Chapter: Clinical Dermatology: Disorders of blood vessels and lymphatics
Arterial disease
Arterial
disease
Raynaud’s phenomenon
This
is a paroxysmal pallor of the digits provoked by cold or, rarely, emotional
stress. At first the top of one or more fingers becomes white. On rewarming, a
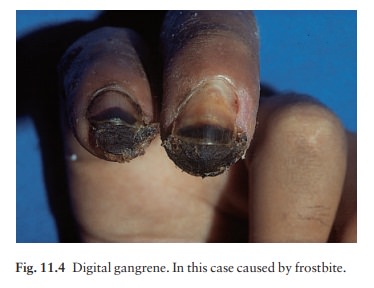
In severe disease the fingers lose pulp substance, ulcerate or become
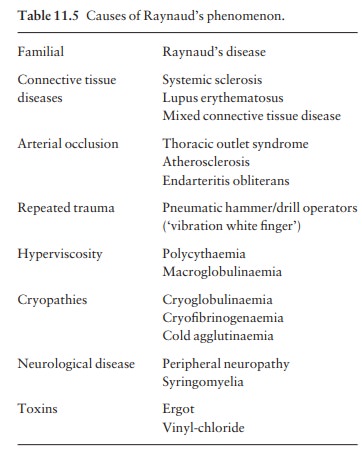
gangrenous (Fig. 11.4). Some causes are listed in Table 11.5. Raynaud’s
disease, often familial, is the name given when no cause can be found. However,
some patients with what seems to be Raynaud’s disease will later develop a
connective tissue disease, usually scleroderma.
The
main treatment is to protect the vulnerable digits from cold. Warm clothing
reduces the need for peripheral vasoconstriction to conserve heat. Smoking
should be abandoned. Calcium channel blockers (e.g. nifedipine 10–30 mg three
times daily) are the most effective agents although they work best in patients
with primary Raynaud’s disease. Patients should be warned about dizziness
caused by postural hypoten-sion. Initially it is worth giving nifedipine as a
5-mg test dose with monitoring of the blood pressure in the clinic. If this is
tolerated satisfactorily the starting dosage should be 5 mg daily, increasing
by 5 mg every
The blood pressure should be monitored before
each incremental increase in the dosage. Diltiazem (30–60 mg three times daily)
is less effective than nifedipine but has fewer side-effects. Systemic
vasodil-ators such as naftidrofuryl oxalate, nicotinic acid and thymoxamine
(moxisylyte) are also worth trying. Glycerol trinitrate ointment, applied once
daily may reduce the severity and frequency of attacks and may allow reduction
in the dosage of calcium channel blockers and vasodilators. Infusions with
reserpine or prostacyclin help some severe cases although occasionally
sympathectomy is needed.
Polyarteritis nodosa
This
is discussed in already.
Temporal arteritis
Here
the brunt is borne by the larger vessels of the head and neck. The condition
affects elderly people and may be associated with polymyalgia rheum-atica. The
classical site is the temporal arteries, which become tender and pulseless, in
association with severe headaches. Rarely, necrotic ulcers appear on the scalp.
Blindness may follow if the ophthalmic arteries are involved, and to reduce
this risk systemic steroids should be given as soon as the diagnosis has been
made. In active phases the erythrocyte sedimentation rate (ESR) is high and its
level can be used to guide treatment, which is often prolonged.
Atherosclerosis
This
occlusive disease, most common in developed countries, will not be discussed in
detail here, but involvement of the large arteries of the legs is of concern to
dermatologists. It may cause intermittent claudication, nocturnal cramp, ulcers
or gangrene. These may develop slowly over the years, or within minutes if a
thrombus forms on an atheromatous plaque. The feet are cold and pale, the skin
is often atrophic, with little hair, and peripheral pulses are diminished or
absent.
Investigations
should include urine testing to exclude diabetes mellitus. Fasting plasma
lipids (cholesterol, triglycerides and lipoproteins) should be checked in the
young, especially if there is a family history of vascular disease. Doppler
ultrasound measurements help to distinguish atherosclerotic from venous leg ulcers
in the elderly. Complete assessment is best carried out by a specialist in
peripheral vascular disease or a vascular surgeon.
Arterial emboli
Emboli
may lodge in arteries supplying the skin and cause gangrene, ulcers or necrotic
papules, depending on the size of the vessel obstructed. Causes include
dislodged thrombi (usually from areas of atheroscle-rosis), fat emboli (after
major trauma), infected emboli (e.g. gonococcal septicaemia or subacute
bacterial endocarditis) and tumour emboli.
Pressure sores (Fig. 11.5)
Sustained
or repeated pressure on skin over bony prominences can cause ischaemia and
pressure sores. These are common in patients over 70 years old who are confined
to hospital, especially those with a frac-tured neck of femur. The morbidity
and mortality of those with deep ulcers is high.

Cause
The
main factors responsible for pressure sores are as follows.
1 Prolonged
immobility and recumbency (e.g. caused by paraplegia, arthritis or senility).
2 Vascular
disease (e.g. atherosclerosis).
3 Neurological
disease causing diminished sensation(e.g. in paraplegia).
4 Malnutrition,
severe systemic disease and generaldebility.
Clinical features
The
sore begins as an area of erythema which pro-gresses to a superficial blister
or erosion. If pressure continues, deeper damage occurs with the develop-ment
of a black eschar which, when removed or shed, reveals a deep ulcer, often
colonized by Pseudomonasaeruginosa.
The skin overlying the sacrum, greatertrochanter, ischial tuberosity, the heel
and the lateral malleolus is especially at risk.
Management
The
following are important.
Prevention:
by turning recumbent patients regu-larly and using antipressure mattresses for
susceptible patients.
2 Treatment
of malnutrition and the general condition.
3 Debridement.
Regular cleansing with normal salineor 0.5% aqueous silver nitrate.
Antibacterial prepara-tions locally. Absorbent dress-ings. Semipermeable
dressings such as Opsite, if there is no infection. Appropriate systemic
antibiotic if an infection is spreading.
4 Plastic
surgical reconstruction may be indicated inthe young when the ulcer is clean.
Related Topics