Chapter: Obstetrics and Gynecology: Abnormal Labor and Intrapartum Fetal Surveillance
Intrapartum Fetal Heart Rate Monitoring
Intrapartum Fetal Heart Rate Monitoring
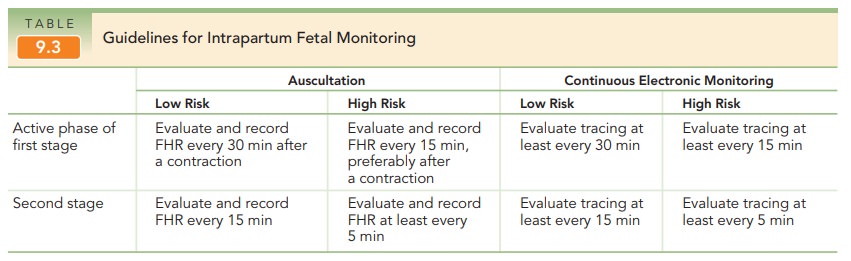
Fetal heart rate (FHR) monitoring is a modality in-tended to determine if a fetus is well-oxygenated. The ma-jority of neonates (approximately 85%) born in the United States are assessed with electronic fetal monitoring(EFM), making it the most common obstetric procedure. Intermittent auscultation of the FHR after a contractionalso is used to assess intrapartum fetal well-being. Beginning in the 1980s, EFM became more common; rates of its use have doubled over the past 35 years.
EFM may be performed externally
or internally. Most external monitors use a Doppler device with computerized
logic to interpret and count the Doppler signals. Internal FHR monitoring is
accomplished with a fetal electrode, which is a spiral wire placed directly on
the fetal scalp or other presenting part.
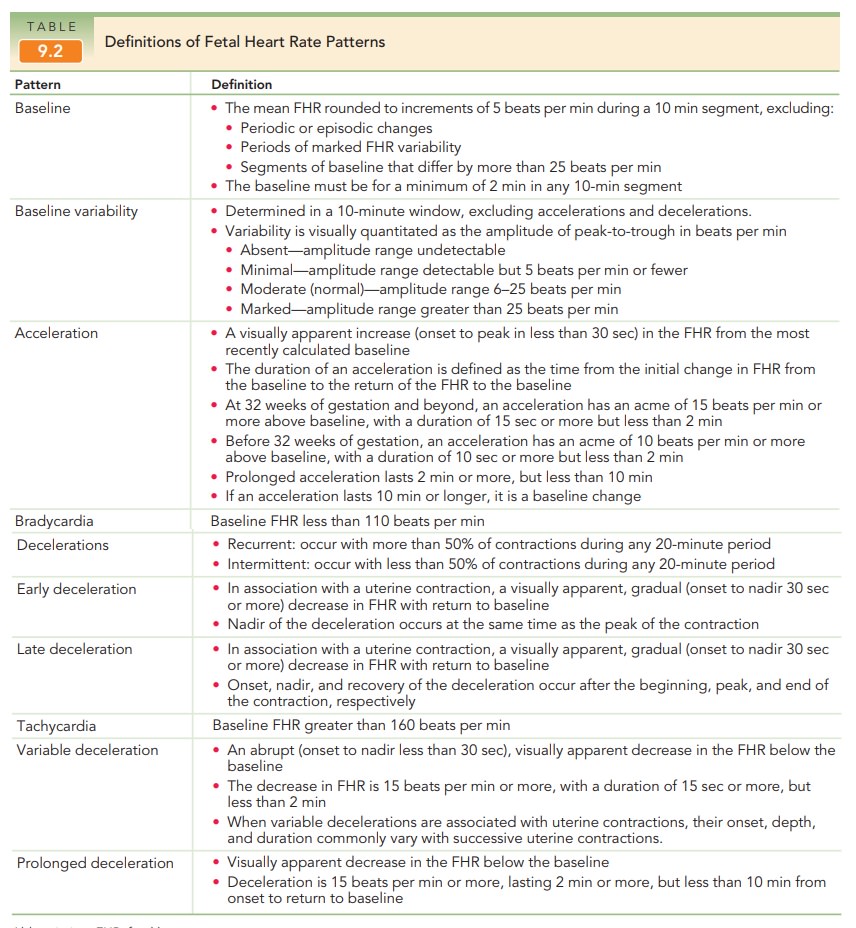
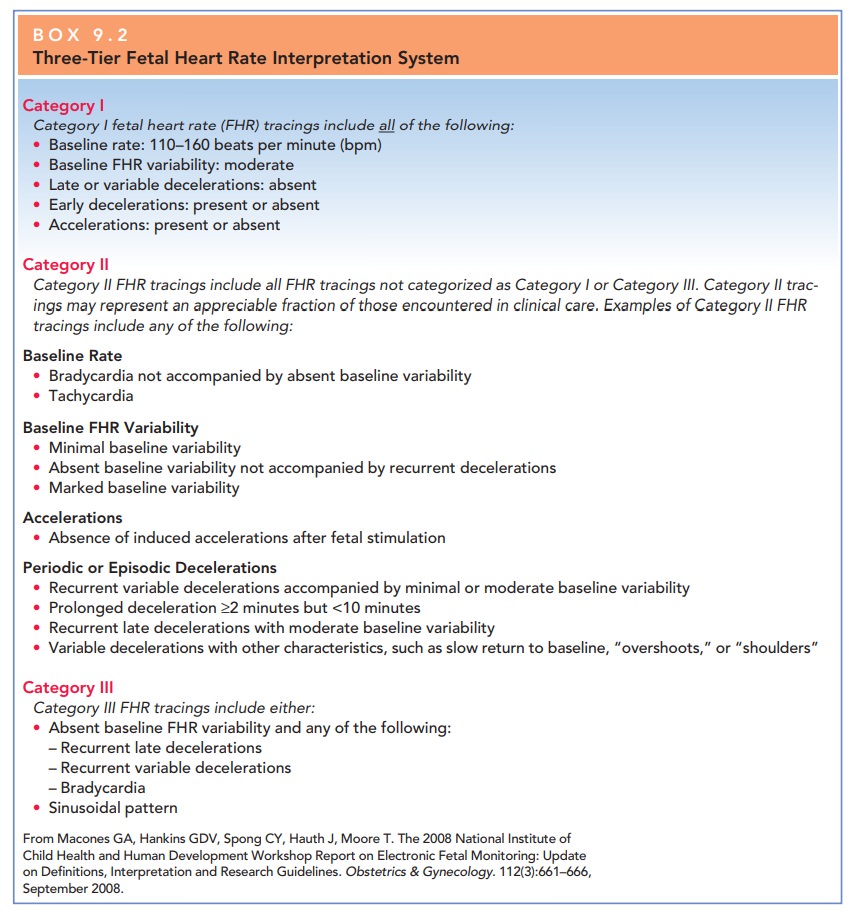
Fetal heart rates by EFM are
described in terms of base-line rate, variability, presence of accelerations,
periodic or episodic decelerations, and the changes in these character-istics
over time (Table 9.2) and classified by a three-tier fetal heart rate
interpretation system (Box 9.2). The goal
of FHRmonitoring is to detect signs of fetal jeopardy in time to intervene
before irreversible damage occurs. Despite the liberal use ofcontinuous EFM
in both high-risk and low-risk patients, there has been no consistent decrease
in the frequency of cerebral palsy in the last two decades. Fetuses who are
se-verely asphyxiated during the intrapartum period will have abnormal heart
rate patterns.
However,
most patients with nonreassuring FHR patterns give birth to healthy infants. In
addition, the false-positive rate of EFM for predicting adverse outcomes is
high
FETAL HEART RATE PATTERNS
The normal baseline FHR is
120–160 beats per minute (bpm). An FHR less than 120 beats per minute is
considered bradycardia. Fetal
bradycardia between 100 and 120 beatsper minute usually can be tolerated for
long periods when it is accompanied by normal FHR variability. An FHR be-tween
80–100 bpm is nonreassuring. An FHR that persists below 80 is an ominous sign
and may presage fetal death.
An FHR above 160 beats per minute
is considered tachycardia. The most
common cause of fetal tachycardiais chorioamnionitis, but it also may be due to
maternal fever, thyrotoxicosis, medication, and fetal cardiac arrhyth-mias.
Fetal tachycardia between 160 and 200 beats per minute without any other
abnormalities in FHR is usually well-tolerated.
FETAL HEART RATE VARIABILITY
Fetal heart rate variability refers to
the fluctuations in theFHR of two cycles or more, visually quantified as the
am-plitude of peak to trough in beats per minute. FHR is gradedaccording to amplitude range (see Table 9.3; Fig
9.10).
Moderate
variability is an assuring sign that reflects ade-quate fetal oxygenation and
normal brain function. In the presence of normal FHR variability, regardless of
what other FHR patterns exist, the fetus is not experiencing cerebral tissue
asphyxia.
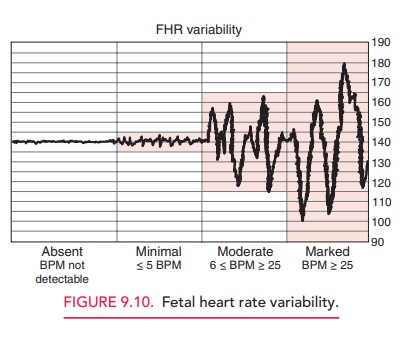
Decreased variability is
associated with fetal hypoxia, acidemia, drugs that may depress the fetal CNS
(e.g., ma-ternal narcotic analgesia), fetal tachycardia, fetal CNS and cardiac
anomalies, prolonged uterine contractions (uter-ine hypertonus), prematurity,
and fetal sleep
PERIODIC FHR CHANGES
The FHR may vary with uterine
contractions by slowing or accelerating in periodic patterns. These periodic FHRchanges are classified as
accelerations or decelerations,based on whether they are increases or decreases
in the FHR and on their magnitude (in beats per minute).
Accelerations Accelerationsof the FHR are visually appar-ent increases (onset to peak in less
than 30 seconds) in the FHR from the most recently calculated baseline Accelerations aregenerally associated with reassuring fetal status
and an ab-sence of hypoxia and acidemia. Stimulation of the fetal scalp by
digital examination usually causes heart rate ac-celeration in the normal fetus
with an arterial fetal pH of >7.20 if delivery were to occur at the time of
measure-ment. For this reason, fetal scalp stimulation is sometime used as a
test of fetal well-being. External vibration stim-ulation, also termed vibroacoustic stimulation, elicits the
same response and is also used for this purpose (see “Ancillary Tests,” below).
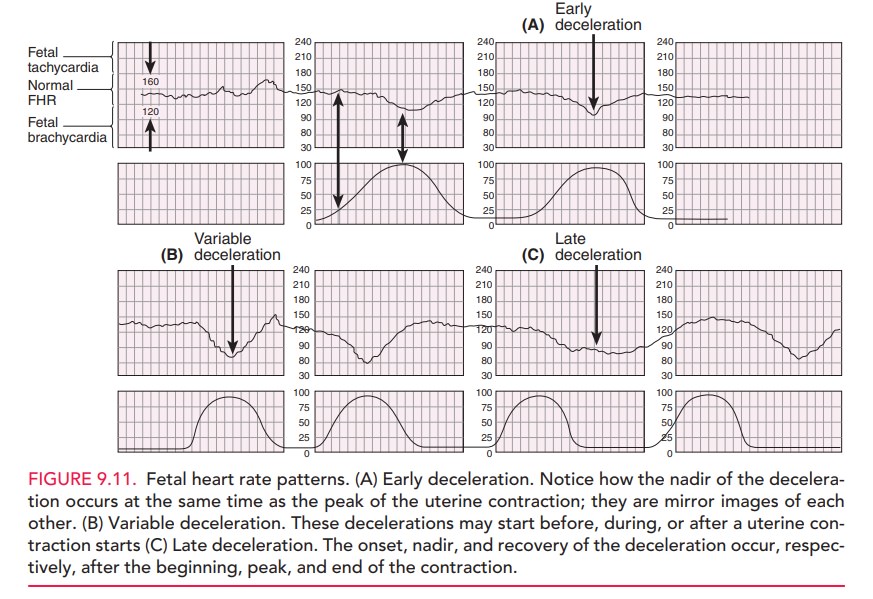
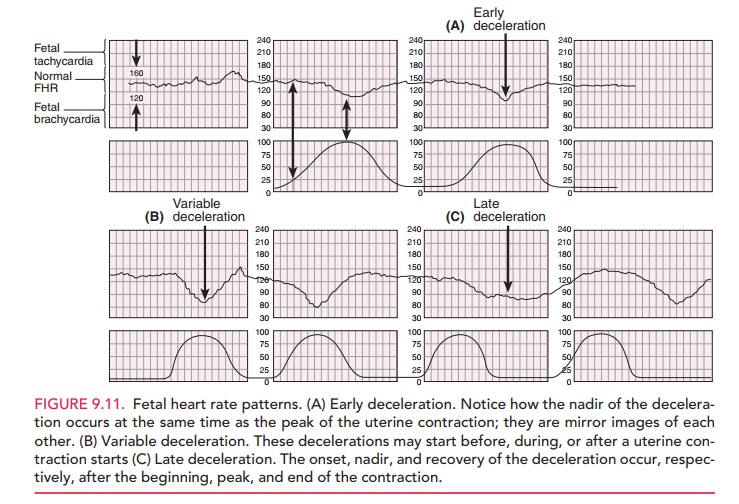
Decelerations Fetal heart ratedecelerationsare visuallyapparent
decreases in FHR from the baseline. They can beeither gradual (onset to nadir in 30 seconds or more)
or abrupt (onset to nadir in less than 30 seconds). Early de-celerations are associated with uterine contractions:
thenadir of the deceleration occurs at the same time as the peak of the uterine
contraction and, thus, is a “mirror image” of the contraction (Fig 9.11). Early
decelerations are the result of pressure on the fetal head from the birth
canal, digital examination, or forceps application that causes a reflex
response through the vagus nerve with acetylcholine release at the fetal
sinoatrial node. This response may be blocked with vagolytic drugs, such as
at-ropine. Early FHR decelerations are considered physio-logic, and are not a
cause of concern.
Late FHR
decelerations are visually apparent de-creases in the fetal heart
rate from the baseline fetal heart rate, associated with uterine contractions.
The onset, nadir, and recovery of the deceleration occur, respectively, after
the beginning, peak, and end of the contraction. Late decelerations are considered significantlynonreassuring,
especially when repetitive and associated with decreased variability. Late
decelerations are associatedwith uteroplacental insufficiency, as a result of
either decreased uterine perfusion or decreased placental func-tion, and thus
with decreased intervillous exchange of oxygen and carbon dioxide and
progressive fetal hypoxia and acidemia.
Variable FHR decelerations are abrupt, visually
apparentdecreases in the fetal heart rate below the baseline fetal heart rate. These
variable decelerations may start before, dur-ing, or after uterine contraction
starts, hence the term “variable.” Variable decelerations are also mediated
through the vagus nerve, with sudden and often erratic release of acetylcholine
at the fetal sinoatrial node, resulting in their characteristic sharp
deceleration slope. They are usually associated with umbilical cord
compression, which may result from wrapping of the cord around parts of the
fetus, fetal anomalies, or even knots in the umbilical cord. They are also
commonly associated with oligohydramnios, in which the buffering space for the
umbilical cord created by the amniotic fluid is lost. Variable decelerations are themost common periodic FHR pattern. They
are often cor-rectable by changes in the maternal position to relieve pressure
on the umbilical cord. Infusion of fluid into the amniotic cavity (amnioinfusion) to relieve umbilical
cord compression in cases of oligohydramnios or when rupture of membranes has
occurred, has been shown to be effec-tive in decreasing the rate of
decelerations and cesarean delivery.
Related Topics