Chapter: Clinical Dermatology: Connective tissue disorders
Systemic sclerosis
Systemic
sclerosis
In
this disorder the skin becomes hard as connective tissues thicken. Early in the
condition, T-helper cells dominate the inflammatory infiltrate in the dermis
and cause fibroblasts to proliferate and produce more hyaluronic acid and type
I collagen. In addition there is intimal thickening of arterioles and arteries.
These processes are not confined to the skin, but involve many other organs,
including the gut, lungs, kidneys and heart, leading to their dysfunction and
to death.
The
cause of systemic sclerosis is unknown but many, apparently unrelated, pieces
of the complex jigsaw are now beginning to come together. A systemic
sclerosis-like syndrome is a feature of the chronic graft-vs.-host disease
sometimes seen after bone marrow transplantation and prolonged, untreated porphyria cutanea
torda. Similar syndromes have been reported following ingestion of adulterated
rapeseed oil in Spain and dimerised L-tryptophan
for insomnia and treatment with the antitumour agent, bleomycin. Environmental
factors may also be rel-evant in isolated cases; changes like those of systemic
sclerosis have affected workers exposed to polyvinyl chloride monomers,
trichlorethylene and epoxy resins and in those subjected for years to severe
vibration.
Presentation
Most
patients suffer from Raynaud’s phenomenon
and sclerodactyly. Their fingers become immob-ile, hard and shiny. Some
become hyperpigmented and itchy early in their disease. Peri-ungual
telangiec-tasia is common.
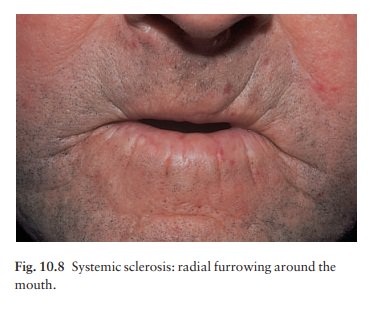
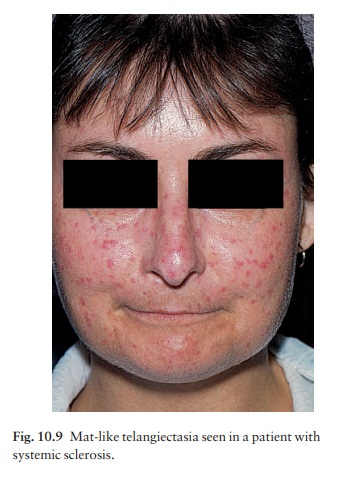
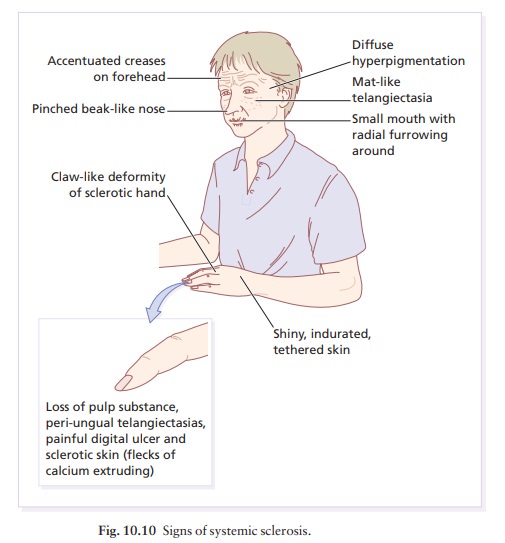
As
the disease progresses, sclerosis spreads to the face, scalp and trunk. The
nose becomes beak-like, and wrinkles radiate around the mouth (Fig. 10.8–
10.10). Most have abnormalities of the gut including dysphagia, oesophagitis,
constipation, diarrhoea and malabsorption. Fibrosis of the lungs leads to
dyspnoea, and fibrosis of the heart to congestive failure. The kidneys are involved
late, but this has a grave prognosis from malignant hypertension.
Complications
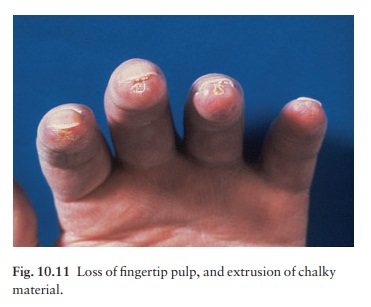
Most
complications are caused by the involvement of organs other than the skin, but
ulcers of the fingertips and calcinosis are distressing (Fig. 10.11). Hard skin
immobilizes the joints and leads to contractures.
Differential diagnosis
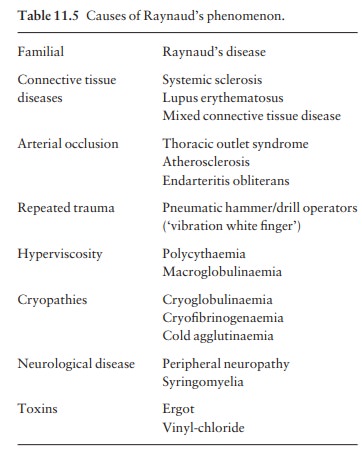
Other
causes of Raynaud’s phenomenon are given in Table 11.5. The differential
diagnosis includes chilblains and
erythromelalgia. The sclerosis should be distinguished from that of wide-spread
morphoea, porphyria cutanea tarda, mixed connective tissue disease,
eosinophilic fasciitis, dia-betic sclerodactyly and an acute arthritis with
swollen fingers. Rarely the disease is mimicked by progeria, scleromyxoedema,
amyloidosis or carcinoid syndrome. Changes like those of progressive systemic
sclerosis affect workers exposed to polyvinyl chloride mono-mers or to severe
chronic vibration, and are also seen in chronic graft-vs.-host reactions after
bone marrow transplants.
Investigations
The
diagnosis is made clinically because histological abnormalities are seldom
present until the physical signs are well established. Laboratory tests should
include a fluorescent antinuclear antibody test and the evaluation of the
heart, kidney, lungs, joints and muscles. Barium studies are best avoided as
obstruc-tion may follow poor evacuation. Other contrast media are available.
X-rays of the hands, measurement of muscle enzymes and immunoglobulin levels,
and a blood count, ESR and test for the scleroderma-associated antibody Scl-70
are also worthwhile.
Treatment
This is unsatisfactory. The calcium channel blocker nifedipine may help Raynaud’s phenomenon. Systemic steroids, salicylates, antimalarials and long-term penicillin are used, but are not of proven value. D-penicillamine has many side-effects, especially on renal function. Physiotherapy is helpful; photo-pheresis is experimental. Recently, there have been promising reports of the efficacy of ultraviolet A-1 (340 – 400 nm) phototherapy for affected skin in systemic sclerosis.
Related Topics