Chapter: Obstetrics and Gynecology: Abnormal Labor and Intrapartum Fetal Surveillance
Breech Presentation
BREECH PRESENTATION
Breech
presentation occurs in about 2% of singleton de-liveries at term
and more frequently in the early third and second trimesters. In addition to
prematurity, other condi-tions associated with breech presentation include
multiple pregnancy, polyhydramnios, hydrocephaly, anencephaly, aneuploidy,
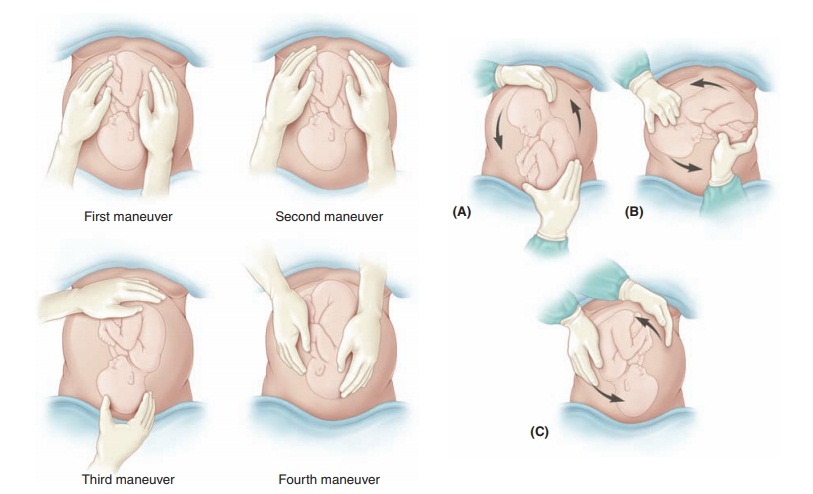
uterine anomalies, and uterine tumors. The three kinds of breech
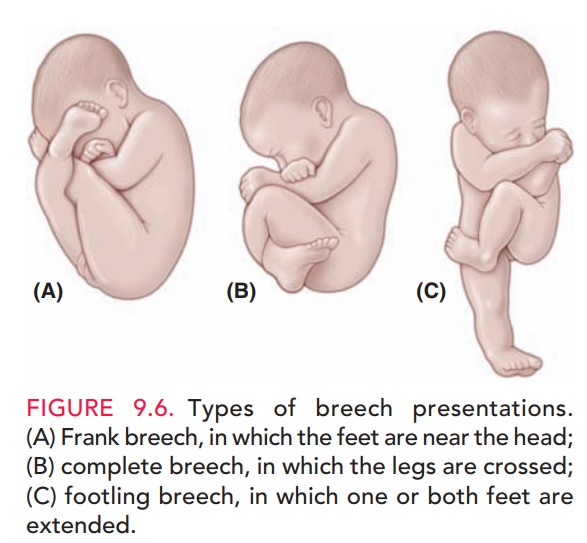
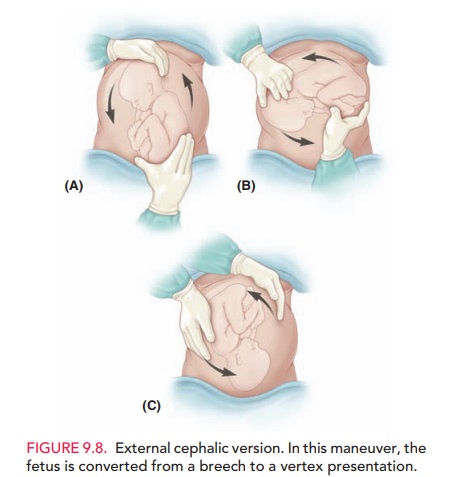
presentation—frank, complete, and incomplete breech (Fig. 9.6)—are diagnosed by
a combi-nation of Leopold maneuvers, pelvic examination, ultra-sonography, and
other imaging techniques (Fig. 9.7). Themorbidity
and mortality rates for mother and fetus, regardless of gestational age or mode
of delivery, are higher in the breech than in the cephalic presentation. This
increased risk to the fetuscomes from associated factors such as fetal
anomalies, prematurity, and umbilical cord prolapse, as well as birth trauma.
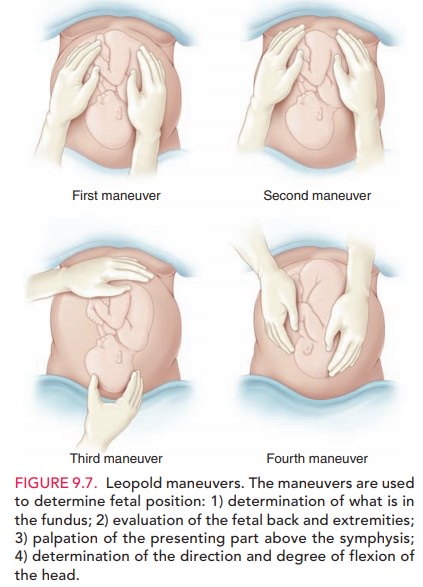
External cephalic version (ECV)
involves applyingpressure to the mother’s abdomen to turn the fetus in either a
forward or backward somersault to achieve a vertex pre-sentation prior to labor
(Fig. 9.8). The goal of ECV is to increase the proportion of vertex
presentations among fe-tuses that were formerly in the breech position near
term. Once a vertex presentation is achieved, the chances for a vaginal
delivery increase. This maneuver is
successful in ap-proximately half of properly selected cases. Patients who
havecompleted 36 weeks of gestation are preferred candidates for ECV for
several reasons. First, if spontaneous version is going to occur, it is likely
to have taken place by 36 com-pleted weeks of gestation. Second, risk of a
spontaneous reversion is decreased after external cephalic version at term
compared with earlier gestations. Selection
criteria in-clude a normal fetus with reassuring fetal heart tracing, ade-quate
amniotic fluid, presenting part not in the pelvis, and no uterine operative
scars. The risks include premature rup-ture of membranes, placental
abruption, cord accident, and uterine rupture. External version is more often
suc-cessful in parous women. Existing
evidence may support theuse of a tocolytic agent (a drug that stops uterine
contractions) during ECV attempts, particularly in nulliparous patients
Administration of anti-D immune
globulin to Rh negative women is recommended.
In light of recent studies that
further clarify the long-term risks of vaginal breech delivery, the decision
regard-ing mode of delivery should depend on the experience of the healthcare
provider. Cesarean delivery will be the
pre-ferred mode for most physicians because of the diminishing ex-pertise in
vaginal breech delivery. Planned vaginal delivery ofa term singleton breech
fetus may be reasonable under hospital-specific protocol guidelines for both
eligibility and labor management. The following criteria have been suggested
for vaginal breech delivery:
· Normal
labor curve
· Gestational
age greater than 37 weeks
· Frank or
complete breech presentation. Because of the risk of umbilical cord prolapse,
vaginal delivery of a fetus in the footling breech position is not recommended.
· Absence
of fetal anomalies on ultrasound examination
· Adequate
maternal pelvis
· Estimated
fetal weight between 2500 g and 4000 g
· Documentation
of fetal head flexion. Hyperextension of the fetal head occurs in about 5% of
term breech fetuses, requiring cesarean delivery to avoid head entrapment.
· Adequate
amniotic fluid volume (defined as a 3-cm ver-tical pocket)
· Availability
of anesthesia and neonatal support
If a vaginal breech delivery is
planned, the woman should be informed that the risk of perinatal or neonatal
mortality or short-term serious neonatal morbidity may be higher in it than in
a cesarean delivery, and the patient’s informed consent should be documented.
Related Topics