Chapter: Clinical Dermatology: Connective tissue disorders
Systemic lupus erythematosus

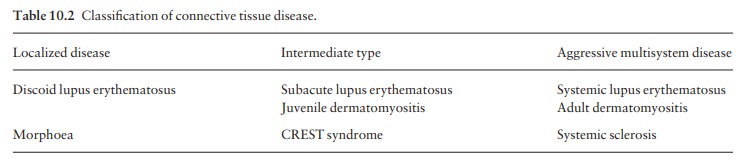
Lupus erythematosus
Lupus
erythematosus (LE) is a good example of such a spectrum, ranging from the
purely cutaneous type (discoid LE), through patterns associated with some
internal problems (disseminated discoid LE and sub-acute cutaneous LE), to a
severe multisystem disease (systemic lupus erythematosus, SLE; Table 10.2).
Systemic
lupus erythematosus
Cause
This
is unknown, but hereditary factors, e.g. com-plement deficiency and certain HLA
types, increase susceptibility. Particles looking like viruses have been seen
in endothelial cells, and in other tissues, but their role is not clear.
Patients with LE have autoantibodies to DNA, nuclear proteins and to other
normal antigens, and this points to an autoimmune cause. Exposure to sunlight
and artificial ultraviolet radiation (UVR), pregnancy and infection may
precipitate the disease or lead to flare-ups. Some drugs, such as hydralazine
and procainamide trigger SLE in a dose-dependent way, whereas others including
oral contraceptives, anti-convulsants, minocycline and captopril, precipitate
the disease just occasionally.
Presentation
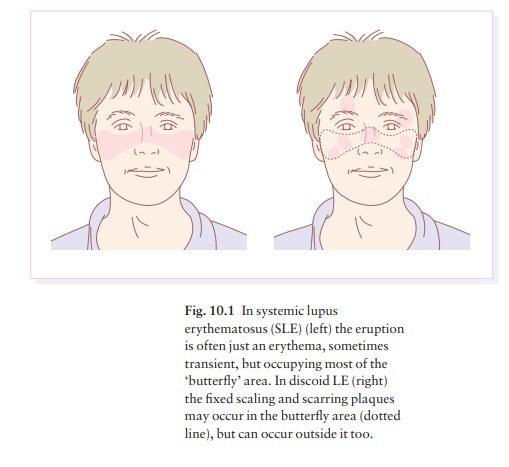
Typically,
but not always, the onset is acute. SLE is an uncommon disorder, affecting
women more often than men (in a ratio of about 8 : 1). The classic rash of
acute SLE is an erythema of the cheeks and nose in the rough shape of a
butterfly (Figs 10.1 and 10.2), with facial swelling. Occasionally, a few
blisters may be seen. Some patients develop widespread discoid papulosquamous
plaques very like those of discoid LE; others, about 20% of patients, have no
skin dis-ease at any stage.
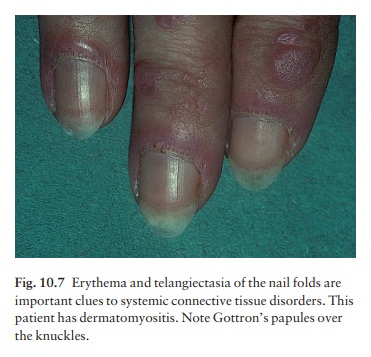
Other
dermatological features include peri-ungual telangiectasia (see Fig. 10.7),
erythema over the digits, hair fall (especially at the frontal margin of the
scalp), and photosensitivity. Ulcers may occur on the pal-ate, tongue or buccal
mucosa.
Course
The
skin changes may be transient, continuous or recurrent; they correlate well
with the activity of the systemic disease. Acute SLE may be associated with
fever, arthritis, nephritis, polyarteritis, pleurisy, pneu-monitis,
pericarditis, myocarditis and involvement of the central nervous system.
Internal involvement can be fatal, but the overall prognosis now is for about
three-quarters of patients to survive for 15 years. Renal involvement suggests
a poorer prognosis.
Complications
The skin disease may cause scarring or hyperpigmenta-tion, but the main dangers lie with damage to other organs and the side-effects of treatment, especially systemic steroids.
Differential diagnosis
SLE
is a great imitator. Its malar rash can be confused with sunburn, polymorphic
light eruption and rosacea. The discoid
lesions are distinct-ive, but are also seen in discoid LE and in subacute
cutaneous LE. Occasionally, they look like psoriasis or lichen planus. The hair
fall suggests telogen effluvium. Plaques on the scalp may cause a scarring
alopecia. SLE should be suspected when a characteristic rash is combined with
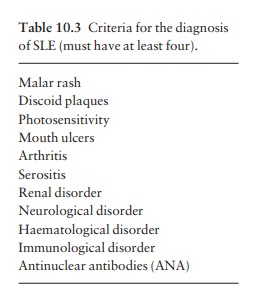
fever, malaise and internal disease (Table 10.3).
Investigations
Conduct
a full physical examination, looking for internal disease. Biopsy of skin
lesions is worthwhile because the pathology and immunopathology are
dis-tinctive. There is usually some thinning of the epidermis,
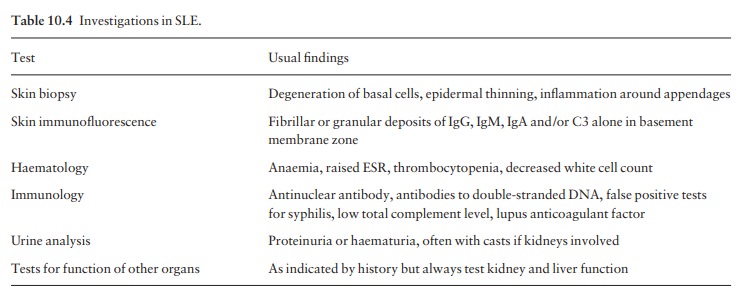
Direct immunofluorescence is helpful: IgG, IgM, IgA and C3 are
found individually or together in a band-like pattern at the dermo-epidermal
junction of involved skin and often uninvolved skin as well. Relevant
laboratory tests are listed in Table 10.4.
Treatment
Systemic steroids are the mainstay of treatment, with bed rest needed during exacerbations. Large doses of prednisolone are often needed to achieve control, as assessed by symptoms, signs, erythrocyte sedimentation rate (ESR), total comple-ment level and tests of organ function. The dosage is then reduced to the smallest that suppresses the disease. Immunosuppressive agents, such as azathio-prine, cyclophosphamide and other drugs (e.g. antihypertensive therapy or anticon-vulsants) may also be needed.
Antimalarial drugs may help some patients with marked photosensitivity, as may
sunscreens. Intermittent intravenous infusions of gamma globulin show promise.
Long-term and regular follow-up is necessary.
1 Do
not wait for the laboratory to confirm that your patient has severe SLE: use
systemic steroids quickly if indicated by clinical findings.
2
A person
with aching joints and smallamounts of antinuclear antibodies probably does not
have SLE.
3
Once
committed to systemic steroids, adjusttheir dosage on clinical rather than
laboratory grounds.
Related Topics