Chapter: Obstetrics and Gynecology: Abnormal Labor and Intrapartum Fetal Surveillance
Abnormal Labor
ABNORMAL LABOR
Abnormal
labor, or labor
dystocia (literally, “difficultlabor or childbirth”) is characterized by
the abnormal pro-gression of labor. Dystocia is the leading indication for
primary cesarean delivery in the United States. Despite thehigh prevalence of labor disorders, considerable variability
exists in the diagnosis, management, and criteria for dystocia that re-quires
intervention. Because dystocia can rarely be diag-nosed with certainty, the
relatively imprecise term “failure to progress” has been used, which includes
lack of pro-gressive cervical dilation or lack of descent of the fetal head or
both.
Factors That Contribute to Normal Labor— The Three Ps
Labor is the
occurrence of uterine contractions of suffi-cient intensity, frequency, and
duration to bring about demonstrable effacement and dilation of the cervix. Dystocia
results from what have been categorized classi-cally as abnormalities of the
“power” (uterine contractions or maternal expulsive forces), “passenger”
(position, size, or presentation of the fetus), or “passage” (pelvis or soft
tissues).
UTERINE CONTRACTIONS (“POWER”)
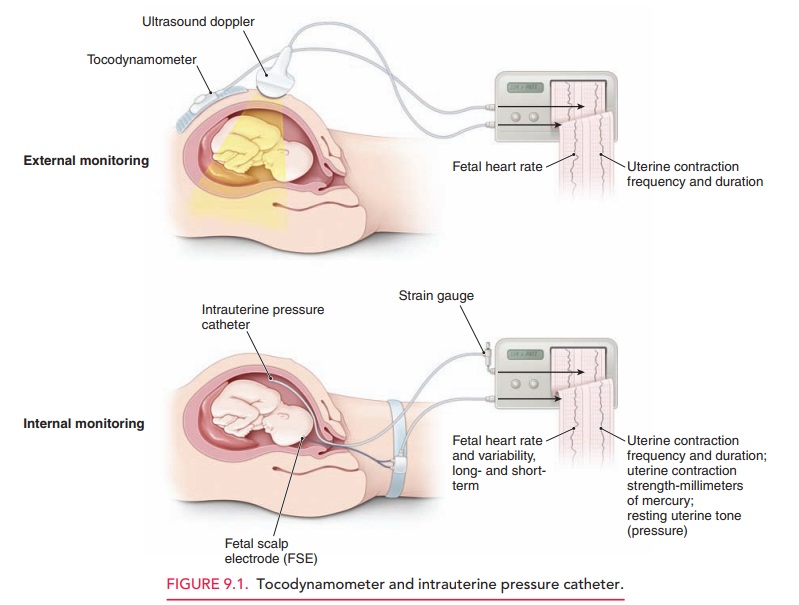
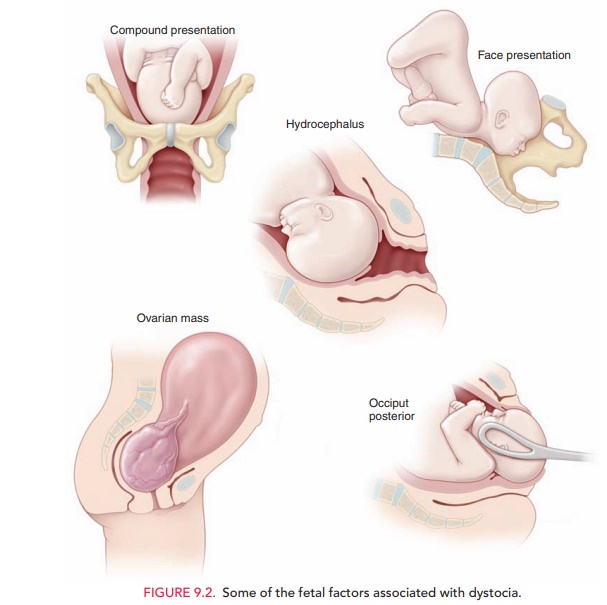
Uterine
activity can be monitored by palpation, external tocody-namometry, or by using
intrauterine pressure catheters (IUPCs) (Fig.
9.1). A tocodynamometer is an external strain gauge that is placed on the
maternal abdomen. It records the frequency of uterine contractions and
relaxations, as well as the duration of each contraction. An IUPC, in ad-dition
to recording contraction frequency and duration, also directly measures the
pressure generated by uterine contractions, via a catheter inserted into the
uterine cav-ity. The catheter is attached to a gauge that measures
intra-uterine pressure in millimeters of mercury (mm Hg).
Recent
studies suggest that the use of an IUPC instead of external tocodynamometry
does not affect the outcome in cases of abnormal labor.
However, an IUPC may be useful in
specific situations, such as maternal obesity or other factors that may prevent
accurate clinical evaluation of uterine contractions.
For cervical dilation and fetal
descent to occur, each uterine contraction must generate at least 25 mm Hg of
peak pressure. Optimal intrauterine pressure is 50 to 60 mm Hg. The frequency
of uterine contractions is also impor-tant in generating a normal labor
pattern: the optimal fre-quency of uterine contractions is a minimum of three
contractions in a 10-minute interval, often described as “adequate.” Uterine
contractions that are too frequent are not optimal, because they prevent
intervals of uterine re-laxation. During this “rest interval,” the fetus receives
unimpeded uteroplacental blood flow for oxygen and waste transport. Without
these rest periods, fetal oxygenation may be compromised.
Another unit of measure commonly
used to assess con-tractile strength is the Montevideo unit (MVU). This unit is the number of uterine
contractions in 10 minutes times the average intensity (above the resting
baseline intrauterine pressure). Normal
progress of labor is usually associated with 200or more Montevideo units.
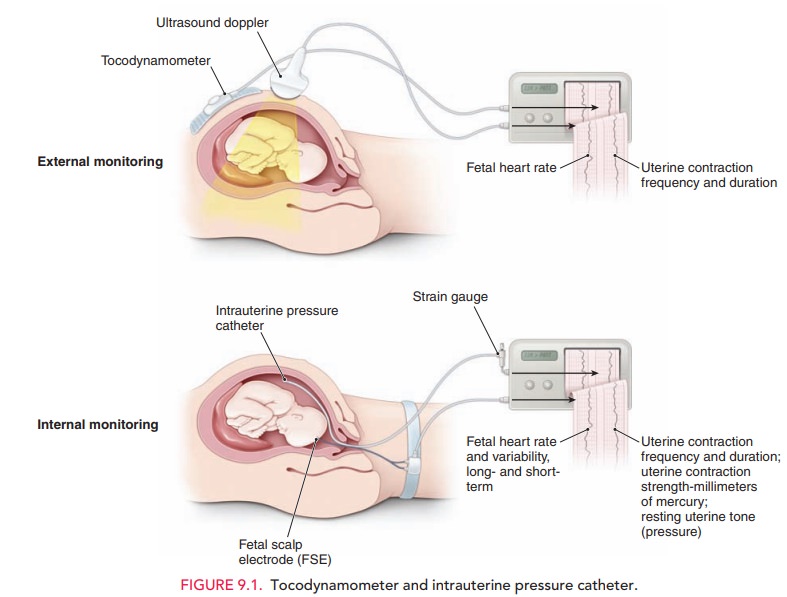
FETAL FACTORS (“PASSENGER”)
Evaluation of the passenger
includes clinical estimation of fetal weight and clinical evaluation of fetal
lie, presenta-tion, position, and attitude. If
a fetus has an estimated weightgreater than 4000 to 4500 grams, the risk of
dystocia, includ-ing shoulder dystocia and fetopelvic disproportion, is
greater. Because ultrasound estimation of fetal weight is often in-accurate
by as much as 500 to 1000 grams when the fetus is near term (40 weeks’
gestational age), this information must be used in conjunction with other
parameters when making management decisions.
Fetal
attitude, presentation, and lie also play a role in the progress of labor (Fig.
9.2). If the fetal head is asynclitic (turnedto one side; asynclitism) or extended (extension),
a larger cephalic diameter is presented to the pelvis, thereby increas-ing the
possibility of dystocia. A brow
presentation (about 1 in 3000 deliveries) typically converts to either a
vertex or face presentation, but, if persistent, may cause dystocia re-quiring
cesarean delivery. Likewise, a face
presentation (about 1 in 600 to 1000 deliveries) requires cesarean
deliv-ery in most cases. However, a mentum
anterior presenta-tion (chin toward mother’s abdomen) may be
deliveredvaginally if the fetal head undergoes flexion, rather than the normal
extension. A persistentoccipitoposterior positionis
alsoassociated with longer labors (approximately 1 hour in multiparous patients
and 2 hours in nulliparous patients). Incompoundpresentations, when one or more limbs prolapse alongsidethe
presenting part (about 1 in 700 deliveries), the extrem-ity usually retracts
(either spontaneously or with manual as-sistance) as labor continues. When it
does not, or in the 15% to 20% of compound presentations associated with
umbilical cord prolapse, cesarean delivery is required.
Fetal anomalies, such as
hydrocephaly and soft tissue tumors, may also cause dystocia. The routine use
of prena-tal ultrasound for other causes has allowed identification of these
situations, significantly reducing the incidence of un-expected dystocia of
this kind.
MATERNAL FACTORS (“PASSAGE”)
A number of maternal factors are
associated with dystocia. Dystocia can result from maternal skeletal or
soft-tissue anomalies that obstruct the birth canal. Cephalopelvicdisproportion, in which the size of the maternal
pelvis isinadequate to the size of the presenting part of the fetus, may impede
fetal descent into the birth canal.
Clinical,
radiographic, and CT measurements of the bony pelvis are poor predictors of
successful vaginal delivery, due to the inaccuracy of these measurements as
well as case-by-case differences in fetal accommodation and mechanisms of
labor.
Clinical
pelvimetry, the manual evaluation of the diam-eters of the
pelvis, is also a poor predictor of successful vaginal birth, except in rare
circumstances when the pelvic diameters are so small as to render the pelvis
“completely contracted.” Although radiographic and CT pelvimetry can be helpful
in some cases, the progress of descent of the presenting part in labor is the
best test of pelvic adequacy.
Soft-tissue causes of dystocia
include abnormalities of the cervix, tumors or other lesions of the colon or
adnexa, distended bladder, uterine fibroids, an accessory uterine horn, and
morbid obesity. Epidural anesthesia may con-tribute to dystocia by decreasing
the tone of the pelvic floor musculature.
Risks
Dystocia
may be associated with serious complications for both the woman and the fetus. Infection
(chorioamnionitis) is aconsequence of prolonged labor, especially in the
setting of ruptured membranes. Fetal infection and bacteremia, including
pneumonia caused by aspiration of infected amniotic fluid, is linked to
prolonged labor. In addition, there are the attendant risks of cesarean or
operative de-livery, such as maternal soft tissue injury to the lower genital
tract and fetal trauma
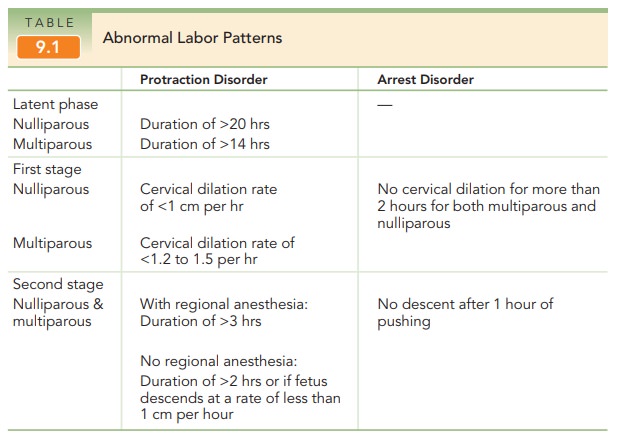
Diagnosis and Management of Abnormal Labor Patterns
Graphic documentation of
progressive cervical dilation and effacement facilitates assessing a patient’s
progress in labor and identifying abnormal labor patterns. The Friedman Curve
is commonly used for this purpose. Labor abnormalities can be categorized into
two general types: protraction disorders,
in which labor is slow to progress, and arrest
disorders, in which labor ceases to progress (Table 9.1). Protraction can
occur dur-ing both the latent and active phases of labor, while arrest is
recognized only in the active phase. Although the defi-nition of the latent phase of labor is controversial,
in gen-eral it can be defined as the phase in which the cervix effaces but
undergoes minimal dilation.
Management of abnormal labor
encompasses a wide range of options, from observation to operative or cesarean
delivery. Management choice depends on several factors:
·
Adequacy of uterine contractions
·
Fetal malposition or
cephalopelvic disproportion
·
Other clinical conditions, such
as nonreassuring fetal status or chorioamnionitis
Management decisions should be
balanced between ensur-ing a positive outcome for mother and fetus and avoiding
the concomitant risks of operative and cesarean delivery.
FIRST-STAGE DISORDERS
prolonged latent phase is one that exceeds 20 hours in
anulliparous patient or 14 hours in a multiparous patient. A pro-longed latent
phase does not necessarily predict an abnormal ac-tive phase of labor. Some
patients who have initially beendiagnosed as having a prolonged latent phase
are subse-quently found to have been in false labor. A prolonged la-tent phase
does not in itself pose a danger to the mother or fetus. Options for management
of women with a pro-longed latent phase of labor include observation and
seda-tion. With either of these options, the patient may stop having contractions,
in which case she is not in labor; may go into active labor; or may continue
experiencing pro-longed labor into the active phase. In the latter case, other
interventions as described below may be administered to augment uterine
contractions.
Once the patient is in active labor, the first stage is consid-ered prolonged when the cervix dilates less than 1 cm per hour in nulliparous women, and less than 1.2 to 1.5 cm per hour in multi-parous women. Management options for a prolonged firststage include observation, augmentation by amniotomy or oxytocin, and continuous support. Cesarean delivery usu-ally is warranted if maternal or fetal status becomes non-reassuring.
Augmentation Augmentationrefers to stimulation ofuterine contractions when spontaneous
contractions have failed to result in progressive cervical dilation or de-scent
of the fetus. Augmentation can be achieved with amniotomy (artificial rupture of membranes) or oxy-tocin
administration. Augmentation should be
consideredif the frequency of contractions is less than 3 contractions per 10
minutes or the intensity of contractions is less than 25 mm Hg above the
baseline or both. Before augmentation, the mater-nal pelvis and cervix as
well as fetal position, station, and well-being should be assessed. If there is
no evidence of disproportion, oxytocin can be used if uterine contractions are
judged to be inadequate. Contraindications to aug-mentation are similar to
those for labor induction .
If the
membranes have not ruptured, amniotomy may en-hance progress in the active
phase and negate the need for oxytocin augmentation. Amniotomy
allows the fetal head, rather thanthe otherwise intact amniotic sac, to be the
dilating force. It may also stimulate the release of prostaglandins, which
could aid in augmenting the force of contractions.
Amniotomy is usually performed with a thin, plastic rod with a sharp hook on the end. The end is guided to the open cervical os with the examiner’s fingers, and the hook is used to snag and disrupt the amniotic sac. Risks of amniotomy include fetal heart rate decelerations due to cord compression and an increased incidence of chorioamnionitis. For these reasons, amniotomy should not be routine and should be used for women with pro-longed labor. The fetal heart rate (FHR) should be eval-uated both before and immediately after rupture of the membranes.
It has
been shown that amniotomy combined with oxytocin administration early in the
active stage reduces labor by up to 2 hours, although there is no change in the
rate of cesarean delivery with this treatment protocol.
The goal of oxytocin
administration is to effect uterine ac-tivity sufficient to produce cervical
change and fetal de-scent while avoiding uterine hyperstimulation and fetal
compromise. Typically, a goal of a maximum of 5 contrac-tions in a 10-minute
period with resultant cervical dilation is considered adequate. Oxytocin may be
administered in low-dose or high-dose regimens. Low-dose regimens are associated
with a decreased incidence and severity of uterine hyperstimulation. High-dose
regimens are associated with decreased labor times, incidence of
chorioamnionitis, and cesarean delivery for dystocia.
Continuous Labor
Support Continuous support duringlabor from
caregivers (nurses, midwives, or lay individuals) may have a number of benefits
for women and their new-borns. Continuous care has been associated with reduced need for
pain relief and oxytocin administration, lower rates of cesarean and operative
deliveries, decreased incidence of 5-minute Apgar scores lower than 7, and
increased patient satisfaction with the labor experience. However, there are
insufficient data comparing differences in benefits on the basis of level of
training of support personnel—that is, whether the caregivers were nurses,
midwives, or doulas. There is no evidence of harmful effects from continuous
support during labor.
SECOND-STAGE DISORDERS
A
second-stage protraction disorder should be considered when the second stage
exceeds 3 hours if regional anesthesia has been ad-ministered, or 2 hours if no
regional anesthesia is used, or if the fetus descends at a rate of less than 1
cm per hour if no regional anesthesia is used. Second-stage arrest is diagnosed
when there is no descent after 1 hour of pushing. In the
past, the fetus wasthought to be at increased risk for morbidity and mortality
when the second stage exceeded 2 hours. Currently, more intensive intrapartum
surveillance provides the ability to identify the fetus that may not be
tolerating labor well.
Thus, the
length of the second stage of labor is not in itself an absolute or even a
strong indication for operative or cesarean delivery.
As long as heart tones continue
to be reassuring and cephalopelvic disproportion has been ruled out, it is
con-sidered safe to allow the second stage to continue. If uterine contractions
are inadequate, oxytocin adminis-tration can be initiated or the dosage
increased if already in place.
Bearing down efforts by the
patient in conjunction with uterine contractions help bring about delivery.
Labor positions other than the dorsal lithotomy position (e.g., knee-chest,
sitting, squatting, or birth-chair) may bring about subtle changes in fetal
presentation and facilitate vaginal delivery. Fetal accommodation may also be
facili-tated by allowing the effects of epidural analgesia to dissi-pate. The
absence of epidural analgesia may increase the tone of the pelvic floor
muscles, facilitating the cardinal movements of labor and restoring the urge to
push. In some cases of fetal malpresentation, manual techniques can facilitate
delivery. If the fetus is in the occipitoposte-rior position and does not
spontaneously convert to the nor-mal position, rotation can be performed to
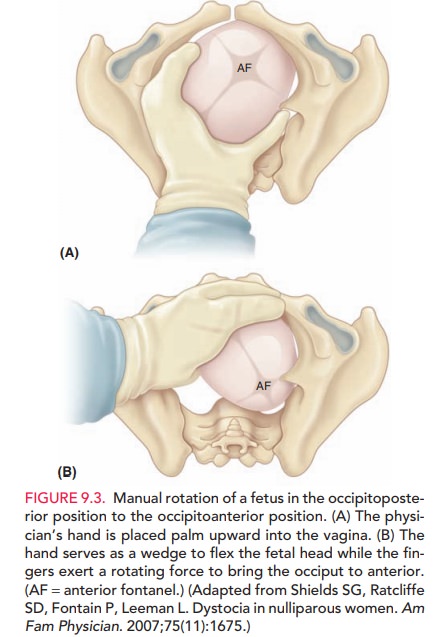
turn the fetus to the anterior position (Fig. 9.3).
The decision to perform an operative delivery in the second stage versus continued observation should be made on the basis of clinical assessment of the woman and the fetus and the skill and training of the obstetrician. Nonreassuring status of the fetus or mother is an indica-tion for operative or cesarean delivery.
Related Topics