Chapter: Obstetrics and Gynecology: Abnormal Labor and Intrapartum Fetal Surveillance
Operative Delivery
OPERATIVE DELIVERY
Operative vaginal deliveries are
accomplished by apply-ing direct traction on the fetal skull with forceps, or
by applying traction to the fetal scalp by means of a vacuum extractor. The
incidence of operative vaginal delivery in the United States is estimated to be
10% to 15%. Although considered safe in
appropriate circumstances, opera-tive vaginal delivery has the potential for
maternal and neo-natal complications. Operative vaginal delivery shouldbe
performed only by individuals with privileges for such procedures and in
settings in which personnel are read-ily available to perform a cesarean
delivery in the event the operative vaginal delivery is unsuccessful. However,
the incidence of intracranial hemorrhage is highest among infants delivered by
cesarean section following a failed vacuum or forceps delivery. The combination
of vacuum and forceps has a similar risk for intracranial hemor-rhage.
Therefore, an operative vaginal delivery should not be attempted when the
probability of success is very low
Classification
For both forceps and vacuum
extraction deliveries, the type of delivery depends on the fetal station—the
relationship between the leading portion of the fetal head and the level of the
maternal ischial spines. Outlet
operative vaginaldelivery is the application of forceps or vacuum under
thefollowing conditions:
·
The scalp is visible at the
introitus without separating labia.
·
The fetal skull has reached
pelvic floor.
·
The sagittal suture is in
anteroposterior diameter or right or left occiput anterior or posterior
position.
·
The fetal head is at or on the
perineum.
·
Rotation does not exceed 45°.
Low
operative vaginal delivery is the application offorceps or
vacuum when the leading point of the fetal skull is at station +2 or more and is not on the
pelvic floor. This type of operative vaginal delivery has two sub-types:
·
Rotation 45° or less (left or right occiput
anterior to occiput anterior, or left or right occiput posterior to occiput
posterior)
·
Rotation greater than 45°
Midpelvis
operative vaginal delivery is the applicationof forceps or
vacuum when the fetal head is engaged but the leading point of the skull is
above station +2. Under
very unusual circumstances, such as the sudden onset of severe fetal or
maternal compromise, application of for-ceps or vacuum above station +2 may be attempted while
simultaneously initiating preparation for a cesarean de-livery in the event
that the operative vaginal delivery is unsuccessful.
Indications and Contraindications
No indication for operative
vaginal delivery is absolute. The following indications apply when the fetal
head is engaged and the cervix is fully dilated:
· Prolonged
or arrested second stage of labor
· Suspicion
of immediate or potential fetal compromise
· Shortening
of the second stage for maternal benefit
In certain situations, operative
vaginal delivery should be avoided or, at the least, carefully considered in
terms of rel-ative maternal and fetal risks. Most authorities consider vac-uum
extraction inappropriate in pregnancies before 34 weeks of gestation because of
the risk of fetal intraventricular hemorrhage. Operative delivery also is contraindicated if alive fetus is known to
have a bone demineralization condition (e.g., osteogenesis imperfecta) or has a
bleeding disorder (e.g., allo-immune thrombocytopenia, hemophilia, or von
Willebrand dis-ease), and if the fetal head is unengaged or the position of the
fetal head is unknown
Forceps
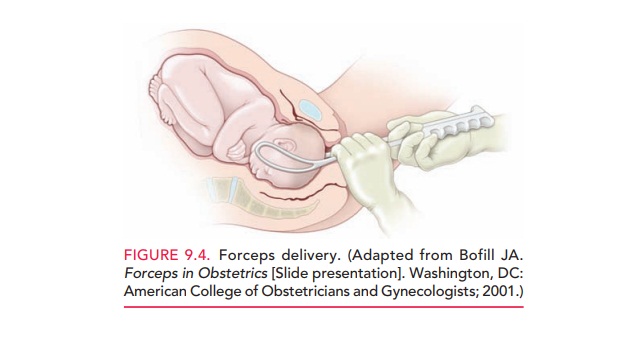
Forceps are
primarily used to apply traction to the fetalhead to augment the expulsive
forces, when the mother’s voluntary efforts in conjunction with uterine
contractions are insufficient to deliver the infant (Fig. 9.4). Occasionally,
forceps are used to rotate the fetal head before applying traction to complete
vaginal delivery. Forceps also may be used to control delivery of the fetal
head, thereby avoiding precipitous delivery. Different types of forceps are
available for the different degrees of molding of the fetal head.
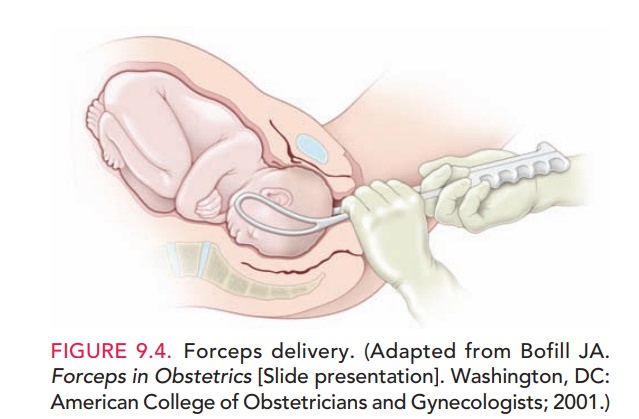
Maternal complications of forceps
delivery include per-ineal trauma, hematoma, and pelvic floor injury. Neonatal
risks include injuries to the brain and spine, musculoskeletal injury, and
corneal abrasion if the forceps are mistakenly ap-plied over the neonate’s
eyes. The risk of shoulder dysto-cia, in
which the fetus’s anterior shoulder becomes lodgedagainst the pubic symphysis,
is increased in forceps deliver-ies of infants weighing over 4000 g.
Vacuum Extraction
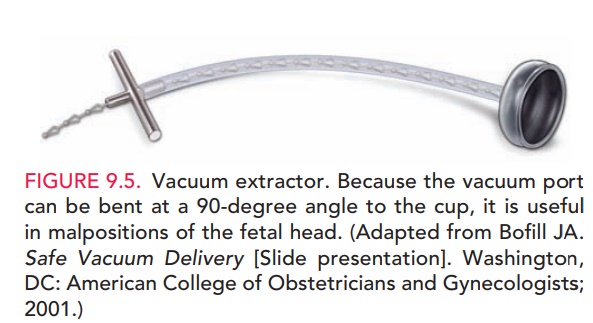
In vacuum extraction, a soft vacuum cup is applied to the fetal head
and suction is exerted by means of a mechanical pump (Fig. 9.5). Vacuum
extraction is associated with less maternal trauma than are forceps, but carries
significant neonatal risks. Although the amount of traction applied to the
fetal skull is less than that applied with forceps, it is still substantial and
can cause serious fetal injury. Neonatal risks include intracranial hemorrhage,
subgaleal hematomas, scalp lacerations (if torsion is excessive),
hyperbiliru-binemia, and retinal hemorrhage. In addition, separation of the
scalp from the underlying structures can lead to cephalohematoma. Overall, the incidence of serious
complica-tions with vacuum extraction is approximately 5%. It is
rec-ommended that rocking movements or torque not be applied to the device and
that only steady traction in the
Clinicians caring for the neonate should also be alerted that an
operative deliv-ery has been used so that they can monitor the neonate for
signs and symptoms of injury.
Related Topics