Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Nursing Process: Postoperative Care of the Patient Undergoing Orthopedic Surgery
NURSING PROCESS: POSTOPERATIVE
CARE OF THE PATIENT UNDERGOING ORTHOPEDIC SURGERY
Assessment
After orthopedic
surgery, the nurse continues the preoperative care plan, modifying it to match
the patient’s current postoperative sta-tus. The nurse reassesses the patient’s
needs in relation to pain, neurovascular status, health promotion, mobility,
and self-esteem. Skeletal trauma and surgery performed on bones, muscles, or joints
can produce significant pain, especially during the first 1 or 2 postoperative
days. Tissue perfusion must be monitored closely, because edema and bleeding
into the tissues can compromise cir-culation and result in compartment
syndrome. Inactivity con-tributes to venous stasis and the development of DVT.
General anesthesia, analgesia, and immobility can result in altered
func-tioning of respiratory, gastrointestinal, and urinary systems.
The nurse notes the
prescribed limits on mobility and as-sesses the patient’s understanding of the
mobility restrictions. Thenurse discusses the plan of care with the patient and
encourages active participation in the plan.
In addition, the nurse assesses and monitors the patient
for po-tential problems related to the surgery. Frequent assessment of vital
signs, level of consciousness, neurovascular status, wound drainage, breath
sounds, bowel sounds, fluid balance, and pain provides the nurse with data that
may suggest the possible devel-opment of complications. The nurse reports
abnormal findings to the physician promptly.
With major orthopedic
surgery, there is a risk of hypovolemic shock because of blood loss. Muscle
dissection frequently produces wounds in which hemostasis is poor. Wounds that
are closed under tourniquet control may bleed during the postoperative period.
The nurse must be alert for signs of hypovolemic shock.
Changes in the patient’s
pulse rate, respiratory rate, or color may indicate pulmonary or cardiovascular
complications. Atelectasis and pneumonia are common and may be related to
preexisting pul-monary disease, deep anesthesia, decreased activity,
analgesics, and reduced respiratory reserve due to advanced age or an
underlying musculoskeletal disorder (eg, restrictive lung expansion secondary
to kyphosis, rheumatoid arthritis, or osteoporosis).
Voiding in unnatural positions may contribute to urinary
re-tention. In addition, elderly men usually have some degree of prostate
enlargement and may already have difficulty voiding. Therefore, it is important
to monitor urinary output.
Temperature elevations
within the first 48 hours are frequently related to atelectasis or other
respiratory problems. Temperature elevations during the next few days are
frequently associated with urinary tract infections. Superficial wound
infections take 4 to 6 days to develop. Fever from phlebitis usually occurs
during the end of the first week through the second week.
Thromboembolic disease is one of the most common and most
dangerous of all complications oc-curring in the postoperative orthopedic
patient. Advanced age, venous stasis, lower extremity orthopedic surgery, and
immobi-lization are significant risk factors. The nurse assesses the patient
daily for calf swelling, tenderness, warmth, redness, and a posi-tive Homans’
sign. The nurse promptly reports abnormal find-ings to the physician.
In addition, fat embolus
may occur with ortho-pedic surgery. The nurse must be alert to changes
in respiration, behavior, and level of consciousness that suggest the development
of fat embolus.
Nursing Diagnosis
Based on all assessment data, the patient’s major nursing
diag-noses after orthopedic surgery may include the following:
·
Acute pain related to the
surgical procedure, swelling, and immobilization
·
Risk for peripheral
neurovascular dysfunction related to swelling, constricting devices, or
impaired circulation
·
Risk for ineffective
therapeutic regimen management related to insufficient knowledge or available
support and resources
·
Impaired physical mobility
related to pain, edema, or the presence of an immobilizing device (eg, splint,
cast, or brace)
·
Risk for situational low
self-esteem: disturbed body image or role performance related to impact of
musculoskeletal problem
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications may
in-clude the following:
·
Hypovolemic shock
·
Atelectasis; pneumonia
·
Urinary retention
·
Infection
·
Venous stasis and DVT
Planning and Goals
The major goals for the patient after orthopedic surgery
may in-clude relief of pain, adequate neurovascular function, health
pro-motion, improved mobility, positive self-esteem, and absence of
complications.
Nursing Interventions
RELIEVING PAIN
After orthopedic surgery, pain can be intense. Edema,
hematomas, and muscle spasms contribute to the pain experienced. Some pa-tients
report that the pain is less than that experienced preopera-tively, and only
moderate amounts of analgesics are needed. The nurse closely monitors the
patient’s pain level and response to therapeutic measures and makes every
effort to relieve the pain and discomfort.
Multiple pharmacologic approaches to pain management
exist. Patient-controlled analgesia (PCA) and epidural analgesia may be
prescribed to control the pain. If intramuscular and oral anal-gesics are
prescribed on an as-needed basis (PRN), the nurse in-structs the patient to
request the analgesic before the pain becomes severe. Alternatively, the nurse
can offer the medication at set intervals. The nurse rotates intramuscular
injection sites, avoid-ing the operative hip and thigh. The nurse may
administer med-ications on a preventive basis within the prescribed intervals
if the onset of pain can be predicted (eg, 30 minutes before planned ac-tivity
such as transfer or exercise).
In addition to pharmacologic approaches to controlling
pain, elevation of the operative extremity and application of cold, if
prescribed, help to control edema and pain. Portable suction of the wound
decreases fluid accumulation and hematoma forma-tion. The nurse may find that
repositioning, relaxation, distrac-tion, and guided imagery help in reducing
the patient’s pain.
The nurse should report increasing and uncontrollable
pain to the orthopedic surgeon for evaluation. Pain should diminish rapidly after
the initial postoperative period. After 2 to 3 days, most patients require only
occasional oral analgesia for residual muscle soreness and spasm.
MAINTAINING ADEQUATE NEUROVASCULAR FUNCTION
The nurse continues the preoperative plan of care. The
nurse monitors the neurovascular status of the involved body part and notifies
the physician promptly of any indications of diminished tissue perfusion. The
patient is reminded to perform muscle-setting, ankle, and calf-pumping
exercises hourly while awake to enhance circulation.
MAINTAINING HEALTH
The nurse continues the
preoperative plan of care. It is important to encourage the patient to
participate in the postoperative treat-ment regimen.well-balanced diet with
adequate protein and vitamins is needed for wound healing. The patient
progresses to a regular diet as soon as possible. Large amounts of milk should
not be given to orthopedic patients who are on bed rest, however, be-cause this
adds to the calcium pool in the body and requires that the kidneys excrete more
calcium, which increases the risk for urinary calculi.
The nurse monitors the patient for pressure ulcers, which
are a threat to any patient who must spend an extended time in bed or who is
elderly, malnourished, or unable to move without as-sistance. Turning, washing,
and drying the skin and minimiz-ing pressure over bony prominences are
necessary to avoid skin breakdown.
IMPROVING PHYSICAL MOBILITY
Patients are frequently reluctant to move after
orthopedic surgery. Preoperative education about the planned postoperative
treat-ment regimen promotes patient participation in physical activi-ties.
Patients often increase their mobility once they have been reassured that
movement within therapeutic limits is beneficial, that the nurse will provide assistance,
and that discomfort can be controlled.
Metal pins, screws,
rods, and plates used for internal fixation are designed to maintain the
position of the bone until ossifi-cation occurs. They are not designed to
support the body’s weight, and they can bend, loosen, or break if stressed. The
es-timated strength of the bone, the stability of the fracture, re-duction and
fixation, and the amount of bone healing are important considerations in
determining weight-bearing limits. Although the incision may appear healed, the
underlying bone requires more time to repair and regain normal strength. Some
orthopedic procedures require weight-bearing restrictions. The or-thopedic
surgeon will prescribe the weight-bearing limits and the use of protective
devices (orthoses), if necessary, after surgery.
The physical therapist tailors the exercise program to
the in-dividual patient’s needs. The goal is the patient’s return to the
highest level of function in the shortest time possible. Rehabili-tation
involves progressive increases in the patient’s activities and exercises.
Assistive devices (crutches, walker) may be used for postoperative mobility.
Preoperative practice with assistive de-vices helps the patient use them
postoperatively. The nurse makes sure that the patient uses these devices
safely.
MAINTAINING SELF-ESTEEM
The nurse continues the preoperative plan of care. The
nurse and the patient set realistic goals. Increased self-care activities
within the limits of the therapeutic regimen and resumption of roles facilitate
recognition of abilities and promote self-esteem, personal identity, and role
performance. Acceptance of altered body image is facilitated by support
provided by the nurse, family, and others.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Hypovolemic Shock
Excessive loss of blood
during or after surgery can result in shock. The nurse monitors the patient for
signs and symptoms of hypo-volemic shock: increased pulse rate, decreased blood
pressure, urine output less than 30 mL per hour, restlessness, change in
mentation, thirst, decreased hemoglobin and hematocrit. The nurse reports these
findings to the orthopedic surgeon and assistsin appropriate
management.
Atelectasis and Pneumonia
The nurse monitors the patient’s breath sounds and encourages
deep breathing and coughing exercises. Full expansion of the lungs prevents the
accumulation of pulmonary secretions and the development of atelectasis and
pneumonia. Incentive spirometry, if prescribed, is encouraged. If signs of
respiratory problems de-velop (eg, increased respiratory rate, productive
cough, dimin-ished or adventitious breath sounds, fever), the nurse reports the
findings to the surgeon.
Urinary Retention
The nurse closely
monitors the patient’s urinary output after surgery. The nurse encourages the
patient to void every 3 to 4 hours to prevent urinary retention and bladder
distention. It is important to provide privacy during toileting. Because the
patient may need to void in an unusual position, the nurse assists the pa-tient
with positioning. Fracture bedpans may be more comfortable than other bedpans.
Voiding in the side-lying position may be helpful to the male patient. Some
male patients can void only if standing, and clarification with the surgeon of
the activity pre-scription may be needed before the patient is assisted to a
standing position. If the patient is unable to void, intermittent
catheteriza-tions may be prescribed until the patient is able to void
indepen-dently. Indwelling urinary catheters are to be used only when absolutely
necessary and should be removed as soon as possible.
Infection
Infection is a risk
after any surgery, but it is of particular concern for the postoperative
orthopedic patient because of the high risk of osteomyelitis. Osteomyelitis
often requires prolonged courses of intravenous antibiotics. At times, the
infected bone and pros-thesis or internal fixation device must be surgically
removed. Therefore, prophylactic systemic antibiotics are usually prescribed
during the perioperative and immediate postoperative period. The nurse assesses
the patient’s response to these antibiotics. When changing dressings and
emptying wound drainage devices, aseptic technique is essential. The nurse
monitors the patient’s vital signs, incision, and drainage. The nurse monitors
the patient for signs of urinary tract infection. Prompt assessment for and
treatment of infection are essential.
Venous Stasis and Deep Vein Thrombosis
Prevention of DVT requires use of ankle and calf-pumping
ex-ercises, elastic compression stockings, and sequential compres-sion devices.
Adequate hydration and early mobilization are equally important. Prophylactic
warfarin, adjusted-dose heparin, or low-molecular-weight heparin (eg,
enoxaparin sodium) may be prescribed. Aspirin has no apparent effect in
preventing DVT in the orthopedic patient. The nurse monitors the patient for
signs of DVT and promptly reports findings to the physician for management.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching the Patient Self-Care
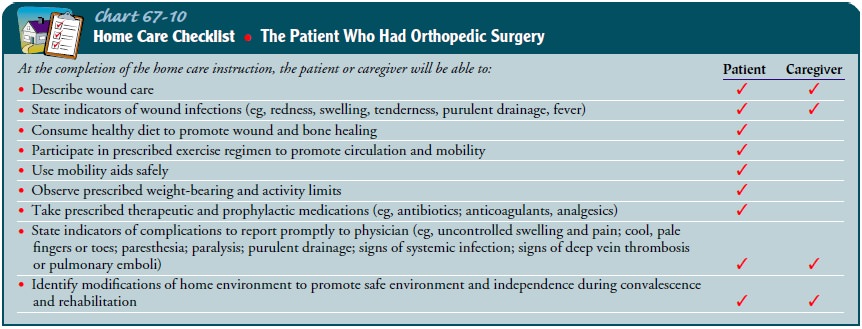
The length of stay in the hospital after orthopedic surgery is usu-ally less than 1 week. Convalescence and rehabilitation take place at home or in a nonacute care setting. The nurse teaches the pa-tient and the family to recognize complications that must be re-ported promptly to the orthopedic surgeon.
The patient must understand the prescribed medication regimen. The nurse
should demonstrate proper wound care. The patient gradually resumes physical
activities and adheres to weight-bearing limits. The pa-tient must be able to
perform transfers and to use mobility aids safely. If the patient has a cast or
other immobilizing device, fam-ily members should be instructed about how to
assist the patient in a way that is safe for the patient and for the family
member (eg, using proper body mechanics when lifting the patient). Specific
exercises need to be taught and practiced before discharge. The nurse discusses
recovery and health promotion, emphasizing a healthy lifestyle and diet.
Continuing Care
If special equipment or home modifications are needed for
safe care at home, they must be obtained before the patient is dis-charged
home. The nurse, physical therapist, and social worker can assist the patient
and family in identifying their needs and in getting ready to care for the
patient at home.
Frequently, home health
nursing and home physical therapy are part of the discharge plan of care. These
referrals provide re-sources and help the patient and the family cope with the
de-mands of care during convalescence and rehabilitation. The nurse can explore
problems that the patient and family identify during the home care visit. The
nurse assesses the patient’s progress and monitors for possible complications.
Regular medical follow-up care after discharge needs to be arranged (Chart
67-10).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Reports
decreased level of pain
a) Uses
multiple approaches to reduce pain
b) Uses
occasional oral medication to control discomfort
c) Elevates
extremity to control edema and discomfort
d) Moves
with greater comfort
2) Exhibits
adequate neurovascular function
a) Exhibits
normal color and temperature of skin
b) Has
warm skin
c) Has
normal capillary refill response
d) Demonstrates
intact sensory and motor function
e) Demonstrates
reduced swelling
3)Promotes
health
a) Eats
diet appropriate for nutritional needs
b) Maintains
adequate hydration
c) Abstains
from smoking
d) Practices
respiratory exercises
e) Repositions
self to relieve pressure on skin
f) Engages
in strengthening and preventive exercises
4)Maximizes
mobility within the therapeutic limits
a) Requests
assistance when moving
b) Elevates
edematous extremity after transfer
c) Uses
immobilizing devices as prescribed
d) Complies
with prescribed weight-bearing limitation
5)Expresses
positive self-esteem
a) Discusses
temporary or permanent changes in body image
b) Discusses
role performances
c) Views
self as capable of assuming responsibilities
d) Actively
participates in planning care and in the thera-peutic regimen
6)Exhibits
absence of complications
a) Does
not experience shock
b) Maintains
normal vital signs and blood pressure
c) Has
clear lung sounds
d) Demonstrates
wound healing without signs of infection
e) Does
not experience urinary retention
f) Voids
clear urine clear
g) Exhibits
no signs of DVT
Related Topics