Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Joint Replacement - Managing the Patient Undergoing Orthopedic Surgery
JOINT REPLACEMENT
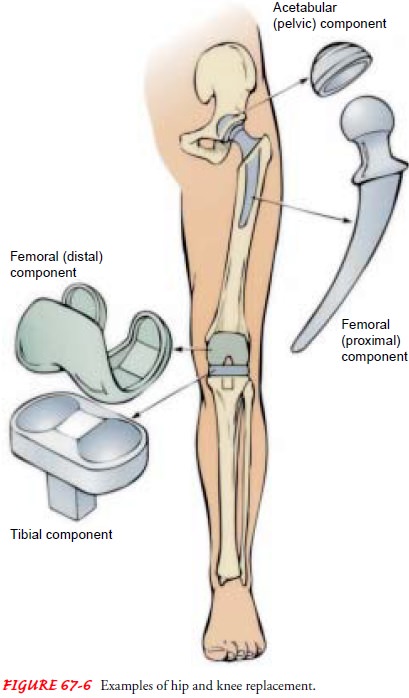
Patients with severe joint pain and disability may undergo joint replacement. Conditions contributing to joint degeneration in-clude osteoarthritis (degenerative joint disease), rheumatoid arthritis, trauma, and congenital deformity. Some fractures (eg, femoral neck fracture) may cause disruption of the blood supply and subsequent avascular necrosis; management with joint re-placement may be elected over ORIF. Joints frequently replaced include the hip, knee (Fig. 67-6), and finger joints. Less frequently, more complex joints (shoulder, elbow, wrist, ankle) are replaced. The procedure is usually an elective one.
Most joint replacements
consist of metal and high-density polyethylene components. Finger prostheses
are usually Silastic. The joint implants may be cemented in the prepared bone
with polymethyl methacrylate (PMMA), a bone-bonding agent that has properties
similar to bone. Loosening of the prosthesis due to cement–bone interface
failure is a common reason for prosthesis failure. Press-fit, ingrowth
prostheses (porous-coated, cementless artificial joint components) that allow
the patient’s bone to grow into and securely fix the prosthesis in the bone are
alternatives to cemented prostheses. Accurate fitting and the presence of
healthy bone with adequate blood supply are important in the use of ce-mentless
components. Much progress has been made in reducing prosthesis failure rate
through improved techniques, improved materials, and use of bone grafts.
With joint replacement,
excellent pain relief is obtained in most patients. Return of motion and
function depends on pre-operative soft tissue condition, soft tissue reactions,
and general muscle strength. Early failure of joint replacement is associated
with excessive activity and preoperative joint and bone pathology.
Nursing Interventions
Assessment of the
patient and preoperative management are aimed at having the patient in optimal
health at the time of surgery. Pre-operatively, it is important to evaluate
cardiovascular, respiratory, renal, and hepatic functions. Age, obesity,
preoperative leg edema, history of DVT, and varicose veins increase the risk of
post-operative DVT and pulmonary embolism. These are the most com-mon causes of
postoperative mortality for patients older than 60 years of age undergoing
total hip replacement. Every effort is made to prevent these complications.
Preoperatively, it is
important to assess the neurovascular sta-tus of the extremity undergoing joint
replacement. Postoperative assessment data are compared with preoperative
assessment data to identify changes and deficits. For example, an absent pulse
postoperatively is of concern unless the pulse was also absent pre-operatively.
Nerve palsy could occur as a result of surgery.
PREVENTING INFECTION
Preoperative assessment
of the patient for infections, including urinary tract infection, is necessary
because of the risk of post-operative infection. Any infection 2 to 4 weeks
before planned surgery may result in postponement of surgery. Preoperative skin
preparation frequently begins 1 or 2 days before the surgery. Air-borne
bacteria that contaminate the wound at the time of surgery cause most deep
infections. Therefore, as with any surgery, there is strict adherence to
aseptic principles and the operating area is controlled and made as bacteria
free as possible.
Prophylactic antibiotics are administered perioperatively
as a single preoperative or short perioperative course (Rosen et al., 1999).
Culture of the joint during surgery, before intraoperative antibiotic therapy
is begun, may be important in identifying and treating subsequent infections.
If osteomyelitis develops, it is difficult to treat.
Persistent in-fection at the site of the prosthesis usually requires removal of
the implant and joint revision, which is a complex procedure. Also, it is not
always possible to achieve a functional joint when the re-construction
procedure has to be repeated.
PROMOTING AMBULATION
Patients with total hip
or total knee replacement begin ambu-lation with a walker or crutches within a
day after surgery. The nurse and the physical therapist assist the patient in
achieving the goal of independent ambulation. At first, the patient may only be
able to stand for a brief period because of orthostatic hypoten-sion. Specific
weight-bearing limits on the prosthesis are deter-mined by the physician and
are based on the patient’s condition, the procedure, and the fixation method.
Usually, patients with cemented prostheses can proceed to weight bearing as
tolerated. If the patient has a press-fit, cementless, ingrowth prosthesis,
weight bearing immediately after surgery may be limited to min-imize
micromotion of the prosthesis in the bone. As the patient is able tolerate more
activity, the nurse encourages transferring to a chair several times a day for
short periods and walking for pro-gressively greater distances.
Related Topics