Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Skin Traction
SKIN TRACTION
Skin traction is used to control muscle spasms and to immobilize an area before surgery. Skin traction is accomplished by using a weight to pull on traction tape or on a foam boot attached to the skin. The amount of weight applied must not exceed the tolerance of the skin. No more than 2 to 3.5 kg (4.5 to 8 lb) of trac-tion can be used on an extremity. Pelvic traction is usually 4.5 to 9 kg (10 to 20 lb), depending on the weight of the patient.
Types of skin traction used for adults include Buck’s
extension traction (applied to the lower leg), the cervical head halter
(occa-sionally used to treat neck pain), and the pelvic belt (sometimes used to
treat back pain).
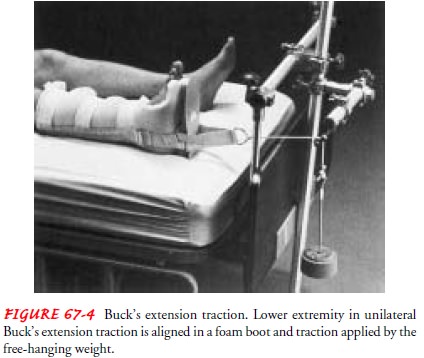
Buck’s Extension Traction
Buck’s extension traction (unilateral or bilateral) is
skin traction to the lower leg. The pull is exerted in one plane when partial
or temporary immobilization is desired (see Fig. 67-4). It is used to provide
immobility after fractures of the proximal femur before surgical fixation.
Before the traction is applied, the nurse inspects the
skin for abrasions and circulatory disturbances. The skin and circulation must
be in healthy condition to tolerate the traction. The ex-tremity should be
clean and dry before the foam boot or traction tape is applied.
To apply Buck’s traction, one nurse elevates and supports
the extremity under the patient’s heel and knee while another nurseplaces the
foam boot under the leg, with the patient’s heel in the heel of the boot. Next,
the nurse secures Velcro straps around the leg. Traction tape overwrapped with
elastic bandage in a spi-ral fashion may be used instead of the boot. Excessive
pressure is avoided over the malleolus and proximal fibula during applica-tion
to prevent pressure ulcers and nerve damage. The nurse then passes the rope
affixed to the spreader or footplate over a pulley fastened to the end of the
bed and attaches the weight—usually 5 to 8 pounds—to the rope.
Potential Complications
Skin breakdown, nerve
pressure, and circulatory impairment are complications that may develop as a
result of skin traction. Skin breakdown results from irritation caused by
contact of the skin with the tape or foam and shearing forces. Older adults are
at greater risk for this complication because of their sensitive, fragile skin.
Nerve pressure results
from pressure on the peripheral nerves. Footdrop may occur if pressure is
applied to the peroneal nerve at the point at which it passes around the neck
of the fibula just below the knee.
Circulatory impairment
is manifested by cold skin tempera-ture, decreased peripheral pulses, slow
capillary refill time, and bluish skin. Deep vein thrombosis (DVT), a serious
circulatory impairment, is manifested by calf tenderness, swelling, and a
pos-itive Homans’ sign.
Nursing Interventions
ENSURING EFFECTIVE TRACTION
To ensure effective skin
traction, it is important to avoid wrinkling and slipping of the traction
bandage and to maintain counter-traction. Proper positioning must be maintained
to keep the leg in a neutral position. To prevent bony fragments from moving
against one another, the patient should not turn from side to side; however,
the patient may shift position slightly with assistance.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Skin Breakdown.
During the initial assessment, the nurse iden-tifies sensitive, fragile skin (common in older adults). The nurse also closely monitors the reaction of the skin in contact with tape or foam to ensure that shearing forces are avoided. The nurse performs the following procedures to monitor and prevent skin breakdown:
·
Removes the foam boots to
inspect the skin, the ankle, and the Achilles tendon three times a day. A
second nurse is needed to support the extremity during the inspection and skin
care.
·
Palpates the area of the
traction tapes daily to detect under-lying tenderness.
·
Provides back care at least
every 2 hours to prevent pressure ulcers. The patient who must remain in a
supine position is at increased risk for development of a pressure ulcer.
·
Uses special mattress overlays
(eg, air-filled, high-density foam) to minimize the development of skin ulcers.
Nerve Pressure.
Skin traction can place
pressure on peripheralnerves. When traction is applied to the lower extremity,
care must be taken to avoid pressure on the peroneal nerve at the point at
which it passes around the neck of the fibula just below the knee. Pressure at
this point can cause footdrop. The nurse questions the patient about sensation
and asks the patient to move the toes and foot. Dorsiflexion of the foot
demonstrates function of the pero-neal nerve. Weakness of dorsiflexion or foot
movement and in-version of the foot might indicate pressure on the common
peroneal nerve. Plantar flexion demonstrates function of the tib-ial nerve.
The following are important points to keep in mind when
car-ing for the patient in traction:
·
Regularly assess sensation and
motion.
·
Immediately investigate any
complaint of burning sensation under the traction bandage or boot.
·
Promptly report altered
sensation or motor function.
Circulatory Impairment.
After skin traction is
applied, the nurseassesses circulation of the foot or hand within 15 to 30
minutes and then every 1 to 2 hours. Circulatory assessment consists of the
following:
·
Peripheral pulses, color,
capillary refill, and temperature of the fingers or toes
·
Indicators of DVT, including
calf tenderness, swelling, and a positive Homans’ sign
The nurse also encourages the patient to perform active
foot exercises every hour when awake.
Related Topics