Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Nursing Process: The Patient in a Cast
NURSING PROCESS:THE PATIENT IN A CAST
Assessment
Before the cast is applied, the nurse completes an
assessment of the patient’s general health, presenting signs and symptoms,
emo-tional status, understanding of the need for the cast, and condi-tion of
the body part to be immobilized in the cast. Physical assessment of the part to
be immobilized must include assessment of the neurovascular status (neurologic and circulatory func-tioning) of
the body part, degree and location of swelling, bruis-ing, and skin abrasions.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, major nursing diagnoses for
the pa-tient with a cast may include the following:
·
Deficient knowledge related to
the treatment regimen
·
Acute pain related to the
musculoskeletal disorder
·
Impaired physical mobility
related to the cast
·
Self-care deficit:
bathing/hygiene, feeding, dressing/groom-ing, or toileting due to restricted
mobility
·
Impaired skin integrity
related to lacerations and abrasions
·
Risk for peripheral
neurovascular dysfunction related to phys-iologic responses to injury and
compression effect of cast
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications
that may develop include the following:
·
Compartment syndrome
·
Pressure ulcer
·
Disuse syndrome
Planning and Goals
The major goals for the patient with a cast include
knowledge of the treatment regimen, relief of pain, improved physical
mobil-ity, achievement of maximum level of self-care, healing of lacer-ations
and abrasions, maintenance of adequate neurovascular function, and absence of
complications.
Nursing Interventions
EXPLAINING THE TREATMENT REGIMEN
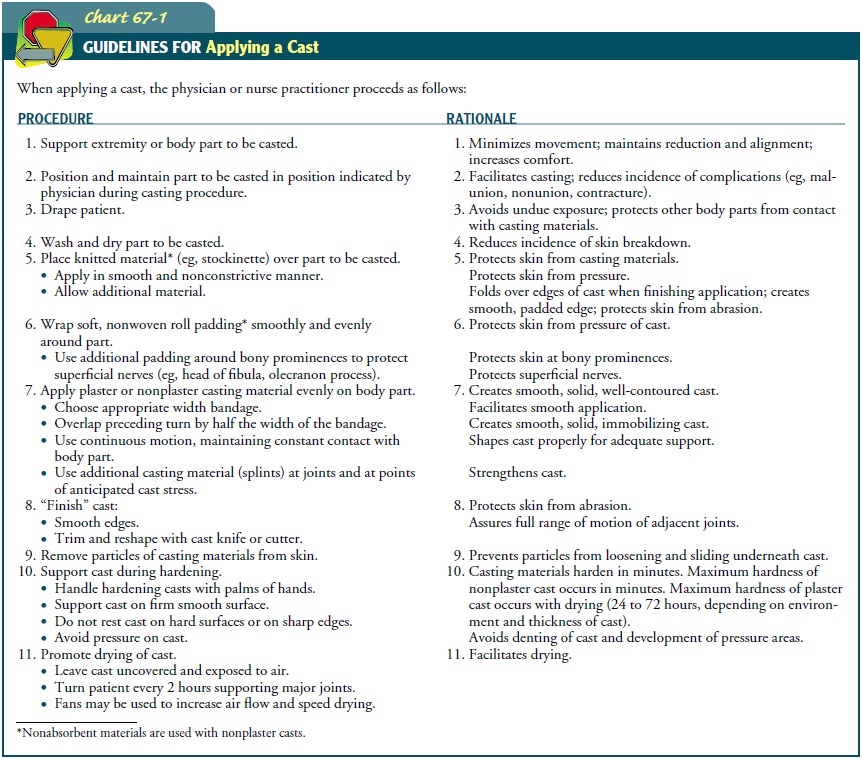
Before the cast is applied, the patient needs information
con-cerning the pathologic problem and the purpose and expectations of the
prescribed treatment regimen. This knowledge promotes the patient’s active
participation in and adherence to the treat-ment program. It is important to
prepare the patient for the ap-plication of the cast by describing the
anticipated sights, sounds, and sensations (eg, heat from the hardening
reaction of the plaster). The patient needs to know what to expect during
appli-cation and that the body part will be immobilized after casting (Chart
67-1).
RELIEVING PAIN
The nurse must carefully evaluate pain associated with muscu-loskeletal problems, asking the patient to indicate the exact site and to describe the character and intensity of the pain to help de-termine its cause. Most pain can be relieved by elevating the in-volved part, applying cold as prescribed, and administering usual dosages of analgesics.
Pain associated with the disease process (eg, fracture)
is fre-quently controlled by immobilization. Pain due to edema that is associated with trauma, surgery, or bleeding into the
tissues can frequently be controlled by elevation and, if prescribed,
inter-mittent application of cold. Ice bags (one-third to one-half full) or
cold application devices are placed on each side of the cast, if prescribed,
making sure not to indent the cast.
Pain may be indicative of complications. Pain associated
with compartment syndrome is relentless and is not controlled by modalities such
as elevation, application of cold if prescribed, and usual dosages of
analgesics. Severe pain over a bony prominence warns of an impending pressure
ulcer. Pain decreases when ul-ceration occurs. Discomfort due to pressure on
the skin may be relieved by elevation that controls edema or by positioning
that alters pressure. It may be necessary, however, to modify the cast or to
apply a new cast.
IMPROVING MOBILITY
Every joint that is not immobilized should be exercised
and moved through its range of motion to maintain function. If the patient has
a leg cast, the nurse encourages toe exercises. If the pa-tient has an arm
cast, the nurse encourages finger exercises.
PROMOTING HEALING OF SKIN ABRASIONS
Before the cast is
applied, it is important to treat skin lacerations and abrasions to promote
healing. The nurse thoroughly cleans the skin and treats it as prescribed.
Sterile dressings are used to cover the injured skin. If the skin wounds are
extensive, an alternative method (eg, external fixator) may be chosen to
immobilize the body part. While the cast is on, the nurse observes the patient
for systemic signs of infection, odors from the cast, and purulent drainage
staining the cast. It is important to notify the physician if any of these
occurs.
MAINTAINING ADEQUATE NEUROVASCULAR FUNCTION
Swelling and edema are natural responses of the
tissue to trauma and surgery. The patient may complain that the cast is too
tight. Vascular insufficiency and nerve compression due to unrelieved swelling
can result in compartment syndrome. The nurse monitors circulation, motion, and
sensation of the affected extremity, assessing the fingers or toes of the
casted extremity and comparing them with those of the opposite extremity.
Normal findings include minimal swelling, minimal discomfort, pink color, warm
to touch, rapid capillary refill response, normal sen-sations, and ability to
exercise fingers or toes. The nurse encour-ages the patient to move fingers or
toes hourly when awake to stimulate circulation.
It is important to
perform frequent, regular assessments of neurovascular status. Early
recognition of diminished circulation and nerve function is essential to
prevent loss of function. As-sessment data including progressive unrelieved
pain, pain on passive stretch, paresthesia, motor loss, sensory loss, coolness,
paleness, slow capillary refill, and sensation of tightness indicate potential
compartment syndrome. The nurse adjusts the extrem-ity so that it is no higher
than heart level to enhance arterial per-fusion and control edema and notifies
the physician at once.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Compartment Syndrome
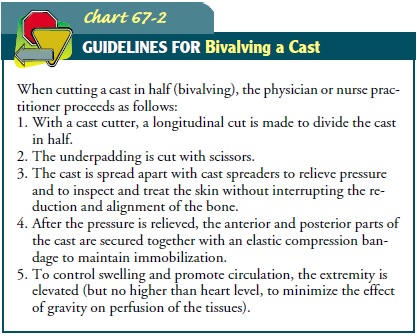
Compartment syndrome
occurs when there is increased tissue pressure within a limited space (eg,
cast, muscle compartment) that compromises the circulation and the function of
the tissue within the confined area. To relieve the pressure, the cast must be
bivalved (cut in half longitudinally) while maintaining align-ment, and the
extremity must be elevated no higher than heart level (Chart 67-2). If pressure
is not relieved and circulation is not restored, a fasciotomy may be necessary to relieve the pressure within the
muscle compartment. The nurse closely monitors the patient’s response to
conservative and surgical management of compartment syndrome. The nurse records
neurovascular re-sponses and promptly reports changes to the physician.
Pressure Ulcers
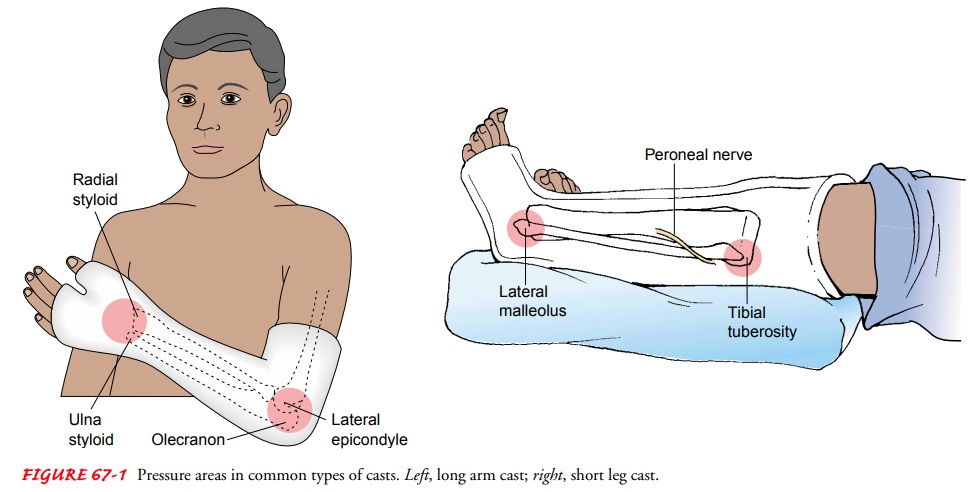
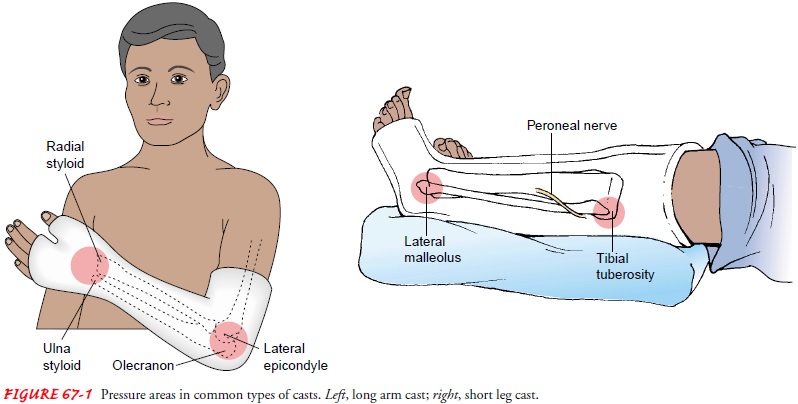
Pressure of the cast on soft tissues may cause tissue anoxia and pressure ulcers. Lower extremity sites most susceptible to pressure are the heel, malleoli, dorsum of the foot, head of the fibula, and anterior surface of the patella. The main pressure sites on the upper extremity are located at the medial epicondyle of the humerus and the ulnar styloid (see Fig. 67-1).
Usually, the patient
with a pressure ulcer reports pain and tightness in the area. A warm area on
the cast suggests underly-ing tissue erythema. The area may break down. The
drainage may stain the cast and emit an odor. Even if discomfort does not occur
with tissue breakdown and necrosis, there may still be extensive loss of
tissue. The nurse must monitor the patient with a cast for pressure ulcer
development and report findings to the physician.
To inspect the pressure area, the physician may bivalve
the cast or cut an opening (window) in the cast. If the physician elects to
create a window to inspect the pressure site, a portion of the cast is cut out.
The affected area is inspected and possibly treated. The portion of the cast is
replaced and held in place by an elastic com-pression dressing or tape. This
prevents the underlying tissue from swelling through the window and creating
pressure areas around its margins.
Disuse Syndrome
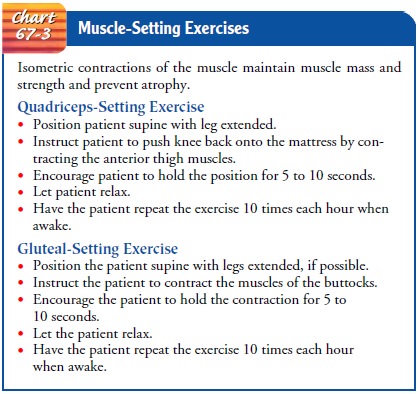
While in a cast, the patient needs to learn to tense or
contract muscles (eg, isometric muscle contraction) without moving the part.
This helps to reduce muscle atrophy and maintain muscle strength. The nurse
teaches the patient with a leg cast to “push down” the knee and teaches the
patient in an arm cast to “make a fist.” Muscle-setting exercises (eg,
quadriceps-setting and gluteal-setting exercises) are important in maintaining
muscles essential for walking (Chart 67-3). Isometric exercises should be
performed hourly while the patient is awake.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching the Patient Self-Care
Self-care deficits occur when a portion of the body is immobi-lized. The nurse encourages the patient to participate actively in personal care and to use assistive devices safely. The nurse must assist the patient in identifying areas of self-care deficit and in developing strategies to achieve independence in activities of daily living (ADLs) (Chart 67-4). The patient’s participation in planning and accomplishing ADLs is an important aspect of self-care, independence, maintaining control, and avoiding untoward psychological reactions, such as depression.
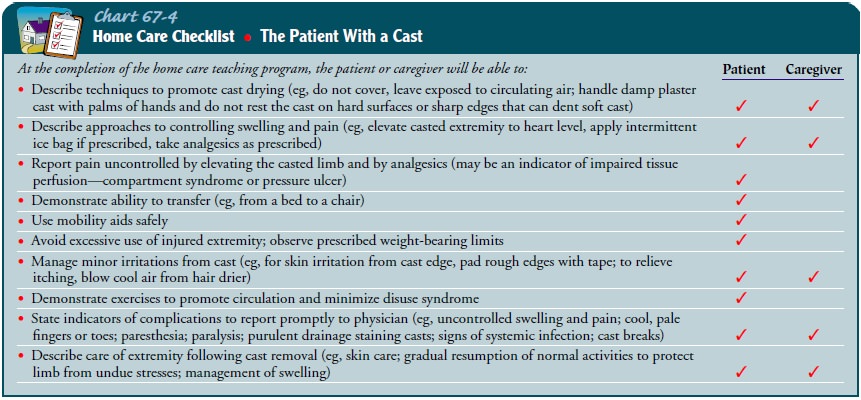
When the cast is dry, the nurse instructs the patient as
follows:
·
Move about as normally as
possible, but avoid excessive use of the injured extremity and avoid walking on
wet, slippery floors or sidewalks.
·
Perform prescribed exercises
regularly, as scheduled.
·
Elevate the casted extremity
to heart level frequently to pre-vent swelling.
·
Do not attempt to scratch the
skin under the cast. This may cause a break in the skin and result in the
formation of a skin ulcer. Cool air from a hair dryer may alleviate an itch.
·
Cushion rough edges of the
cast with tape.
·
Keep the cast dry but do not
cover it with plastic or rubber, because this causes condensation, which
dampens the cast and skin. Moisture softens a plaster cast. (A wet fiberglass
cast must be dried thoroughly with a hair dryer on a cool setting to avoid skin
problems.)
·
Report any of the following to
the physician: persistent pain, swelling that does not respond to elevation,
changes in sensation, decreased ability to move exposed fingers or toes, and
changes in skin color and temperature.
·
Note odors around the cast,
stained areas, warm spots, and pressure areas. Report them to the physician.
·
Report a broken cast to the
physician; do not attempt to fix it yourself.
The nurse prepares the patient for cast removal or cast
changes by explaining what to expect (Chart 67-5). The cast is cut with a cast
cutter, which vibrates. The patient can feel the vibration and pressure during
its use. The cutter does not penetrate deeply enough to hurt the patient’s
skin. The cast padding is cut with scissors.
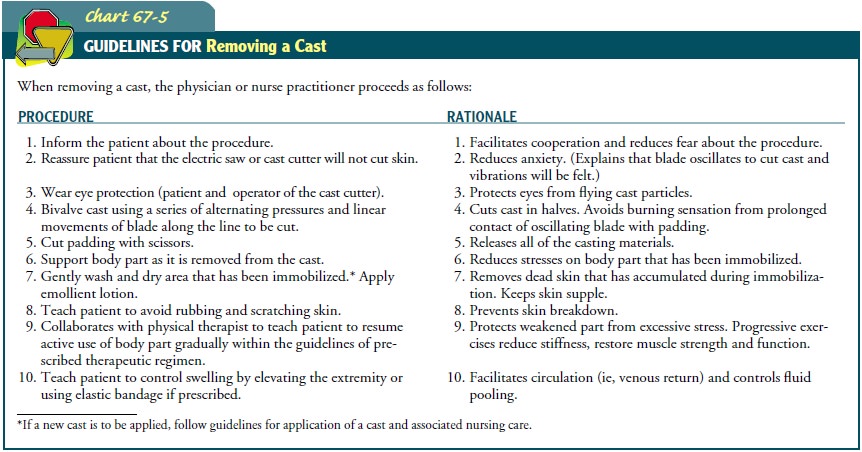
The casted body part is weak from disuse, is stiff, and
may ap-pear atrophied. There may be extreme stiffness even after only a few
weeks of immobilization. Therefore, support is needed when the cast is removed.
The skin, which is usually dry and scaly from accumulated dead skin, is
vulnerable to injury from scratching.
The skin needs to be washed gently and lubricated with an
emol-lient lotion.
The nurse and physical therapist teach the patient to
resume activities gradually within the prescribed therapeutic regimen.
Exercises that are prescribed to help the patient regain joint motion are
explained and demonstrated. Because the muscles are weak from disuse, the body
part that has been casted cannot withstand normal stresses immediately. In
addition, the nurse teaches the patient who has noticeable swelling of the affected
extremity after the cast is removed to continue to elevate the ex-tremity to
control swelling until normal muscle tone and use are reestablished.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Understands
the therapeutic regimen
a) Elevates
affected extremity
b) Exercises
according to instructions
c) Keeps
cast dry
d) Reports
any problems that develop
e) Keeps
follow-up clinic or physician appointments
2) Reports
less pain
a) Elevates
extremity that is in the cast
b) Repositions
self
c) Uses
occasional oral analgesic
3) Demonstrates
increased mobility
a) Uses
assistive devices safely
b) Exercises
to increase strength
c) Changes
position frequently
d) Performs
range-of-motion exercises of joints not in the cast
4) Exhibits
healing of abrasions and lacerations
a) Demonstrates
no local signs of infection (ie, local dis-comfort, purulent drainage, cast
staining, or odor from cast)
b) Demonstrates
no systemic signs or symptoms of infection
c) Demonstrates intact skin when cast is removed
5) Maintains
adequate neurovascular function of affected extremity
a) Exhibits
normal skin color and temperature
b) Experiences
minimal swelling
c) Exhibits
satisfactory capillary refill on testing
d) Demonstrates
active movement of fingers or toes if they are not casted
e) Reports
normal sensations in casted body part
f) Reports
that pain is controllable
6) Exhibits
absence of complications
a) Demonstrates
normal neurovascular status of casted extremity
b) Develops
no pressure ulcers
c) Exhibits
minimal muscle wasting
7) Participates
in self-care activities
a) Performs
hygiene and grooming activities indepen-dently or with minimal assistance
b) Performs
ADLs independently or with minimal assistance
c) Adheres
to prescribed exercise regimen.
Related Topics