Chapter: Clinical Dermatology: Disorders of blood vessels and lymphatics
Venous hypertension, the gravitational syndrome and venous leg ulceration
Venous
hypertension, the gravitational syndrome and venous leg ulceration
Ulcers
of the lower leg, secondary to venous hyperten-sion, have an estimated
prevalence of around 1%, are more common in women than in men, and account for
some 85% of all leg ulcers seen in the UK and USA.
Cause
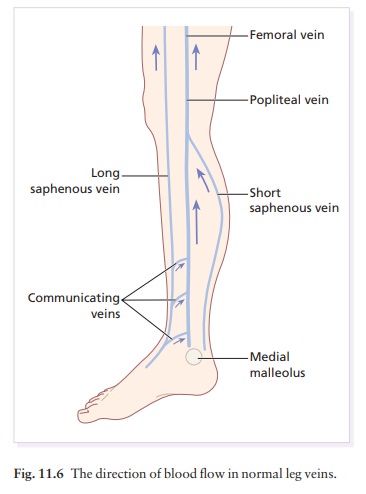
Satisfactory
venous drainage of the leg requires three sets of veins: deep veins surrounded by muscles; superficial
veins; and the veins connecting these togetherathe perforating or communicating
veins (Fig. 11.6). When the leg muscles contract, blood in the deep veins is
squeezed back, against gravity, to the heart (the calf muscle pump); reflux is
prevented by valves. When the muscles relax, with the help of gravity, blood
from the superficial veins passes into the deep veins via the communicating
vessels. If the valves in the deep and communicating veins are incompetent, the
calf muscle pump now pushes blood into the super-ficial veins, where the
pressure remains high (‘venous hypertension’) instead of dropping during
exercise. This persisting venous hypertension enlarges the cap-illary bed;
white cells accumulate here and are then activated (by hypoxic endothelial
cells), releasing oxygen free radicals and other toxic products which cause local
tissue destruction and ulceration. The increased venous pressure also forces
fibrinogen and α2-macroglobulin out through the capillary walls;
thesemacromolecules trap growth and repair factors so that minor traumatic
wounds cannot be repaired and an ulcer develops. Patients with these changes
develop lipodermatosclerosis and have a
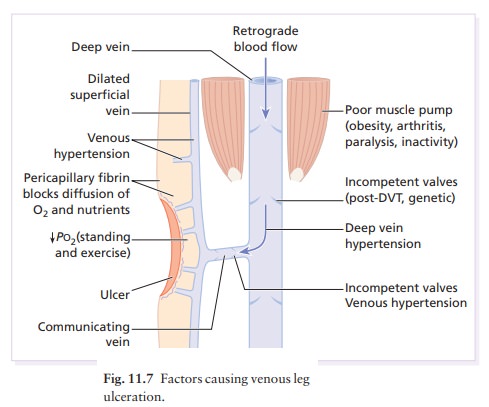
high serum fibrinogen and reduced blood fibrinolytic activity. Figure 11.7
shows the factors causing venous ulceration.
Clinical features
Venous
hypertension is heralded by a feeling of heavi-ness in the legs and by pitting
oedema. Other signs include:
1 red
or bluish discoloration;
2 loss of
hair;
3 brown
pigmentation (mainly haemosiderin fromthe breakdown of extravasated red blood
cells) and scattered petechiae;
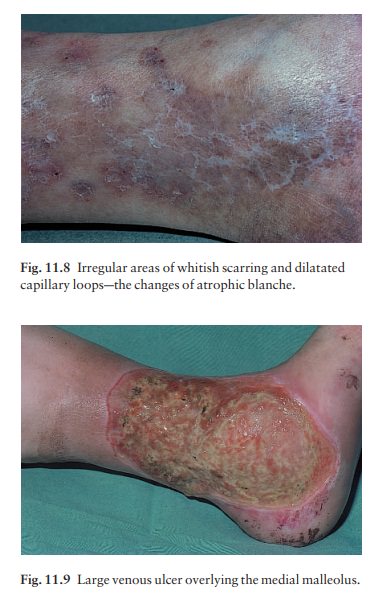
4 atrophie
blanche (ivory white scarring withdilatated capillary loops; Fig. 11.8); and
5 induration,
caused by fibrosis and oedema of thedermis and subcutisasometimes called
‘lipoder-matosclerosis’.
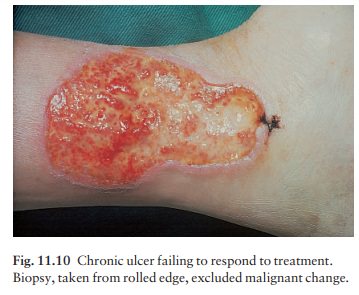
Ulceration
is most common near the medial malleo-lus (Fig. 11.9). In contrast to arterial
ulcers, which are usually deep and round, with a punched out appearance, venous
ulcers are often large but shallow, with prominent granulation tissue in their
bases. Incompetent perforating branches (blowouts) between the superficial and
deep veins are best felt with the patient standing. Under favourable conditions
the exudative phase gives way to a granulating and healing phase, signalled by
a blurring of the ulcer mar-gin, ingrowth of skin from it, and the appearance
of scattered small grey epithelial islands over the base. Prolonged ulceration,
with lipodermatosclerosis, gives the leg the look of an inverted champagne
bottle.
Complications
Bacterial superinfection is inevitable in a longstanding ulcer, but needs systemic antibiotics only if there is pyrexia, a purulent discharge, rapid extension or an increase in pain, cellulitis, lymphangitis or septicaemia.
Eczema is common around venous ulcers. Allergic
contact dermatitis is a common
com-plication and should be suspected if the rash worsens, itches or fails to
improve with local treatment. Lanolin, parabens (a preservative) and neomycin
are the most common culprits.
Malignant
change can occur. If an ulcer has a hyper-plastic base or a rolled edge, biopsy
may be needed to rule out a squamous cell carcinoma (Fig. 11.10).
Differential diagnosis
The
main causes of leg ulceration are given in Table 11.7. The most important
differences between venous and other leg ulcers are the following.
Atherosclerotic.
These ulcers are more common onthe toes, dorsum of foot, heel, calf and shin,
and are unrelated to perforating veins. Their edges are often sharply defined,
their outline may be polycyclic and the ulcers may be deep and gangrenous.
Islands of intact skin are characteristically seen within the ulcer.
Claudication may be present and peripheral pulses absent.
Vasculitic.
These ulcers start as painful palpable pur-puric lesions, turning into small
punched-out ulcers.
The
involvement of larger vessels is heralded by painful nodules that may ulcerate.
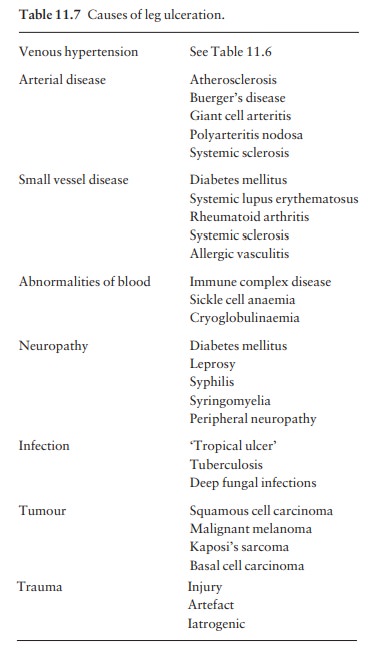
The intractable deep sharply demarcated ulcers of rheumatoid arthritis are
caused by an underlying vasculitis (Fig. 11.11).
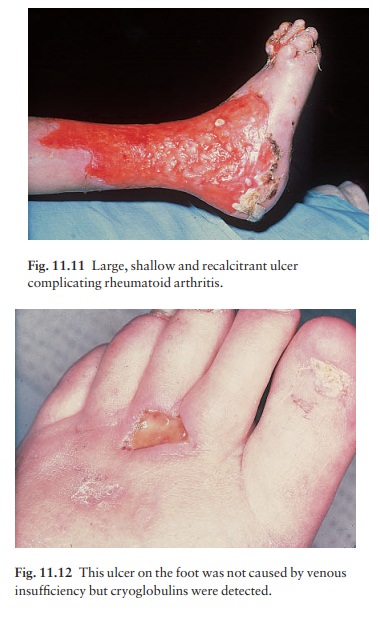
Thrombotic
ulcers. Skin infarction (Fig. 11.12), lead-ing to ulceration, may
be caused by embolism or by the increased coagulability of polycythaemia or
cryoglobulinaemia.
Infective
ulcers. Infection is now a rare cause of legulcers in the UK but
ulcers caused by tuberculosis, leprosy, atypical mycobacteria, diphtheria and
deep fungal infections, such as sporotrichosis or chro-moblastomycosis, are
still seen in the tropics.
Panniculitic
ulcers. These may appear at odd sites,such as the thighs, buttocks
or backs of the calves. The most common types of panniculitis that ulcerate are
lupus panniculitis, pancreatic panniculitis and erythema induratum.
Malignant
ulcers. Those caused by a squamous cellcarcinoma are the most common, but both malignant
melanomas and basal cell
carcino-mas can present as flat lesions,
which expand, crust and ulcerate. Furthermore, squamous cell carci-noma can
arise in any longstanding ulcer, whatever its cause.
Pyoderma
gangrenosum. These large andrapidly spreading ulcers may be circular or
polycyclic, and have a blue, indurated, undermined or pustular margin. Pyoderma
gangrenosum may complicate rheumatoid arthritis, Crohn’s disease, ulcerative
co-litis or blood dyscrasias.
Investigations
Most
chronic leg ulcers are venous, but other causes should be considered if the
signs are atypical. In patients with venous ulcers, a search for contributory
factors, such as obesity, peripheral artery disease, cardiac failure or
arthritis, is always worthwhile. Investigations should include the following.
•
Urine test for sugar.
•
Full blood count to detect anaemia,
which will delay healing.
•
Swabbing for pathogens (see
Bacterial superinfec-tion above).
•
Venography, colour flow duplex
scanning and the measurement of ambulatory venous pressure help to detect
surgically remediable causes of venous incompetence.
•
Doppler ultrasound may help to
assess arterial cir-culation when atherosclerosis is likely. It seldom helps if
the dorsalis pedis or posterior tibial pulses can easily be felt. If the
maximal systolic ankle pressure divided by the systolic brachial pressure
(‘ankle brachial pres-sure index’) is greater than 0.8, the ulcer is unlikely
to be caused by arterial disease.
Cardiac
evaluation for congestive failure.
Venous
ulcers will not heal if the leg remains swollen and the patient chair-bound.
Pressure bandages take priority over other measures but not for
atheroscle-rotic ulcers with an already precarious arterial supply. A common error
is to use local treatment that is too elaborate. As a last resort, admission to
hospital for elevation and intensive treatment may be needed, but the results
are not encouraging; patients may stay in the ward for many months only to have
their appar-ently well-healed ulcers break down rapidly when they go home.
The
list of therapies is extensive. They can be divided into the following
categories: physical, local, oral and surgical.
Physical measures
Compression bandages and stockings
Compression
bandaging, with the compression gradu-ated so that it is greatest at the ankle
and least at the top of the bandage, is vital for most venous ulcers; it
reduces oedema and aids venous return. The ban-dages are applied over the ulcer
dressing, from the forefoot to just below the knee. Self-adhesive ban-dages
(e.g. Secure Forte and Coban) are convenient and have largely replaced
elasticated bandages. Bandages stay on for 2–7 days at a time and are left on
at night. One four-layer compression bandaging system includes a layer of
orthopaedic wool (Velband), a standard crepe, an elasticated bandage (e.g.
Elset and Litepress) and an elasticated cohesive bandage (e.g. Secure Forte and
Coban): it requires changing only once a week and is very effective. The
combined four layers give a 40-mmHg compression at the ankle. Once an ulcer has
healed, a graduated compression stocking (e.g. Duomed, Medi Strumpf, or Venosan
2502/2003 (UK) or Jobst or Teds (USA)) from toes to knee (or preferably thigh),
should be prescribed, preferably at pressures of at least 35 mmHg. A foam or
felt pad may be worn under the stockings to pro-tect vulnerable areas against
minor trauma. The stocking should be put on before rising from bed. Care must
be taken with all forms of compression to ensure that the arterial supply is
satisfactory and not compromised.
Elevation of the affected limb
Preferably
above the hips, this aids venous drainage, decreases oedema and raises oxygen
tension in the limb. Patients should rest with their bodies horizontal and their
legs up for at least 2 h every afternoon. The foot of the bed should be raised
by at least 15 cm ; it is not enough just to put a pillow under the feet.
Walking
Walking,
in moderation, is beneficial, but prolonged standing or sitting with dependent
legs is not.
Physiotherapy
Some
physiotherapists are good at persuading venous ulcers to heal. Their secret
lies in a combination of the following: leg exercises, elevation, gentle
massage, ultrasound treatment to the skin around the ulcers, oedema pumps and graduated
compression bandaging.
Diet
Many
patients are obese and should lose weight.
Local therapy
Remember
that many ulcers will heal with no treat-ment at all but, if their blood flow
is compromised, they will not heal despite meticulous care.
Local
therapy should be chosen to:
•
control or absorb the exudates;
•
reduce the pain;
•
control the odour;
•
protect the surrounding skin;
•
remove surface debris;
•
promote re-epithelialization; and
•
make optimal use of nursing time.
There
are many preparations to choose from; those we have found most useful are
listed in Formulary 1.
Clean
ulcers (Fig. 11.13)
Dressings
need be changed only once or twice a week, keeping the ulcer moist. Paraffin
tulle dressings, plain or impregnated with 0.5% chlorhexidine, 0.25% silver
proteinate in compound calamine cream spread on a non-stick dressing, 1% silver
sulphadiazine cream, and simple zinc and castor oil ointment, are all helpful
and easy to apply. The area should be cleaned gently with arachis oil, 5%
hydrogen peroxide or saline before the next dressing is applied. Sometimes
immersing the whole ulcer in a tub of warm water helps to loosen or dissolve
adherent crusts. The pro-longed use of antiseptics may be harmful.

Many
dressings have absorbent and protective pro-perties. These include Granuflex
and DuoDERM Extra Thin (which have the advant-age of sticking to the
surrounding skin), Geliperm, Kaltostat and Sorbsan in the UK and Duoderm,
Opsite and Tegaderm in the USA. Actisorb (UK) is a useful charcoal dressing
that absorbs exudate and minimizes odour. Ointments containing recombinant
human platelet growth factor may aid revascularization.
Medicated bandages based on zinc paste, with ichthammol, or with calamine and clioquinol, are useful when there is much surround-ing eczema, and can be used for all types of ulcers, even infected exuding ones. The bandage is applied in strips from the foot to below the knee. Worsening of eczema under a medicated bandage may signal the development of allergic contact dermatitis to a component of the paste, most often parabens (a pre-servative) or cetostearyl alcohols.
Infected
ulcers (Fig. 11.14)
These
have to be cleaned and dressed more often than clean ones, sometimes even twice
daily. Useful pre-parations include 0.5% silver nitrate, 0.25% sodium
hypochlorite, 0.25% acetic acid, potassium perman-ganate (1 in 10 000 dilution)
and 5% hydrogen per-oxide, all made up in aqueous solution, and applied as
compresses with or without occlusion. Helpful creams and lotions include 1.5%
hydrogen peroxide, 20% benzoyl peroxide, 1% silver sulphadiazine, 10%
povidone-iodine. The main function of dextran polymer beads, and starch
poly-mer beads within cadexomer iodine, is to absorb exudate. Although
antibiotic tulles are easy to apply and are well tolerated, they should not be
used for long periods as they can induce bacterial resistance and sensitize.
Resistance is not such a problem with povidone-iodine, and a readily applied
non-adherent dressing impregnated with this antiseptic may be useful.
Surrounding eczema is helped by weak or moderate strength local steroids, which
must never be put on the ulcer itself. Lassar’s paste, zinc cream or paste
bandages are suitable alternatives.

Oral treatment
The
following may be helpful.
Diuretics.
Pressure bandaging is more important asthe oedema associated with venous
ulceration is largely mechanical. Diuretics will combat the oedema of cardiac
failure.
Analgesics. Adequate analgesia is important.
Aspirinmay not be well tolerated by the elderly. Paracetamol (not available in
the USA), or acetaminophen is often adequate but dihydrocodeine may be
required. Ana-lgesia may be needed only when the dressing is changed.
Antibiotics. Ulcers need not be ‘sterilized’ by
local orsystemic antibiotics. Short courses of systemic anti-biotics should be
reserved for spreading infections (see under Complications above) but are
sometimes tried for pain or even odour. Bacteriological guidance is needed and
the drugs used include erythromycin and flucloxacillin (streptococcal or
staphylococcal cellulitis), metronidazole (Bacteroides
infection) and ciprofloxacin (Pseudomonas aeruginosa
infection). Bacterial infection may prejudice the outcome of skin grafting.
Ferrous
sulphate and folic acid. For anaemia.
Zinc
sulphate. May help to promote healing, espe-cially if the plasma
zinc level is low.
Oxypentifylline
(pentoxyfylline) is fibrinolytic, in-creases the
deformability of red and white blood cells, decreases blood viscosity and
diminishes platelet adhes-iveness. It may speed the healing of venous ulcers if
used with compression bandages.
Stanozolol.
This anabolic steroid may not heal anexisting ulcer more quickly, but may
prevent ulcera-tion in lipodermatosclerosis and may protect against
recurrences. The manufacturer’s advice on contrain-dications, e.g. prostatic
cancer and abnormal liver function, and on monitoring treatment must not be
overlooked.
Oxerutins.
These may help the oedema and symptomsof venous hypertension and are said to
reduce leakage from capillaries by acting on the endothelial cells.
Surgery
Autologous
pinch, split-thickness or mesh grafts have a place. Lyophilized pig dermis, and
synthetic films similar to skin, may also be tried. Sheets of human epidermis
grown in tissue culture can be purchased and placed on granulating wound beds.
Even if grafts do not take, they may stimulate wound healing and relieve pain.
In general, grafts work best on clean ulcers.
Venous
surgery on younger patients with varicose veins may prevent recurrences, if the
deep veins are competent. Patients with atherosclerotic ulcers should see a
vascular surgeon for assessment. Some blockages are surgically remediable.
Related Topics