Chapter: Obstetrics and Gynecology: Abnormal Labor and Intrapartum Fetal Surveillance
Intrapartum Fetal Surveillance
INTRAPARTUM FETAL SURVEILLANCE
Evidence suggesting a nonreassuring fetal status during labor occurs in 5% to 10% of pregnancies. Intrapartumfetal surveillance is the indirect measurement of indica-tors of fetal status, such as fetal heart rate, blood gases, pulse rate, amniotic fluid volume, and fetal stimulation re-sponses, during labor. The goal of intrapartum fetal surveil-lance is to recognize changes in fetal oxygenation that could result in serious complications. However, it is now recognized thatmany neurologic conditions previously attributed to birthasphyxia (defined as a situation of damaging acidemia, hy-poxia, and metabolic acidosis) are in fact attributable to other causes not associated with labor, such as maternal infection, coagulation disorders, and autoimmune disorders; genetic causes; or low birth weight. Physicians should understand that intrapartum fetal surveillance is a tool for detection of events that occur during labor that could compromise fetal oxygenation and, in rare cases, lead to permanent neurologic disability.
Pathophysiology
The uteroplacental unit provides oxygen and nutrients to the fetus
while receiving carbon dioxide and wastes, the products of the normal aerobic
fetal metabolism. Uteroplacental
insufficiency occurs when the utero-placental unit is compromised. Initial
fetal responses include fetal hypoxia (decreased blood oxygen levels); shunting
of blood flow to the fetal brain, heart, and adrenal glands; and transient,
repetitive, late decelerations of the FHR. If hypoxia continues, the fetus will
eventually switch over to anaerobic glycolysis and develop meta-bolic acidosis.
Lactic acid accumulates and progressive damage to vital organs occurs,
especially the fetal brain and myocardium. If intervention is not timely,
serious and possibly permanent damage and sometimes death can result.
Neonatal
encephalopathy is a clinically defined syn-drome of disturbed
neurologic function in the earliest days of life in the term infant, manifested
by difficulty with initiating and maintaining respiration, depression of tone
and reflexes, subnormal level of consciousness, and some-times seizures.
Neonatal encephalopathy is not always as-sociated with permanent neonatal
neurologic impairment. Hypoxic-ischemic
encephalopathy (HIE) is a subtypeof neonatal encephalopathy for which the cause
is consid-ered to be limitation of oxygen and blood flow near the time of
birth. Historically, it has been assumed that most cases of neonatal
encephalopathy were hypoxic-ischemic encephalopathy, but epidemiologic studies
have estab-lished that this assumption is incorrect.
Approximately
70% of cases of neonatal encephalopathy are caused by factors that were present
before the onset of labor.
It is estimated that the
incidence of neonatal encephalop-athy caused by intrapartum hypoxia is
approximately 1.6/10,000, absent other coincident preconceptual or an-tepartum
abnormalities. HIE is thus one item in the larger category of encephalopathies
which may result from con-ditions such as prenatal stroke, prenatal infection,
genetic abnormalities, and neonatal cerebral malformation. The criteria
sufficient to suggest that an encephalopathy is as-sociated with an acute
intrapartum event are presented in Box 9.1.
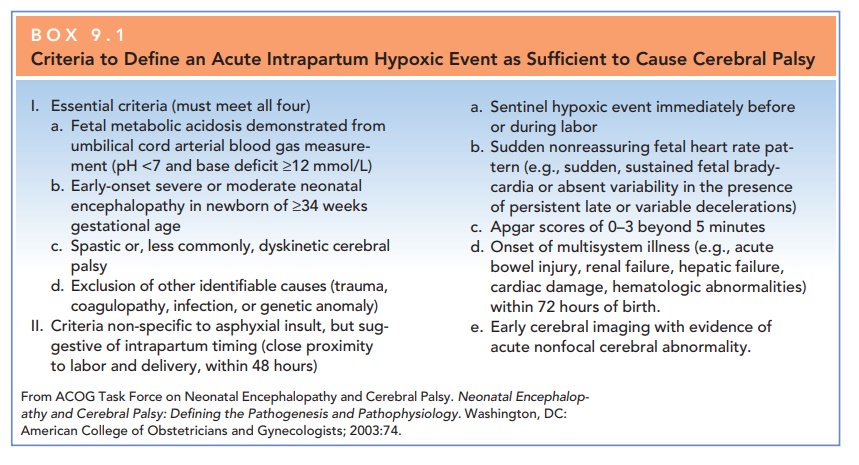
Cerebral palsy is a chronic disability of the centralnervous system (CNS) characterized by aberrant control of movement and posture appearing early in life and not as a result of progressive neurologic disease. Only one type of cerebral palsy, spastic quadriplegia, is associated with antepartum or intrapartum interruption of the fetal blood supply. Disorders not associated with intrapartum or peripartum asphyxia include dyskinetic or ataxic cere-bral palsy (which commonly has a genetic origin) and epilepsy, mental retardation, or attention-deficit hyper-activity disorders.
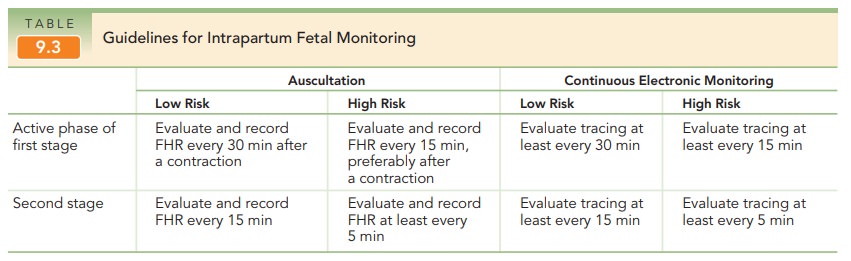
Intrapartum Fetal Heart Rate Monitoring
Fetal heart rate (FHR) monitoring is a modality in-tended to determine if a fetus is well-oxygenated. The ma-jority of neonates (approximately 85%) born in the United States are assessed with electronic fetal monitoring(EFM), making it the most common obstetric procedure. Intermittent auscultation of the FHR after a contractionalso is used to assess intrapartum fetal well-being. Beginning in the 1980s, EFM became more common; rates of its use have doubled over the past 35 years.
EFM may be performed externally
or internally. Most external monitors use a Doppler device with computerized
logic to interpret and count the Doppler signals. Internal FHR monitoring is
accomplished with a fetal electrode, which is a spiral wire placed directly on
the fetal scalp or other presenting part.
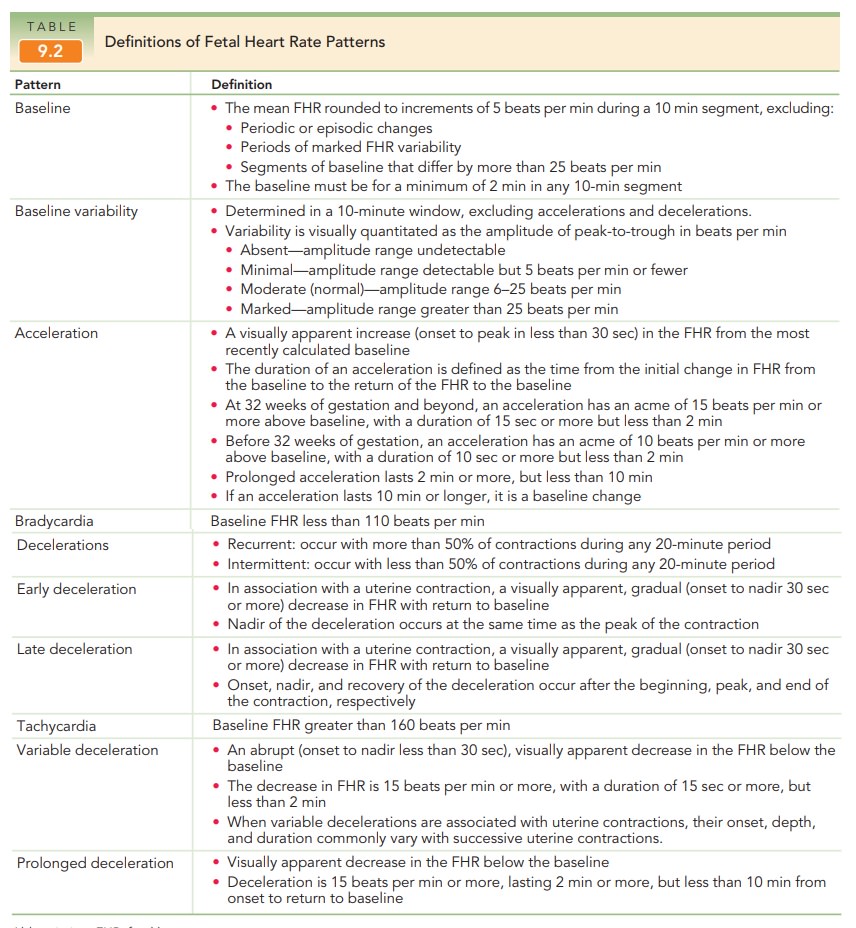
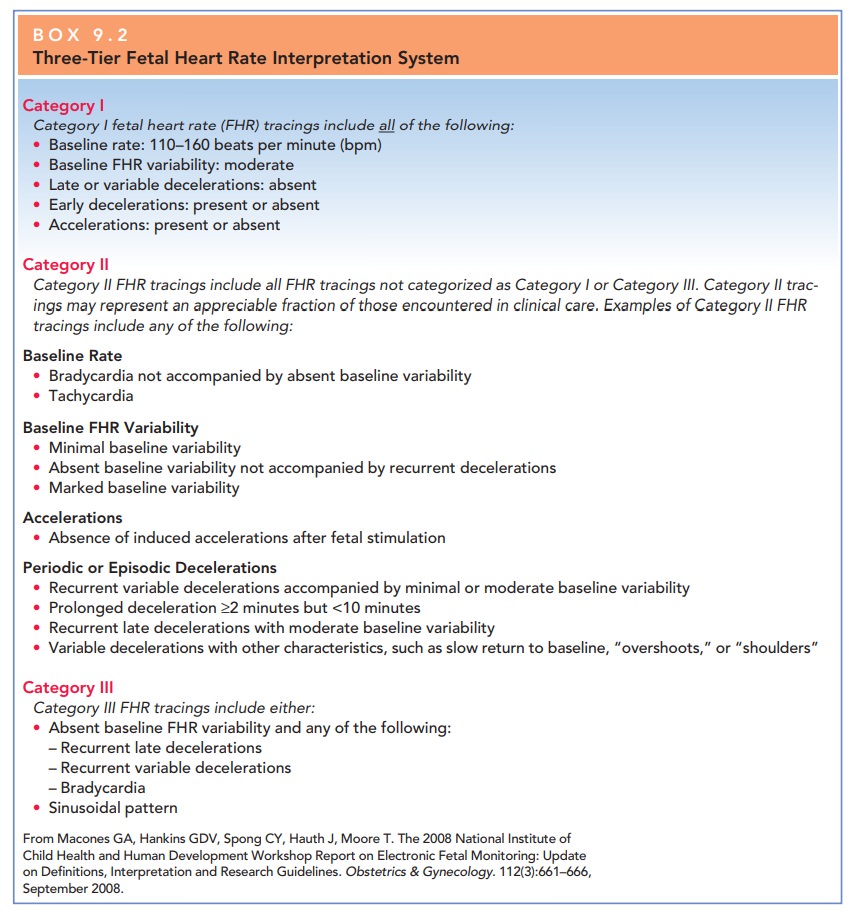
Fetal heart rates by EFM are described in terms of base-line rate, variability, presence of accelerations, periodic or episodic decelerations, and the changes in these character-istics over time (Table 9.2) and classified by a three-tier fetal heart rate interpretation system (Box 9.2). The goal of FHRmonitoring is to detect signs of fetal jeopardy in time to intervene before irreversible damage occurs. Despite the liberal use ofcontinuous EFM in both high-risk and low-risk patients, there has been no consistent decrease in the frequency of cerebral palsy in the last two decades. Fetuses who are se-verely asphyxiated during the intrapartum period will have abnormal heart rate patterns However, most patients with nonreassuring FHR patterns give birth to healthy infants. In addition, the false-positive rate of EFM for predicting adverse outcomes is high.
FETAL HEART RATE PATTERNS
The normal baseline FHR is
120–160 beats per minute (bpm). An FHR less than 120 beats per minute is
considered bradycardia. Fetal
bradycardia between 100 and 120 beatsper minute usually can be tolerated for
long periods when it is accompanied by normal FHR variability. An FHR be-tween
80–100 bpm is nonreassuring. An FHR that persists below 80 is an ominous sign
and may presage fetal death.
An FHR above 160 beats per minute
is considered tachycardia. The most
common cause of fetal tachycardiais chorioamnionitis, but it also may be due to
maternal fever, thyrotoxicosis, medication, and fetal cardiac arrhyth-mias.
Fetal tachycardia between 160 and 200 beats per minute without any other
abnormalities in FHR is usually well-tolerated.
FETAL HEART RATE VARIABILITY
Fetal heart rate variability refers to
the fluctuations in theFHR of two cycles or more, visually quantified as the
am-plitude of peak to trough in beats per minute. FHR is gradedaccording to amplitude range (see Table 9.3; Fig
9.10).
Moderate
variability is an assuring sign that reflects ade-quate fetal oxygenation and
normal brain function. In the presence of normal FHR variability, regardless of
what other FHR patterns exist, the fetus is not experiencing cerebral tissue
asphyxia.
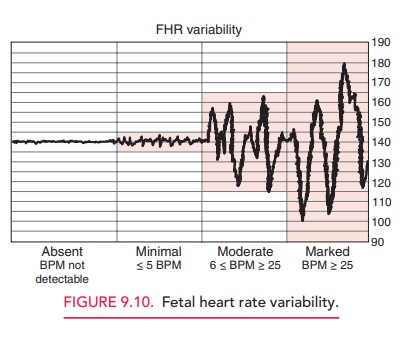
Decreased variability is
associated with fetal hypoxia, acidemia, drugs that may depress the fetal CNS
(e.g., ma-ternal narcotic analgesia), fetal tachycardia, fetal CNS and cardiac
anomalies, prolonged uterine contractions (uter-ine hypertonus), prematurity,
and fetal sleep.
PERIODIC FHR CHANGES
The FHR may vary with uterine
contractions by slowing or accelerating in periodic patterns. These periodic FHRchanges are classified as
accelerations or decelerations,based on whether they are increases or decreases
in the FHR and on their magnitude (in beats per minute).
Accelerations Accelerationsof the FHR are visually appar-ent increases (onset to peak in less
than 30 seconds) in the FHR from the most recently calculated baseline Accelerations aregenerally associated with reassuring fetal status
and an ab-sence of hypoxia and acidemia. Stimulation of the fetal scalp by
digital examination usually causes heart rate ac-celeration in the normal fetus
with an arterial fetal pH of >7.20 if delivery were to occur at the time of
measure-ment. For this reason, fetal scalp stimulation is sometime used as a
test of fetal well-being. External vibration stim-ulation, also termed vibroacoustic stimulation, elicits the
same response and is also used for this purpose (see “Ancillary Tests,” below).
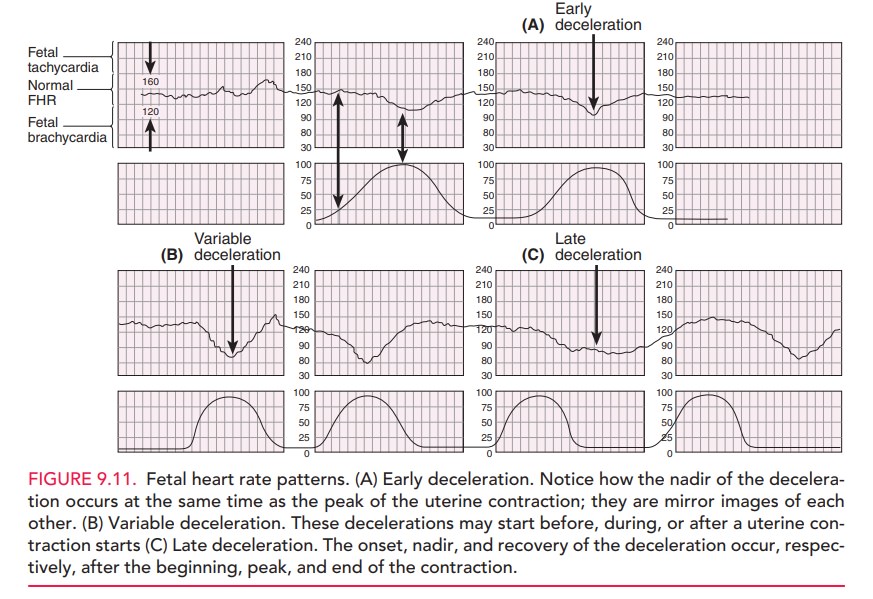
Decelerations Fetal heart ratedecelerationsare visuallyapparent
decreases in FHR from the baseline. They can beeither gradual (onset to nadir in 30 seconds or more)
or abrupt (onset to nadir in less than 30 seconds). Early de-celerations are associated with uterine contractions:
thenadir of the deceleration occurs at the same time as the peak of the uterine
contraction and, thus, is a “mirror image” of the contraction (Fig 9.11). Early
decelerations are the result of pressure on the fetal head from the birth
canal, digital examination, or forceps application that causes a reflex
response through the vagus nerve with acetylcholine release at the fetal
sinoatrial node. This response may be blocked with vagolytic drugs, such as
at-ropine. Early FHR decelerations are considered physio-logic, and are not a
cause of concern.
Late FHR
decelerations are visually apparent de-creases in the fetal heart
rate from the baseline fetal heart rate, associated with uterine contractions.
The onset, nadir, and recovery of the deceleration occur, respectively, after
the beginning, peak, and end of the contraction. Late decelerations are considered significantlynonreassuring,
especially when repetitive and associated with decreased variability. Late
decelerations are associatedwith uteroplacental insufficiency, as a result of
either decreased uterine perfusion or decreased placental func-tion, and thus
with decreased intervillous exchange of oxygen and carbon dioxide and
progressive fetal hypoxia and acidemia.
Variable FHR decelerations are abrupt, visually apparentdecreases in the fetal heart rate below the baseline fetal heart rate. These variable decelerations may start before, dur-ing, or after uterine contraction starts, hence the term “variable.” Variable decelerations are also mediated through the vagus nerve, with sudden and often erratic release of acetylcholine at the fetal sinoatrial node, resulting in their characteristic sharp deceleration slope. They are usually associated with umbilical cord compression, which may result from wrapping of the cord around parts of the fetus, fetal anomalies, or even knots in the umbilical cord. They are also commonly associated with oligohydramnios, in which the buffering space for the umbilical cord created by the amniotic fluid is lost. Variable decelerations are themost common periodic FHR pattern. They are often cor-rectable by changes in the maternal position to relieve pressure on the umbilical cord. Infusion of fluid into the amniotic cavity (amnioinfusion) to relieve umbilical cord compression in cases of oligohydramnios or when rupture of membranes has occurred, has been shown to be effec-tive in decreasing the rate of decelerations and cesarean delivery.
Ancillary Tests
Because the rate of
false-positive diagnosis of EFM is high, attempts have been made to find
ancillary tests that help confirm a nonreassuring FHR tracing.
FETAL STIMULATION
In the case of an EFM tracing
with decreased or absent variability without spontaneous accelerations, an
effort should be made to elicit one. Four techniques are avail-able to
stimulate the fetus: 1) fetal scalp sampling,
Allis clamp scalp stimulation, 3)
vibro-acoustic stim-ulation, and 4) digital scalp stimulation. Each of thesetechniques involves accessing
the fetal scalp through the di-lated cervix. In vibroacoustic stimulation,
the fetal scalp isstimulated with a vibratory device, and in digital scalp
stimulation, the physician uses his or her finger to gently stroke the scalp.
Each of these tests is a reliable
method to exclude aci-dosis if accelerations are noted after stimulation.
Because vibroacoustic stimulation and scalp stimulation are less in-vasive than
the other two methods, they are the preferred methods. When there is an
acceleration following stimu-lation, acidosis is unlikely and labor can
continue.
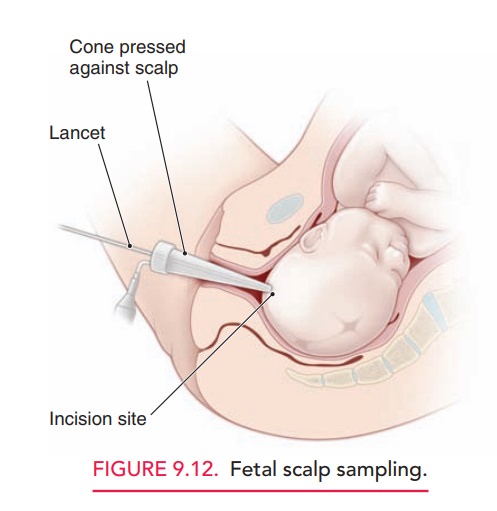
DETERMINATION OF FETAL BLOOD PH OR LACTATE
When a nonreassuring FHR tracing
persists without spon-taneous or stimulated accelerations, a scalp blood sample
for the determination of pH or lactate can be considered (Fig. 9.12). However,
the use of scalp pH has decreased, and it may not be available at some tertiary
hospitals. Furthermore, the positive predictive value of a low scalp pH to
identify a newborn with HIE is only 3%.
PULSE OXIMETRY
The use of pulse oximetry has
been suggested as a modality to reduce the false-positive diagnosis of a
non-reassuring FHR.
However, research has demonstrated that neither the overall rate of cesarean delivery nor the rate of umbilical arterial pH less than 7 decreased when pulse oximetry was used in association with EFM in cases of nonreassuring fetal status. Because of the uncertain ben-efit of pulse oximetry and concerns about falsely reassuring fetal oxygenation, use of the fetal pulse oximeter in clinical practice cannot be supported at this time. Additional stud-ies to test the efficacy and safety of fetal pulse oximetry are underway.
Diagnosis and Management of a Persistently Nonreassuring FHR Pattern
A reassuring FHR pattern
(Category I) may include a nor-mal baseline rate, moderate FHR variability,
persistence of accelerations, and absence of decelerations. Patterns believed
to be predictive of current or impending fetal as-phyxia (Category III) include
recurrent late decelerations, recurrent severe variable decelerations, or
sustained brady-cardia with absent FHR variability. A nonreassuring pattern
(Category II) is one that falls between these two extremes.
In the presence of a
nonreassuring FHR pattern, the etiology should be determined, if possible, and
an attempt should be made to correct the pattern by addressing the primary
problem. If the pattern persists, initial measures include changing the lateral
position to the left lateral po-sition, administering oxygen, correcting
maternal hypo-tension, and discontinuing oxytocin, if appropriate. Where the
pattern does not respond to change in position or oxy-genation, the use of
tocolytic agents has been suggested to abolish uterine contractions and prevent
umbilical cord compression. Uterine hyperstimulation can be identified by
evaluating uterine contraction frequency and duration and can be treated with
beta-adrenergic drugs. Amnio-infusion may also be used to prevent umbilical
cord com-pressions. Awaiting vaginal
delivery is appropriate if it has beendetermined that delivery is imminent. If
it is not, and there is evidence of progressive fetal hypoxia and acidosis,
cesarean delivery is warranted.
Related Topics