Chapter: Medical Surgical Nursing: Musculoskeletal Care Modalities
Skeletal Traction
SKELETAL TRACTION
Skeletal traction is applied directly to the bone. This
method of traction is used occasionally to treat fractures of the femur, the
tibia, and the cervical spine. The traction is applied directly to the bone by
use of a metal pin or wire (eg, Steinmann pin, Kirschner wire) that is inserted
through the bone distal to the fracture, avoiding nerves, blood vessels,
muscles, tendons, and joints. Tongs applied to the head (eg, Gardner-Wells or
Vinke tongs) are fixed in the skull to apply traction that immobilizes cervical
fractures.
The orthopedic surgeon applies skeletal traction, using
surgi-cal asepsis. The insertion site is prepared with a surgical scrub agent
such as povidone-iodine solution. A local anesthetic is ad-ministered at the
insertion site and periosteum. The surgeon makes a small skin incision and
drills the sterile pin or wire through the bone. The patient feels pressure during
this proce-dure and possibly some pain when the periosteum is penetrated.
After insertion, the pin or wire is attached to the
traction bow or caliper. The ends of the wire are covered with corks or tape to
prevent injury to the patient or caregivers. The weights are at-tached to the
pin or wire bow by a rope-and-pulley system that exerts the appropriate amount
and direction of pull for effective traction. Skeletal traction frequently uses
7 to 12 kg (15 to 25 lb) to achieve the therapeutic effect. The weights applied
initially must overcome the shortening spasms of the affected muscles. As the
muscles relax, the traction weight is reduced to prevent frac-ture dislocation
and to promote healing.
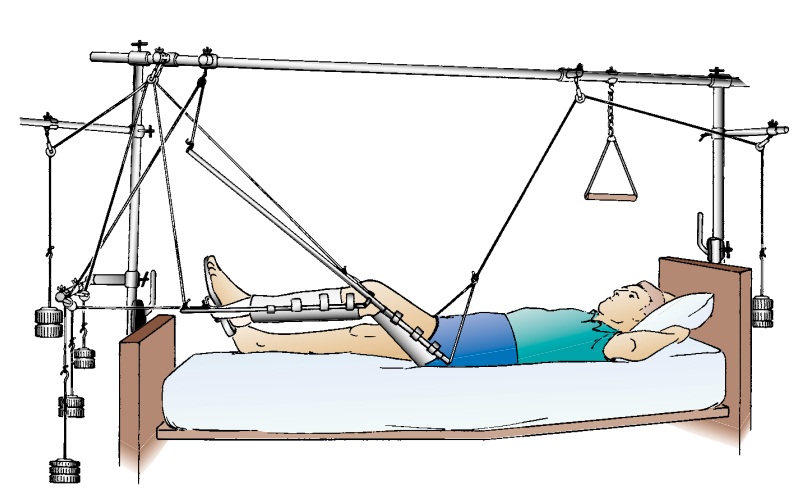
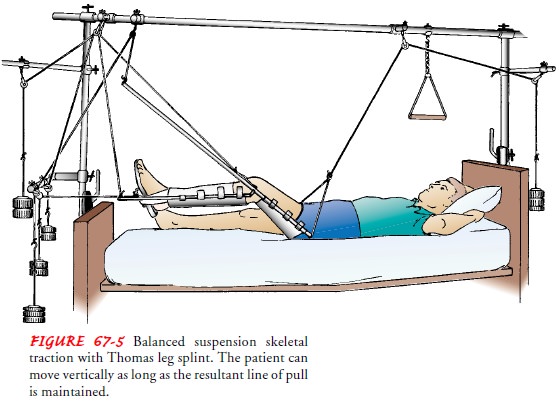
Often, skeletal traction is balanced traction, which supports
the affected extremity, allows for some patient movement, and facili-tates
patient independence and nursing care while maintaining ef-fective traction.
The Thomas splint with a Pearson attachment is frequently used with skeletal
traction for fractures of the femur (see Fig. 67-5). Because upward traction is
required, an overbed frame is used.
When skeletal traction
is discontinued, the extremity is gently supported while the weights are
removed. The pin is cut close to the skin and removed by the physician.
Internal fixation, casts, or splints are then used to immobilize and support
the healing bone.
Nursing Interventions
MAINTAINING EFFECTIVE TRACTION
When skeletal traction
is used, the nurse checks the apparatus to see that the ropes are in the wheel
grooves of the pulleys, that the ropes are not frayed, that the weights hang
free, and that the knots in the rope are tied securely. The nurse also
evaluates the patient’s position, because slipping down in bed results in
in-effective traction.
MAINTAINING POSITIONING
The nurse must maintain
alignment of the patient’s body in trac-tion as prescribed to promote an
effective line of pull. The nurse positions the patient’s foot to avoid
footdrop (plantar flexion), in-ward rotation (inversion), and outward rotation
(eversion). The patient’s foot may be supported in a neutral position by
ortho-pedic devices (eg, foot supports).
PREVENTING SKIN BREAKDOWN
The patient’s elbows frequently become sore, and nerve
injury may occur if the patient repositions by pushing on the elbows. In
addition, patients frequently push on the heel of the unaffected leg when they
raise themselves. This digging of the heel into the mattress may injure the
tissues. Therefore, the nurse should pro-tect the elbows and heels and inspect
them for pressure areas. To encourage movement without using the elbows or
heel, the nurse can suspend a trapeze overhead within easy reach of the
patient. This apparatus helps the patient to move about in bed and to move on
and off the bedpan.
Specific pressure points
are assessed for redness and skin break-down. Areas that are particularly
vulnerable to pressure caused by traction apparatus applied to the lower
extremity include the ischial tuberosity, popliteal space, Achilles tendon, and
heel. If the patient is not permitted to turn on one side or the other, the
nurse must make a special effort to provide back care and to keep the bed dry
and free of crumbs and wrinkles. The patient can as-sist by holding the
overhead trapeze and raising the hips off the bed. If the patient cannot do
this, the nurse can push down on the mattress with one hand to relieve pressure
on the back and bony prominences and to provide for some shifting of weight. A
pressure-relieving air-filled or high-density foam mattress overlay may re-duce
the risk of pressure ulcer.
For change of bed linens, the patient raises the torso
while nurses on both sides of the bed roll down and replace the upper mattress
sheet. Then, as the patient raises the buttocks off the mattress, the nurses
slide the sheets under the buttocks. Finally, the nurses replace the lower
section of the bed linens while the patient rests on the back. Sheets and
blankets are placed over the patient in such a way that the traction is not
disrupted.
MONITORING NEUROVASCULAR STATUS
The nurse assesses the
neurovascular status of the immobilized ex-tremity at least every hour
initially and then every 4 hours. The nurse instructs the patient to report any
changes in sensation or movement immediately so that they can be promptly
evaluated. DVT is a significant risk for the immobilized patient. The nurse
en-courages the patient to do active flexion–extension ankle exercises and
isometric contraction of the calf muscles (calf-pumping exer-cises) 10 times an
hour while awake to decrease venous stasis. In ad-dition, elastic stockings,
compression devices, and anticoagulant therapy may be prescribed to help
prevent thrombus formation.
Prompt recognition of a developing neurovascular problem
is essential so that corrective measures can be instituted promptly.
PROVIDING PIN SITE CARE
The wound at the pin insertion site requires attention.
The goal is to avoid infection and development of osteomyelitis. Initially, the site is covered with a sterile
dressing. Subsequent care of the pin site is individually prescribed and
performed three times a day. The nurse must keep the area clean. Slight serous
oozing at the pin site is expected, but crusting should be prevented. The nurse
assesses the pin site and drainage for signs of infection, such as redness,
tenderness, and purulent drainage. The patient may experience discomfort at the
pin site due to traction on the skin caused by an unsupported muscle.
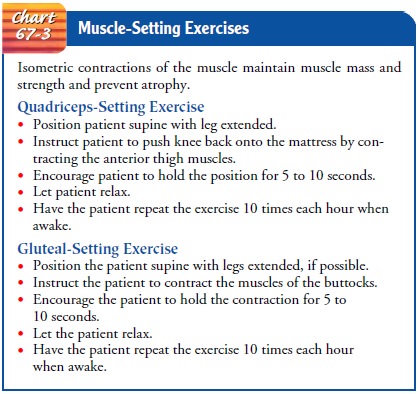
PROMOTING EXERCISE
Patient exercises,
within the therapeutic limits of the traction, as-sist in maintaining muscle
strength and tone and in promoting cir-culation. Active exercises include
pulling up on the trapeze, flexing and extending the feet, and range-of-motion
and weight-resistance exercises for noninvolved joints. Isometric exercises of
the immo-bilized extremity (quadriceps-setting and gluteal-setting exercises)
are important for maintaining strength in major ambulatory mus-cles (see Chart
67-3). Without exercise, the patient will lose mus-cle mass and strength, and
rehabilitation will be greatly prolonged.
Related Topics