Chapter: Clinical Dermatology: Connective tissue disorders
Other connective tissue diseases
Other
connective tissue diseases
Rheumatoid arthritis
Most
patients with rheumatoid arthritis have no skin disease, but some have tiny
fingertip infarcts, purpura, ulcers, palmar or peri-ungual erythema, or
pyoderma gangrenosum. The most common skin manifestations are marble-like
nodules near joints.
These
are always associated with the presence of rheumatoid factor. Some patients
with rheumatoid arthritis have a vasculitis of larger blood vessels with deep
‘punched out’ ulcers on the legs.
Reiter’s syndrome
Reiter’s
syndrome, precipitated by non-specific ure-thritis or dysentery, combines skin
lesions, arthropathy, conjunctivitis, balanitis, mucositis and spondylitis.
Arthritis is the most severe element. The skin lesions (keratoderma
blenorrhagicum) are psoriasis-like red scaling plaques, often studded with
vesicles and pus-tules, seen most often on the feet. The toes are red and
swollen, and the nails thicken. Psoriasiform plaques may also occur on the
penis and scrotum, with redness near the penile meatus. Topical steroids and
systemic NSAIDs help, but many patients need methotrexate and/or systemic steroids.
Relapsing polychondritis
This
process can affect any cartilage as the disorder is apparently caused by
autoimmunity to collagen. The ears are the usual target. The overlying skin
becomes red, swollen and tender. The cartilage in joints, the nose and the
tracheo-bronchial tree may be involved, so that patients develop floppy ears, a
saddle nose, hoarseness, stridor and respiratory insuf-ficiency. Aortic
aneurysms are also seen. Treatment is with systemic steroids and NSAIDs.
Tracheostomy may be necessary.
Behçet’s syndrome
Behçet’s
syndrome is discussed already.
Polyarteritis nodosa
This
is discussed in earily but is considered by some to be a connective tissue
disorder.
Panniculitis
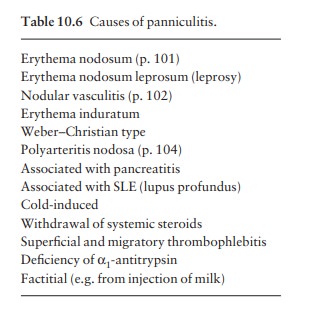
Panniculitis
is an inflammation of the subcutaneous fat. It includes a number of diseases
with different causes but a similar appearance: some are listed in Table 10.6.
Presentation
Most
patients have tender ill-defined red nodules on the lower legs, thighs and
buttocks.
Course
This
depends upon the cause. Migratory throm-bophlebitis may be associated with
underlying malignancy. In lupus profundus, a panniculitis is associated with
discoid or SLE. Erythema induratum may be caused by tuberculosis. Erythema
nodosum leprosum is a reactional state in leprosy. Patients with pancreatitis
may liberate enough lipase into the systemic circulation to cause fat in the
skin to liquefy and discharge through the overlying skin. The Weber–Christian
variant is associated with fever, but its cause is unknown.
Investigations
The
type of panniculitis can sometimes be identified by skin biopsy, which must
include subcutaneous fat. A complete blood count, ESR, chest X-ray, serum
lipase, serum α1-antitrypsin
and tests for antinuclear antibodies are needed.
Treatment
This
depends upon the cause. Rest, elevation of affected extremities and local heat
often help symptoms. NSAIDs may also bring help in the absence of specific
therapy
Related Topics