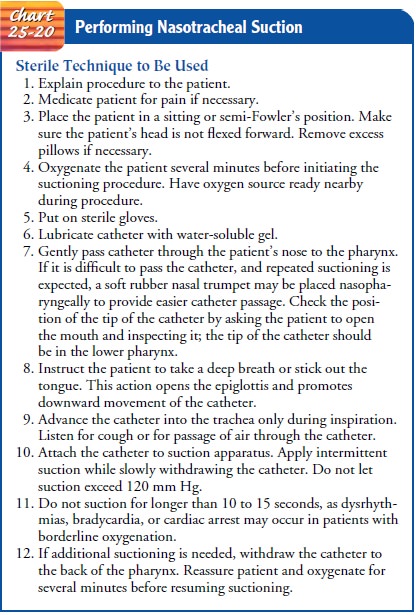
Several
techniques are used to maintain a patent airway. First, secretions are
suctioned from the tracheobronchial tree before the endotracheal tube is
discontinued. Secretions continue to be re-moved by suctioning until the
patient can cough up secretions ef-fectively. Nasotracheal suctioning may be
needed to stimulate a deep cough and aspirate secretions that the patient
cannot cough up. However, it should be used only after other methods to raise
secretions have been unsuccessful (Chart 25-20).
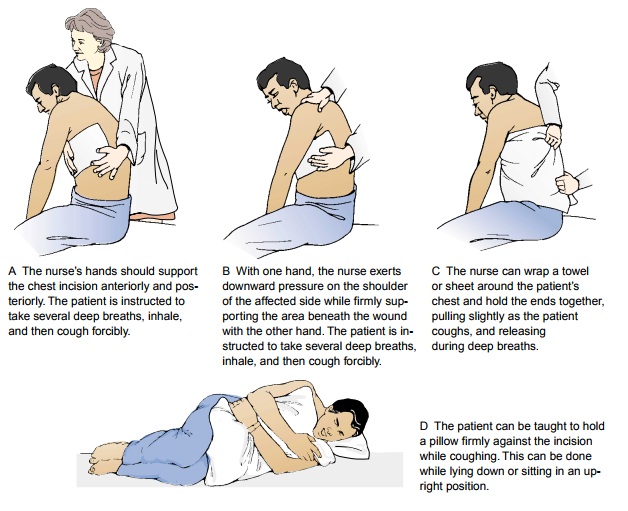
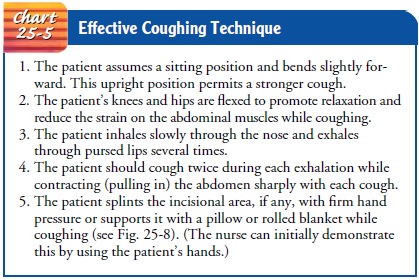
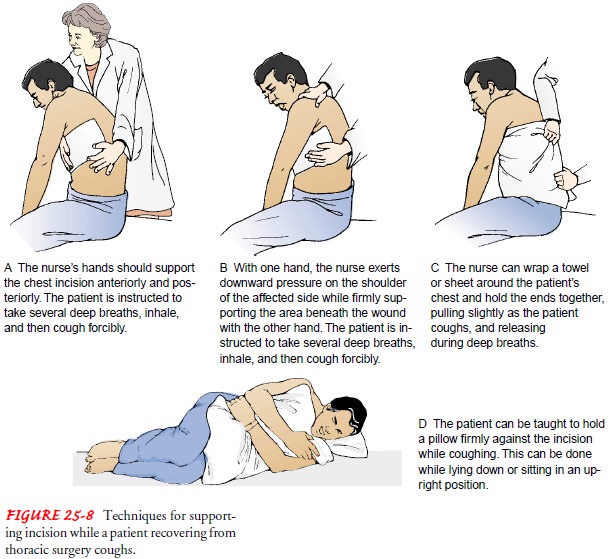
Coughing
technique is another measure used in maintaining a patent airway. The patient
is encouraged to cough effectively; in-effective coughing results in exhaustion
and retention of secretions (see Chart 25-5). To be effective, the cough must
be low-pitched, deep, and controlled. Because it is difficult to cough in a
supine position, the patient is helped to a sitting position on the edge of the
bed, with the feet resting on a chair. The patient should cough at least every
hour during the first 24 hours and when necessary thereafter. If audible
crackles are present, it may be necessary to use chest percussion with the
cough routine until the lungs are clear. Aerosol therapy is helpful in
humidifying and mobilizing secretions so that they can easily be cleared with
coughing. To min-imize incisional pain during coughing, the nurse supports the
in-cision or encourages the patient to do so (Fig. 25-8).
After
helping the patient to cough, the nurse should listen to both lungs, anteriorly
and posteriorly, to determine whether there are any changes in breath sounds.
Diminished breath sounds may indicate collapsed or hypoventilated alveoli.
Chest
physiotherapy is the final technique for maintaining a patent airway. If a
patient is identified as being at high risk for de-veloping postoperative
pulmonary complications, then chest phys-iotherapy is started immediately
(perhaps even before surgery). The techniques of postural drainage, vibration,
and percussion help to loosen and mobilize the secretions so that they can be
coughed up or suctioned.
RELIEVING PAIN AND DISCOMFORT
Pain
after a thoracotomy may be severe, depending on the type of incision and the
patient’s reaction to and ability to cope with pain. Deep inspiration is very
painful after thoracotomy. Pain can lead to postoperative complications if it
reduces the patient’s abil-ity to breathe deeply and cough, and if it further
limits chest ex-cursions so that ventilation becomes ineffective.
Immediately after the surgical procedure and before the incision is closed, the surgeon may perform a nerve block with a long-acting local anesthetic such as bupivacaine (Marcaine, Sensorcaine). Bupivacaine is titrated to relieve postoperative pain while allowing the patient to cooperate in deep breathing, coughing, and mobi-lization. However, it is important to avoid depressing the respira-tory system with excessive analgesia: the patient should not be so sedated as to be unable to cough. There is controversy about the ef-fectiveness of injections of local anesthetic for pain relief after tho-racotomy surgery. Research has shown that bupivacaine was no more effective than saline injections in treating postoperative tho-racotomy pain (Silomon et al., 2000).
Lidocaine
and prilocaine are local anesthetic agents used to treat pain at the site of
the chest tube insertion. These medica-tions are administered as topical
transdermal analgesics that pen-etrate the skin. Lidocaine and prilocaine have
also been found to be effective when used together. EMLA cream, which is a
mix-ture of the two medications, has been found to be effective in treating
pain from chest tube removal, and recent studies found it to be more effective
than intravenous morphine (Valenzuela & Rosen, 1999).
Because
of the need to maximize patient comfort without de-pressing the respiratory
drive, patient-controlled analgesia (PCA) is often used. Opioid analgesic
agents such as morphine are com-monly used. PCA, administered through an
intravenous pump or an epidural catheter, allows the patient to control the
frequency and total dosage. Preset limits on the pump avoid overdosage. With
proper instruction, these methods are well tolerated and allow earlier
mobilization and cooperation with the treatment regimen.
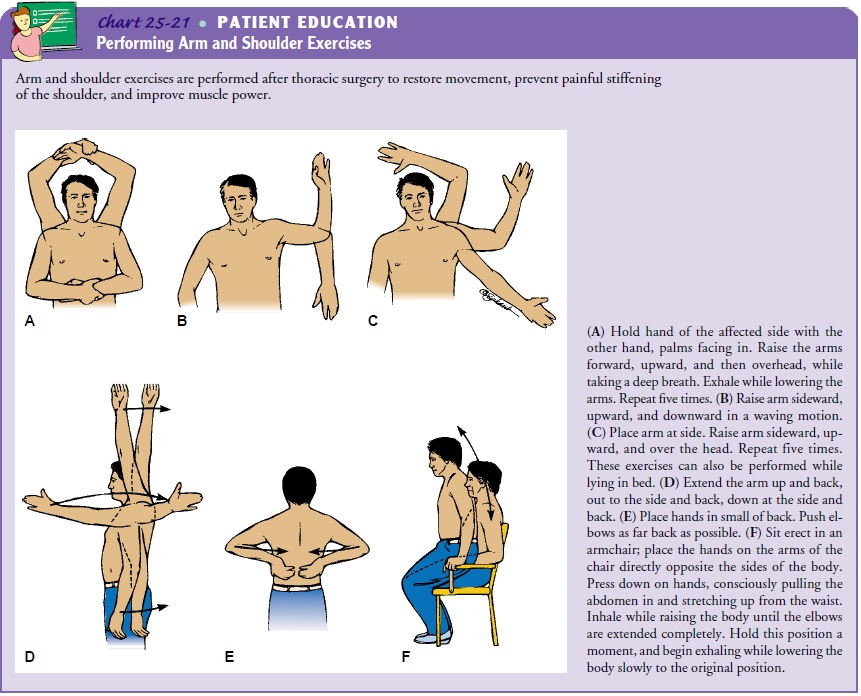
PROMOTING MOBILITY AND SHOULDER EXERCISES
Because
large shoulder girdle muscles are transected during a tho-racotomy, the arm and
shoulder must be mobilized by full range of motion of the shoulder. As soon as
physiologically possible, usually within 8 to 12 hours, the patient is helped
to get out of bed. Although this may be painful initially, the earlier the
patient moves, the sooner the pain will subside. In addition to getting out of
bed, the patient begins arm and shoulder exercises to restore movement and
prevent painful stiffening of the affected arm and shoulder (Chart 25-21).
MAINTAINING FLUID VOLUME AND NUTRITION
Intravenous Therapy
During
the surgical procedure or immediately after, the patient may receive a
transfusion of blood products, followed by a contin-uous intravenous infusion.
Because a reduction in lung capacity often occurs following thoracic surgery, a
period of physiologic ad-justment is needed. Fluids should be administered at a
low hourly rate and titrated (as prescribed) to prevent overloading the
vascu-lar system and precipitating pulmonary edema. The nurse performs careful
respiratory and cardiovascular assessments, as well as intake and output, vital
signs, and assessment of jugular vein distention. The nurse should also monitor
the infusion site for signs of infil-tration, including swelling, tenderness,
and redness.
Diet
It is not unusual for patients undergoing thoracotomy to have poor nutritional status before surgery because of dyspnea, sputum pro-duction, and poor appetite. Therefore, it is especially important that adequate nutrition be provided. A liquid diet is provided as soon as bowel sounds return; the patient is progressed to a full diet as soon as possible. Small, frequent meals are better tolerated and are crucial to the recovery and maintenance of lung function.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Complications
after thoracic surgery are always a possibility and must be identified and
managed early. In addition, the nurse monitors the patient at regular intervals
for signs of respiratory distress or developing respiratory failure,
dysrhythmias, bron-chopleural fistula, hemorrhage and shock, atelectasis, and
pul-monary infection.
Respiratory
distress is treated by identifying and eliminating its cause while providing
supplemental oxygen. If the patient pro-gresses to respiratory failure,
intubation and mechanical ventila-tion are necessary, eventually requiring
weaning.
Dysrhythmias
are often related to the effects of hypoxia or the surgical procedure. They are
treated with antiarrhythmic med-ication and supportive therapy. Pulmonary
infections or effusion, often preceded by atelectasis, may occur a few days
into the postoperative course.
Pneumothorax
may occur following thoracic surgery if there is an air leak from the surgical
site to the pleural cavity or from the pleural cavity to the environment. Failure
of the chest drainage system will prevent return of negative pressure in the
pleural cavity and result in pneumothorax. In the postoperative patient
pneumothorax is often accompanied by hemothorax. The nurse maintains the chest
drainage system and monitors the patient for signs and symptoms of
pneumothorax: increasing shortness of breath, tachycardia, increased
respiratory rate, and increasing res-piratory distress.
Bronchopleural
fistula is a serious but rare complication pre-venting the return of negative
intrathoracic pressure and lung re-expansion. Depending on its severity, it is
treated with closed chest drainage, mechanical ventilation, and possibly talc
pleu-rodesis.
Hemorrhage
and shock are managed by treating the under-lying cause, whether by reoperation
or by administration of blood products or fluids. Pulmonary edema from
overinfusion of intra-venous fluids is a significant danger. The early symptoms
are dyspnea, crackles, bubbling sounds in the chest, tachycardia, and pink,
frothy sputum. This constitutes an emergency and must be reported and treated
immediately.
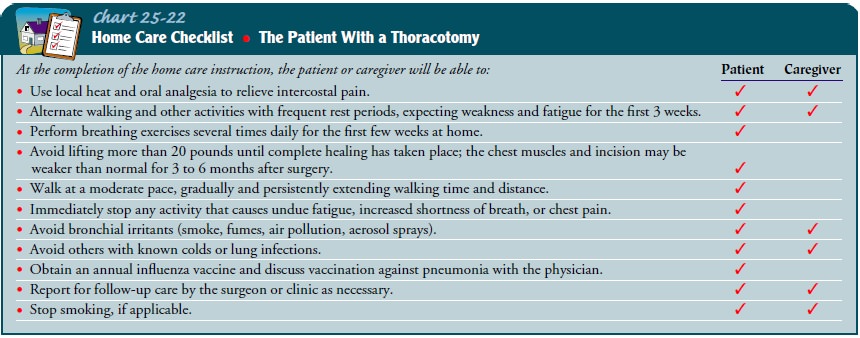
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
nurse instructs the patient and family about postoperative care that will be
continued at home. The nurse explains signs and symptoms that should be
reported to the physician. These include:
·
Change in respiratory status:
increasing shortness of breath, fever, increased restlessness or other changes
in mental or cognitive status, increased respiratory rate, change in
respi-ratory pattern, change in amount or color of sputum
·
Bleeding or other drainage from the
surgical incision or chest tube exit sites
·
Increased chest pain
In
addition, respiratory care and other treatment modalities (oxygen, incentive
spirometer, chest physiotherapy, and oral, in-haled, or intravenous
medications) may be continued at home. Therefore, the nurse needs to instruct
the patient and family in their correct and safe use.
The
nurse emphasizes the importance of progressively in-creased activity. The nurse
instructs the patient to ambulate within limits and explains that return of
strength is likely to be very gradual. Another important aspect of patient
teaching ad-dresses shoulder exercises. It is important to instruct the patient
to do these exercises five times daily. Additional patient teaching is
described in Chart 25-22.
Continuing Care
Depending
on the patient’s physical status and the availability of family assistance, a
home care referral may be indicated. The home care nurse assesses the patient’s
recovery from surgery, with special attention to respiratory status, the
surgical incision, chest drainage, pain control, ambulation, and nutritional
sta-tus. The patient’s use of respiratory modalities should be as-sessed to
ensure they are being used correctly and safely. In addition, the nurse
assesses the patient’s compliance with the postoperative treatment plan and
identifies acute or late post-operative complications.
The
recovery process may be longer than the patient had ex-pected, and providing
support to the patient is an important task for the home care nurse. Because of
shorter hospital stays, at-tending follow-up physician appointments is
essential. The nurse teaches the patient about the importance of keeping
follow-up appointments and completing laboratory tests as prescribed to as-sist
the physician in evaluating recovery. The home care nurse provides continuous
encouragement and education to the patient and family during the process. As
recovery progresses, the nurse also reminds the patient and family about the
importance of par-ticipating in health promotion activities and recommended
health screening.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
·
Demonstrates improved gas exchange,
as reflected in arte-rial blood gas measurements, breathing exercises, and use
of incentive spirometry
·
Shows improved airway clearance, as
evidenced by deep, controlled coughing and clear breath sounds or decreased
presence of adventitious sounds
·
Has decreased pain and discomfort by
splinting incision during coughing and increasing activity level
·
Shows improved mobility of shoulder
and arm; demon-strates arm and shoulder exercises to relieve stiffening
·
Maintains adequate fluid intake and
maintains nutrition for healing
·
Exhibits less anxiety by using
appropriate coping skills, and demonstrates a basic understanding of technology
used in care
·
Adheres to therapeutic program and
home care
·
Is free of complications, as
evidenced by normal vital signs and temperature, improved arterial blood gas
measure-ments, clear lung sounds, and adequate respiratory function
For a detailed plan of nursing care for the patient who has had a thoracotomy, see the Plan of Nursing Care.
Related Topics