Chapter: Clinical Dermatology: Disorders of blood vessels and lymphatics
Disorders involving small blood vessels
Disorders
involving small blood vessels
Acrocyanosis
This
type of ‘poor circulation’, often familial, is more common in females than
males. The hands, feet, nose, ears and cheeks become blue-red and cold. The
palms are often cold and clammy. The condition is caused by arteriolar
constriction and dilatation of the subpapil-lary venous plexus, and to
cold-induced increases in blood viscosity. The best answers are warm clothes
and the avoidance of cold.
Erythrocyanosis
This
occurs in fat, often young, women. Purple-red mottled discoloration is seen
over the buttocks, thighs and lower legs. Cold provokes it and causes an
unpleas-ant burning sensation. An area of acrocyanosis or erythrocyanosis may
be the site where other disorders will settle in the future, e.g. perniosis,
erythema in-duratum, lupus erythematosus, sarcoidosis, cutaneous tuberculosis and
leprosy.
Perniosis (chilblains)
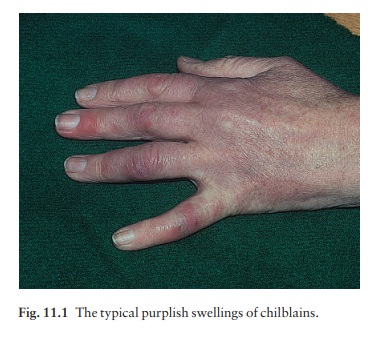
In
this common, sometimes familial, condition, inflamed purple-pink swellings
appear on the fingers, toes and, rarely, ears (Fig. 11.1). They arrive with
winter and are induced by cold. They are painful, and itchy or burning on
rewarming. Occasionally they ulcerate. Chilblains are caused by a combination
of arteriolar and venular constriction, the latter predom-inating on rewarming
with exudation of fluid into the tissues. Warm housing and clothing help.
Topical remedies rarely work, but the oral calcium channel blocker nifedipidine
may be useful. The blood pressure should be monitored at the start of treatment
and at return visits. The vasodilator nicoti-namide (500 mg three times daily)
may be helpful alone or in addition to calcium channel blockers. Sympathectomy
may be advised in severe cases.
Erythromelalgia
This is a rare condition in which the extremities become red, hot and painful when they or their owner are exposed to heat.
The condition may be idiopathic, or caused by a myeloproliferative disease (e.g. poly-cythaemia rubra vera or thrombocythaemia), lupus erythematosus, rheumatoid arthritis, diabetes, degen-erative peripheral vascular disease or hypertension. Small doses of aspirin give symptomatic relief. Alternatives include non-steroidal anti-inflammatory drugs (NSAIDs), α blockers and oxpentifylline (pentoxifylline).
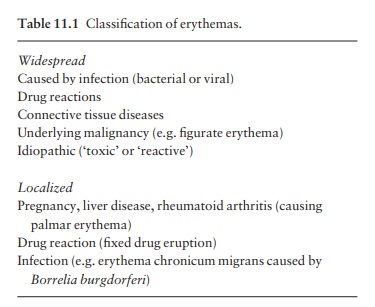
Erythemas
Erythema
accompanies all inflammatory skin condi-tions, but the term ‘the erythemas’ is
usually applied to a group of conditions with redness but without prim-ary
scaling. Such areas are seen in some bacterial and viral infections such as
toxic shock syndrome and measles. Drugs are another common cause . If no cause
is obvious, the rash is often called a ‘toxic’ or ‘reactive’ erythema (Table
11.1).
When
erythema is associated with oedema (‘urticated erythema’) it becomes palpable.
Figurate erythemas
These
are chronic eruptions, made up of bizarre ser-piginous and erythematous rings.
In the past most carried Latin labels; happily, these eruptions are now grouped
under the general term of ‘figurate erythemas’. Underlying malignancy, a
connective tissue disorder, a bacterial, fungal or yeast infection, worm
infestation, drug sensitivity and rheumatic heart disease should be excluded,
but often the cause remains obscure.
Palmar erythema
This
may be an isolated finding in a normal person or be familial. Sometimes it is
seen in pregnancy, liver disease or rheumatoid arthritis. Often associated with
spider telangiectases , it may be caused by increased circulating oestrogens.
Erythema migrans
These
annular erythematous areas are usually solitary, and occur most often on
exposed skin after a tick bite. They expand slowly and may become very large.
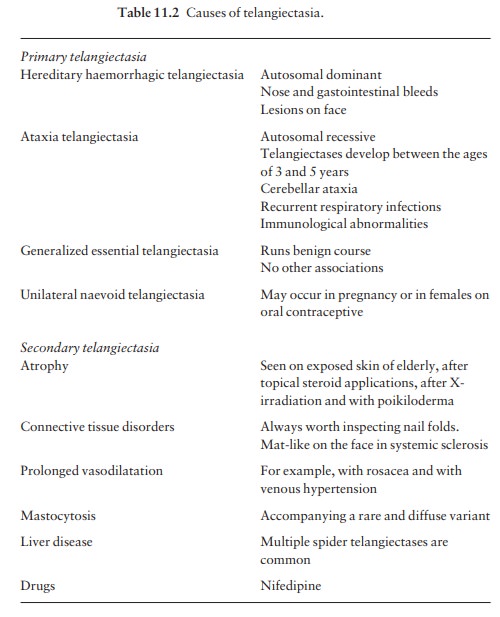
Telangiectases
This
term refers to permanently dilatated and visible small vessels in the skin.
They appear as linear, punctate or stellate crimson-purple markings. The common
causes are given in Table 11.2.
Spider naevi
These
stellate telangiectases do look rather like spiders, with legs radiating from a
central, often palpable, feeding vessel. If the diagnosis is in doubt, press on
the central feeding vessel with the corner of a glass slide and the entire
lesion will disappear. Spider naevi are seen frequently on the faces of normal
children, and may erupt in pregnancy or be the presenting sign of liver
disease, with many lesions on the upper trunk. Liver function should be checked
in those with many spider naevi. The central vessel can be destroyed by
electrodessication without local anaesthesia or with a pulsed dye laser.
Livedo reticularis
This
cyanosis of the skin is net-like or marbled and caused by stasis in the
capillaries furthest from their arterial supply: at the periphery of the
inverted cone supplied by a dermal arteriole (see Fig. 2.1). ‘Cutis marmorata’
is the name given to the mottling of the skin seen in many normal children. It
is physiological and disappears on warming, whereas true livedo reticularis
remains.
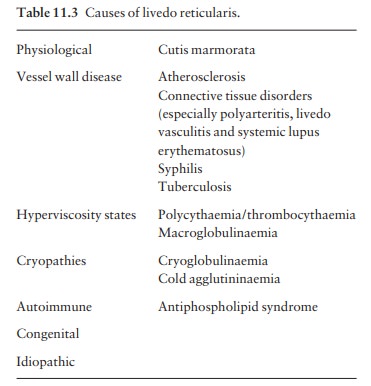
The causes of livedo reticularis are listed in Table 11.3. Livedo vasculitis and cutaneous polyarteritis are forms of vasculitis associated with livedo reticularis .
Antiphospholipid syndrome
Some patients with an apparently idiopathic livedo reticularis develop progressive disease in their peri-pheral, cerebral, coronary and renal arteries. Others, usually women, have multiple arterial or venous thrombo-embolic episodes accompanying livedo reticularis. Recurrent spontaneous abortions and intrauterine fetal growth retardation are also features. Prolongation of the activated partial thromboplastin time (APTT) and the presence of antiphospholipid antibodies (either anticardiolipin antibody or lupus anticoagulant, or both) help to identify this syndrome. Systemic lupus erythematosus should be excluded .
Erythema ab igne
This
appearance is also determined by the underlying vascular network. Its
reticulate pigmented erythema, with variable scaling, is caused by damage from
long-term exposure to local heatausually from an open fire, hot water bottle or
heating pad. If on one side of the leg, it gives a clue to the side of the fire
on which granny likes to sit (Fig. 11.2). The condition is com-mon in northern
Europe (‘tinker’s tartan’), but rare in the USA, where central heating is the
rule.

Flushing
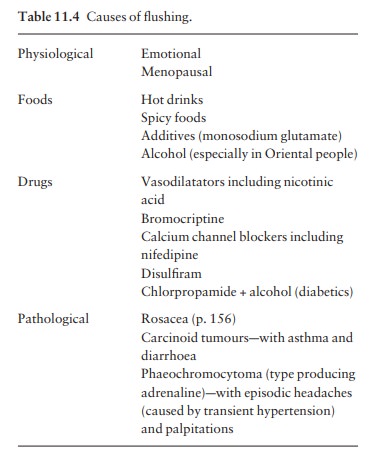
This
transient vasodilatation of the face may spread to the neck, upper chest and,
more rarely, other parts of the body. There is no sharp distinction between
flushing and blushing apart from the emotional pro-vocation of the latter. The
mechanism varies with the many causes that are listed in Table 11.4. Paroxysmal
flushing (‘hot flushes’), common at the menopause, is associated with the
pulsatile release of luteinizing hormone from the pituitary, as a consequence
of low circulating oestrogens and failure of normal negative feedback. However,
luteinizing hormone itself cannot
be
responsible for flushing as this can occur after hypophysectomy. It is possible
that menopausal flush-ing is mediated by central mechanisms involving
encephalins. Hot flushes can usually be helped by oestrogen replacement.
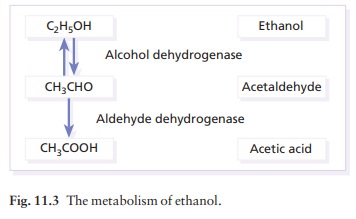
Alcohol-induced
flushing is most commonly seen in oriental people. Ethanol is broken down to
acetalde-hyde by alcohol dehydrogenase and acetaldehyde is metabolized to
acetic acid by aldehyde dehydrogenase (Fig. 11.3). Acetaldehyde accumulation is
in part responsible for flushing. Oriental people not only may have a
high-activity variant of alcohol dehydrogenase but also defective aldehyde
dehydrogenase. Disulfuram (Antabuse) and, to a lesser extent, chlorpropamide
inhibit aldehyde dehydrogenase so that some indi-viduals taking these drugs may
flush.
Related Topics